Rehabilitation in a bedded setting is estimated to be needed in 4% of 2019 novel Coronavirus (COVID-19) patients discharged from hospital, especially from Intensive Care Unit (ICU).1
Functional impairment of patients surviving the COVID-19 acute phase has been poorly described, and the only available information is provided by experts2 or inferred from patients with other clinical conditions (e.g., Acute Respiratory Failure-ARF).3 Two recent studies suggested that early, post-hospitalization rehabilitative interventions would be recommended.4,5
Aim of this study is to assess the clinical and functional presentation of post-acute COVID-19 patients at admission for inpatient rehabilitation. All consecutive COVID-19 patients admitted to undergo inpatient rehabilitation at Istituti Clinici Scientifici (ICS) Maugeri, Tradate, Italy between April 1st and July 31st were evaluated. The study was approved by the Central Ethical Committee of ICS Maugeri (CEC2279; March 12th, 2020) and patients signed the consent form. Healthcare operators were trained in personal protection measures.6 The following evaluations were performed: clinical examination (including vital signs and blood gas analysis) and anthropometric assessment. Dyspnoea and perceived health state were measured by Barthel Dyspnea Index (Bd) (total scores range from 0-best- to 100-worst-), and Euro Quality of Life (EuroQoL-VAS), respectively (total scores range from 0-worst- to 100-best-), whereas disability with Barthel Index (Bi) (total scores range from 0-worst- to 100-best-), and Short Physical Performance Battery (SPPB) (total score results from the sum of three scores: standing balance, walking, and standing from sitting position, with disability if <9−1/2: severe; 3/8 moderate-).7 Functional assessment with Medical Research Council Muscle (MRCm) strength test for quadriceps and biceps (≥4 normal) and respiratory muscles fatigue with Single Breath Counting (SBC) were also evaluated.
Exercise capacity was assessed with the 6-min walk test (6MWT) or One Minute Sit to Stand (1STS)8 (reference value of repetitions: 30–37/min in men and 27–34/min in women, aged 60–79 years). Data accounted for length of stay (LoS) before admission for pulmonary rehabilitation, previous treatment for ARF (Invasive Mechanical Ventilation (IMV), Non-Invasive mechanical Ventilation (NIV), and oxygen), comorbidities (Cumulative Illness Rating Scale (CIRS)) gender and age.
Qualitative and quantitative variables were described with absolute and relative (percentage) frequencies and means (standard deviations, SD) or medians (interquartile ranges, IQR), depending on their normal or non-normal distribution, respectively. Demographic, epidemiological, and clinical variables were compared, stratifying by ICU stay and gender. Chi-squared or Fisher exact test was used for qualitative variables; analysis of variance or Kruskall–Wallis was computed for quantitative variables with a normal or non-normal distribution, respectively. CIRS and LoS were correlated with key clinical variables (Spearman’s correlation) and were ranked according to the Chan’s classification. A p-value <0.05 was considered statistically significant.
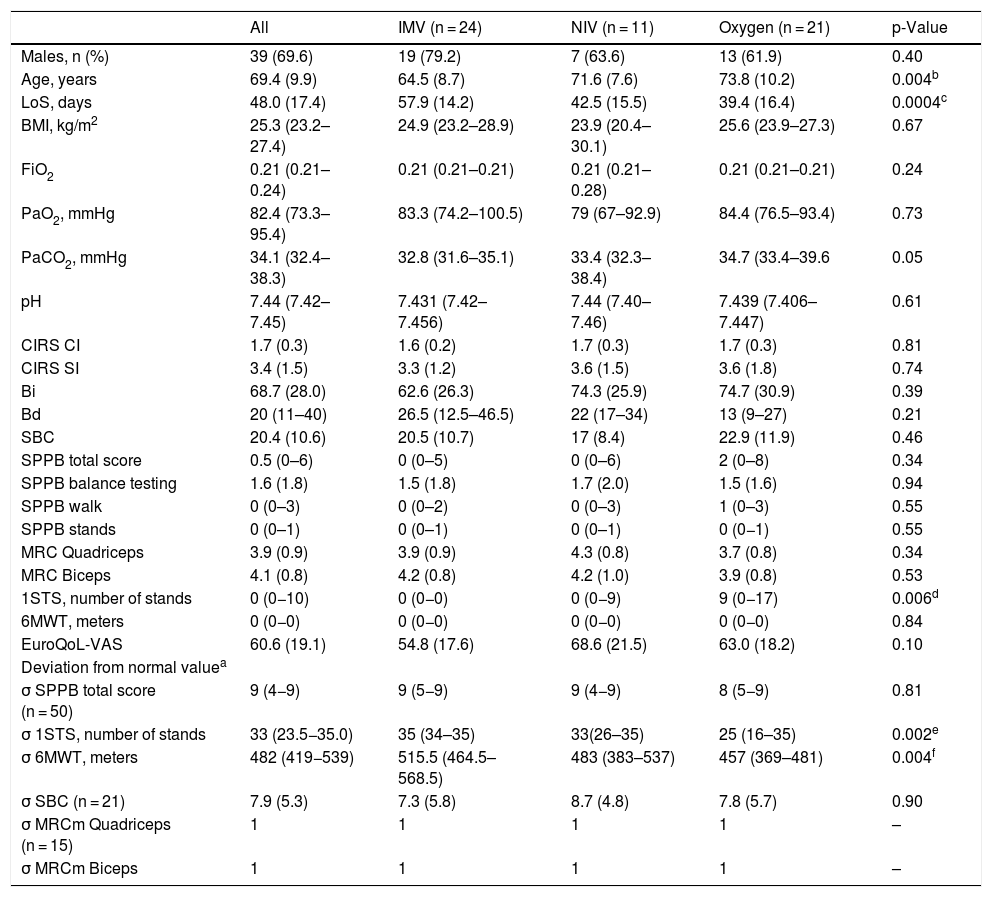
All 56 patients showed a reduced Bi and EuroQoL-VAS and increased Bd (Table 1). Overall 27/56 (48.2%) patients had a total SPPB score of 0, 22/56 (39.3%) between 1 and 8, and 7/56 (12,5%) ≥9. The SPBB ‘standing balance’ was less than 4 in 40 (71.4%) patients. Only 19/56 (33.9%) completed the 1STS test with a median (IQR) number of 14 (9.3–19.8) repetitions. The majority (53, 94.6%) could not perform the 6MWT and 5.4% covered a mean (SD) distance of 423.7 (34.8) m, around 70% of the Enright predicted value.
Baseline characteristics of 56 patients surviving the acute COVID-19 phase.
| All | IMV (n = 24) | NIV (n = 11) | Oxygen (n = 21) | p-Value | |
|---|---|---|---|---|---|
| Males, n (%) | 39 (69.6) | 19 (79.2) | 7 (63.6) | 13 (61.9) | 0.40 |
| Age, years | 69.4 (9.9) | 64.5 (8.7) | 71.6 (7.6) | 73.8 (10.2) | 0.004b |
| LoS, days | 48.0 (17.4) | 57.9 (14.2) | 42.5 (15.5) | 39.4 (16.4) | 0.0004c |
| BMI, kg/m2 | 25.3 (23.2–27.4) | 24.9 (23.2–28.9) | 23.9 (20.4–30.1) | 25.6 (23.9–27.3) | 0.67 |
| FiO2 | 0.21 (0.21–0.24) | 0.21 (0.21–0.21) | 0.21 (0.21–0.28) | 0.21 (0.21–0.21) | 0.24 |
| PaO2, mmHg | 82.4 (73.3–95.4) | 83.3 (74.2–100.5) | 79 (67–92.9) | 84.4 (76.5–93.4) | 0.73 |
| PaCO2, mmHg | 34.1 (32.4–38.3) | 32.8 (31.6–35.1) | 33.4 (32.3–38.4) | 34.7 (33.4–39.6 | 0.05 |
| pH | 7.44 (7.42–7.45) | 7.431 (7.42–7.456) | 7.44 (7.40–7.46) | 7.439 (7.406–7.447) | 0.61 |
| CIRS CI | 1.7 (0.3) | 1.6 (0.2) | 1.7 (0.3) | 1.7 (0.3) | 0.81 |
| CIRS SI | 3.4 (1.5) | 3.3 (1.2) | 3.6 (1.5) | 3.6 (1.8) | 0.74 |
| Bi | 68.7 (28.0) | 62.6 (26.3) | 74.3 (25.9) | 74.7 (30.9) | 0.39 |
| Bd | 20 (11–40) | 26.5 (12.5–46.5) | 22 (17–34) | 13 (9–27) | 0.21 |
| SBC | 20.4 (10.6) | 20.5 (10.7) | 17 (8.4) | 22.9 (11.9) | 0.46 |
| SPPB total score | 0.5 (0–6) | 0 (0–5) | 0 (0–6) | 2 (0–8) | 0.34 |
| SPPB balance testing | 1.6 (1.8) | 1.5 (1.8) | 1.7 (2.0) | 1.5 (1.6) | 0.94 |
| SPPB walk | 0 (0–3) | 0 (0–2) | 0 (0–3) | 1 (0–3) | 0.55 |
| SPPB stands | 0 (0–1) | 0 (0–1) | 0 (0–1) | 0 (0−1) | 0.55 |
| MRC Quadriceps | 3.9 (0.9) | 3.9 (0.9) | 4.3 (0.8) | 3.7 (0.8) | 0.34 |
| MRC Biceps | 4.1 (0.8) | 4.2 (0.8) | 4.2 (1.0) | 3.9 (0.8) | 0.53 |
| 1STS, number of stands | 0 (0−10) | 0 (0−0) | 0 (0−9) | 9 (0−17) | 0.006d |
| 6MWT, meters | 0 (0−0) | 0 (0−0) | 0 (0−0) | 0 (0−0) | 0.84 |
| EuroQoL-VAS | 60.6 (19.1) | 54.8 (17.6) | 68.6 (21.5) | 63.0 (18.2) | 0.10 |
| Deviation from normal valuea | |||||
| σ SPPB total score (n = 50) | 9 (4−9) | 9 (5−9) | 9 (4−9) | 8 (5−9) | 0.81 |
| σ 1STS, number of stands | 33 (23.5−35.0) | 35 (34–35) | 33(26–35) | 25 (16–35) | 0.002e |
| σ 6MWT, meters | 482 (419−539) | 515.5 (464.5–568.5) | 483 (383–537) | 457 (369–481) | 0.004f |
| σ SBC (n = 21) | 7.9 (5.3) | 7.3 (5.8) | 8.7 (4.8) | 7.8 (5.7) | 0.90 |
| σ MRCm Quadriceps (n = 15) | 1 | 1 | 1 | 1 | – |
| σ MRCm Biceps | 1 | 1 | 1 | 1 | – |
Value are expressed as number, mean or median SD or IQR.
Legend: IMV: Invasive Mechanical Ventilation; NIV: Non Invasive Mechanical Ventilation; LoS: length of stay; BMI: body mass index; FiO2: fraction of inspired oxygen; PaO2: partial pressure of oxygen; PaCO2: partial pressure of carbon dioxide; CIRS: Cumulative Illness Rating Scale including the comorbidity index (CI) and the severity index (SI); Bi: Barthel of activity of daily life; Bd: Bathel dyspnoea; SBC: Single Breath Counting; SPPB: Short Physical Performance Battery; MRCm: Medical Research Council Muscular; 1STS: One Minute Sit to Stand; 6MWT: six minute walk test; EuroQoL-VAS: Euro Quality of Life with visual analogue scale. Sidak and Bonferroni multiple comparison tests were performed.
No statistically significant differences were found for clinical and functional data between males and females.
Patients previously treated with IMV were younger (p-value: 0.004), experienced a longer LoS (p-value: 0.0004), and had worse 1STS (p-value: 0.006) when compared with patients previously treated with oxygen (Table 2).
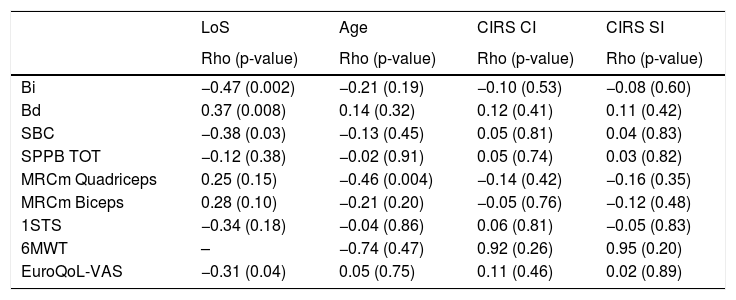
Correlations between LoS, age, CIRS and impairment outcomes.
| LoS | Age | CIRS CI | CIRS SI | |
|---|---|---|---|---|
| Rho (p-value) | Rho (p-value) | Rho (p-value) | Rho (p-value) | |
| Bi | −0.47 (0.002) | −0.21 (0.19) | −0.10 (0.53) | −0.08 (0.60) |
| Bd | 0.37 (0.008) | 0.14 (0.32) | 0.12 (0.41) | 0.11 (0.42) |
| SBC | −0.38 (0.03) | −0.13 (0.45) | 0.05 (0.81) | 0.04 (0.83) |
| SPPB TOT | −0.12 (0.38) | −0.02 (0.91) | 0.05 (0.74) | 0.03 (0.82) |
| MRCm Quadriceps | 0.25 (0.15) | −0.46 (0.004) | −0.14 (0.42) | −0.16 (0.35) |
| MRCm Biceps | 0.28 (0.10) | −0.21 (0.20) | −0.05 (0.76) | −0.12 (0.48) |
| 1STS | −0.34 (0.18) | −0.04 (0.86) | 0.06 (0.81) | −0.05 (0.83) |
| 6MWT | – | −0.74 (0.47) | 0.92 (0.26) | 0.95 (0.20) |
| EuroQoL-VAS | −0.31 (0.04) | 0.05 (0.75) | 0.11 (0.46) | 0.02 (0.89) |
Legend: LoS: length of stay; CIRS: Cumulative Illness Rating Scale including the comorbidity index (CI) and the severity index (SI); Bi: Barthel of activity of daily life; Bd: Bathel dyspnoea; SBC: Single Breath Counting; SPPB: Short Physical Performance Battery; MRCm: Medical Research Council Muscular; 1STS: One Minute Sit to Stand; 6MWT: six minute walk test; EuroQoL-VAS: Euro Quality of Life with visual analogue scale.
Furthermore, a statistically significant fair correlation was found between LoS and Bi, Bd, SBC and EuroQoL-VAS and between age and MRC quadriceps oriented to a worse functional and symptomatic status.
The results of the present study show that COVID-19 survivors can have an impairment of functional and muscular performance, dyspnoea, as well as impaired perceived health state. Patients who underwent IMV were younger, had a longer LoS and could not perform any exercise test.
Our patients, without acute respiratory failure, showed more clinical complications (i.e., reduced ability to carry out daily living activities and moderate dyspnoea, even at rest) when compared with another cohort, which included respiratory failure survivors with an average SPBB < 4.9
Our findings are consistent with those of recent studies,4,5 where post-acute COVID-19 patients suffer from dyspnoeaand severe disability. Although information about fatigue is missing in our study; a recent review underlined this as an important outcome in pulmonary rehabilitation.10 These data support the rationale for pulmonary rehabilitation, being effective in reducing dyspnea and fatigue, improving exercise capacity and quality of life.
In conclusion, our preliminary data suggest indication for previously hospitalized COVID-19 patients to undergo a comprehensive clinical and functional assessment to identify those who are likely to benefit from rehabilitation. However, future studies in this field are also needed about potential effects of pulmonary rehabilitation.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors wish to thank all staff (nurses, physiotherapists, physicians) of the Pulmonary Rehabilitation department Istituti Clinici Scientifici Maugeri, Tradate, who make this study possible.