Patients with Chronic Obstructive Pulmonary Disease (COPD) present musculoskeletal disorders, which result in exercise intolerance, a decline in quality of life (QoL)1 and poor sleep quality2. It is proven that the use of elastic tools in resistance training for patients with COPD is beneficial in improving the functional capacity, QoL and muscle strength3,4. However, it is unknown if the benefits achieved with elastic resistance training using elastic bands and tubes, are maintained after the program, in COPD. Considering the advantages (low cost and portability) of these elastic tools, as well as the benefits for these patients3, it is necessary to evaluate the functionality, health status, and body composition at the end of the training program.
The objective of this study was to analyze functional capacity, body composition, QoL and Physical Activity (PA) level at 3 months follow-up after 12 weeks of elastic resistance training in patients with COPD.
METHODSSampleThe sample size was defined using the study of Ramos et al. (2014)3. In order to evaluate the study parameters a six-minute walk test (6MWT) was carried out by 54 patients divided into three groups. The duration of the study lasted 24 weeks (12 weeks of training and 12 weeks of follow-up). Participants signed the consent form. All the procedures performed were approved by the Research Ethics Committee (approval number of the Ethics Committee: 1.677.874).
Study designA total of 81 patients diagnosed with COPD were recruited. Of these, 48 patients were randomized into three groups: Elastic Band Training Group (EBG), Elastic Tube Training Group (ETG) and Training Group with Conventional Weight Machines (CG). The 3 months follow-up sample was composed of 33 patients, and the study was registered in the Brazilian Clinical Trials Registry (REBEC: RBR-6V9SJJ).
An assessment was individually performed before the beginning of the training, after completing the program training (12 weeks) and after 3 months of follow-up (24 weeks), these evaluations were: spirometry (conducted to confirm the diagnosis of COPD)1, body composition (assessed using bioimpedance analysis - Octopolar InBody 720, Biospace, Seoul, Korea), functional capacity (6MWT)1, QoL (analyzed by COPD Assessment Test- CAT and sleep disorders assessed by the Mini-Sleep Questionnaire - MSQ). To evaluate PA levels the Baecke Questionnaire (BQ) was used.
Training protocolThe training program was performed for 12 weeks, three times per week, 60minutes per session. Materials used included elastic bands (EBG) and elastic tubes (ETG) using chairs specially designed with fixed hooks for these groups, as well as conventional equipment (CG). The exercises used during intervention were: knee extension, knee flexion, shoulder flexion, abduction of shoulder and elbow flexion.
Training protocol consisted of a Maximum Number of Repetitions (MNR) in each set. Therefore, the patient was submitted to a load that had only the MNR imposed by the training dynamics; this consisted of twelve weeks with 2x15 (first week) up to 3x15 (last week) repetitions. The increase in the training load was introduced during the execution of the movement, for EBG and ETG were carried out by adding tubes or bands in the fixed-hooks. The thickness of the elastic tubes indicated different resistances; the greater the thickness the greater the resistance. For CG free weights and pulleys were used.
Statistical analysisOne-way ANOVA was performed to identify the difference between groups at baseline. A 3x3 repeated measures analysis of variance (RMANOVA) with Bonferroni adjustment for multiple comparisons was used to compare group (EBG, ETG and CG) and responses of time (baseline, post training and follow-up). For the comparison between groups (delta values: post training minus baseline and follow-up minus post training) Student T test or Mann Witney was used according to data distribution. Statistical significance was set at p<0.05. The effect size (eta-squared; η2) was calculated across time.
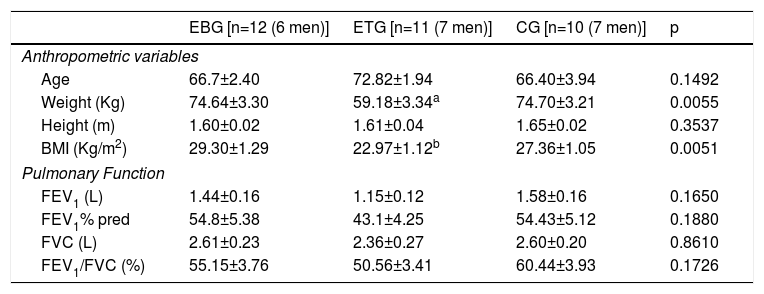
RESULTSAnthropometric and spirometric characteristics of the groups are presented in Table 1.
Anthropometric and spirometric characteristics of the groups. Data expressed as mean and ± standard error.
| EBG [n=12 (6 men)] | ETG [n=11 (7 men)] | CG [n=10 (7 men)] | p | |
|---|---|---|---|---|
| Anthropometric variables | ||||
| Age | 66.7±2.40 | 72.82±1.94 | 66.40±3.94 | 0.1492 |
| Weight (Kg) | 74.64±3.30 | 59.18±3.34a | 74.70±3.21 | 0.0055 |
| Height (m) | 1.60±0.02 | 1.61±0.04 | 1.65±0.02 | 0.3537 |
| BMI (Kg/m2) | 29.30±1.29 | 22.97±1.12b | 27.36±1.05 | 0.0051 |
| Pulmonary Function | ||||
| FEV1 (L) | 1.44±0.16 | 1.15±0.12 | 1.58±0.16 | 0.1650 |
| FEV1% pred | 54.8±5.38 | 43.1±4.25 | 54.43±5.12 | 0.1880 |
| FVC (L) | 2.61±0.23 | 2.36±0.27 | 2.60±0.20 | 0.8610 |
| FEV1/FVC (%) | 55.15±3.76 | 50.56±3.41 | 60.44±3.93 | 0.1726 |
EBG: Elastic band group; ETG: Elastic tube group; CG: Training group with conventional weight machines; Kg: Kilogram; m: meters; Kg/m2: kilogram per square meter; L: Liters; BMI: Body Mass Index; FEV1: Forced expiratory volume in the first second; FEV1% predicted: Forced expiratory volume in the first second percentage predicted; FVC: Forced vital capacity; FEV1/FCV: Ratio between forced expiratory volume in the first second and forced vital capacity; %: percentage.
A total of 33 patients with COPD completed the study, divided into: EBG (degree = GOLD I: 2 patients (17%), GOLD II: 4 (33%), GOLD III: 5 (42%), GOLD IV: 1 (8%); ETG (degree = GOLD I: 0 patients (0%), GOLD II: 3 (27%), GOLD III: 7 (64%), GOLD IV: 1 (9%) and CG (degree = GOLD I: 0 patients (0%), GOLD II: 6 (60%), GOLD III: 3 (30%), GOLD IV: 1 (10%).The results of functional capacity, questionnaires (CAT, MSQ, and PA) and body composition are presented in
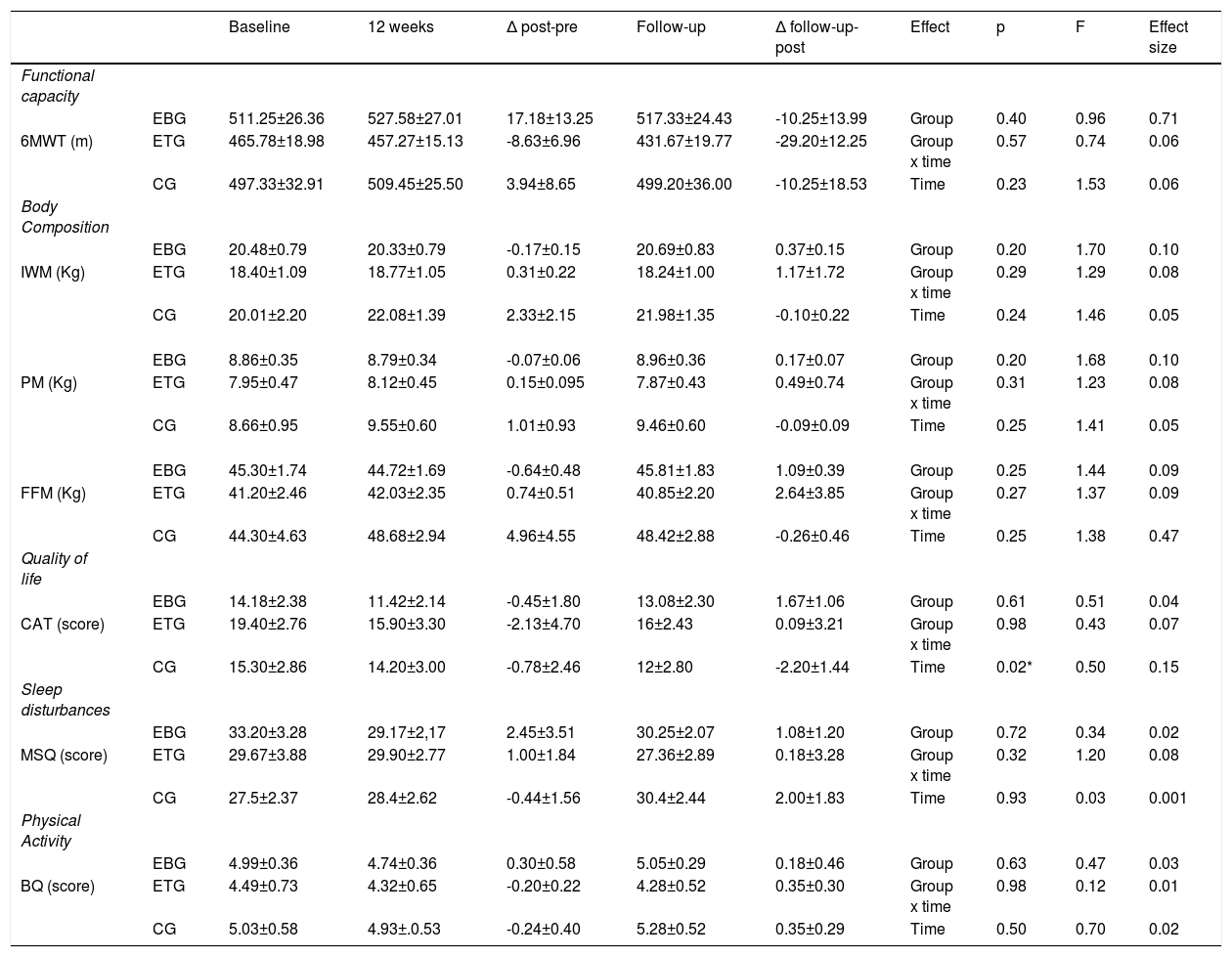
Within the three groups, only CAT questionnaire presented a significant decrease over the three assessments (p<0.05) however, the post- hoc was not significant. Although not a significant one, only among patients from the ETG group was there a decline in their functional capacity after the program. Comparing follow-up with post-program, all three groups reduced their functional capacity but with a similar non-significant amount for EBG and CG, while reaching the Minimum Clinically Important Difference (MCID) on the ETG. The other variables remained stable.
There was a MCID in CAT in EBG and ETG when comparing baseline and after 12 weeks of training (EBG = -2.76 points; ETG= -3.50 points). Table 2
Variables of functional capacity, body composition and questionnaires of quality of life, sleep disturbances and physical activity level expressed as mean ± standard error.
| Baseline | 12 weeks | Δ post-pre | Follow-up | Δ follow-up-post | Effect | p | F | Effect size | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Functional capacity | ||||||||||
| EBG | 511.25±26.36 | 527.58±27.01 | 17.18±13.25 | 517.33±24.43 | -10.25±13.99 | Group | 0.40 | 0.96 | 0.71 | |
| 6MWT (m) | ETG | 465.78±18.98 | 457.27±15.13 | -8.63±6.96 | 431.67±19.77 | -29.20±12.25 | Group x time | 0.57 | 0.74 | 0.06 |
| CG | 497.33±32.91 | 509.45±25.50 | 3.94±8.65 | 499.20±36.00 | -10.25±18.53 | Time | 0.23 | 1.53 | 0.06 | |
| Body Composition | ||||||||||
| EBG | 20.48±0.79 | 20.33±0.79 | -0.17±0.15 | 20.69±0.83 | 0.37±0.15 | Group | 0.20 | 1.70 | 0.10 | |
| IWM (Kg) | ETG | 18.40±1.09 | 18.77±1.05 | 0.31±0.22 | 18.24±1.00 | 1.17±1.72 | Group x time | 0.29 | 1.29 | 0.08 |
| CG | 20.01±2.20 | 22.08±1.39 | 2.33±2.15 | 21.98±1.35 | -0.10±0.22 | Time | 0.24 | 1.46 | 0.05 | |
| EBG | 8.86±0.35 | 8.79±0.34 | -0.07±0.06 | 8.96±0.36 | 0.17±0.07 | Group | 0.20 | 1.68 | 0.10 | |
| PM (Kg) | ETG | 7.95±0.47 | 8.12±0.45 | 0.15±0.095 | 7.87±0.43 | 0.49±0.74 | Group x time | 0.31 | 1.23 | 0.08 |
| CG | 8.66±0.95 | 9.55±0.60 | 1.01±0.93 | 9.46±0.60 | -0.09±0.09 | Time | 0.25 | 1.41 | 0.05 | |
| EBG | 45.30±1.74 | 44.72±1.69 | -0.64±0.48 | 45.81±1.83 | 1.09±0.39 | Group | 0.25 | 1.44 | 0.09 | |
| FFM (Kg) | ETG | 41.20±2.46 | 42.03±2.35 | 0.74±0.51 | 40.85±2.20 | 2.64±3.85 | Group x time | 0.27 | 1.37 | 0.09 |
| CG | 44.30±4.63 | 48.68±2.94 | 4.96±4.55 | 48.42±2.88 | -0.26±0.46 | Time | 0.25 | 1.38 | 0.47 | |
| Quality of life | ||||||||||
| EBG | 14.18±2.38 | 11.42±2.14 | -0.45±1.80 | 13.08±2.30 | 1.67±1.06 | Group | 0.61 | 0.51 | 0.04 | |
| CAT (score) | ETG | 19.40±2.76 | 15.90±3.30 | -2.13±4.70 | 16±2.43 | 0.09±3.21 | Group x time | 0.98 | 0.43 | 0.07 |
| CG | 15.30±2.86 | 14.20±3.00 | -0.78±2.46 | 12±2.80 | -2.20±1.44 | Time | 0.02* | 0.50 | 0.15 | |
| Sleep disturbances | ||||||||||
| EBG | 33.20±3.28 | 29.17±2,17 | 2.45±3.51 | 30.25±2.07 | 1.08±1.20 | Group | 0.72 | 0.34 | 0.02 | |
| MSQ (score) | ETG | 29.67±3.88 | 29.90±2.77 | 1.00±1.84 | 27.36±2.89 | 0.18±3.28 | Group x time | 0.32 | 1.20 | 0.08 |
| CG | 27.5±2.37 | 28.4±2.62 | -0.44±1.56 | 30.4±2.44 | 2.00±1.83 | Time | 0.93 | 0.03 | 0.001 | |
| Physical Activity | ||||||||||
| EBG | 4.99±0.36 | 4.74±0.36 | 0.30±0.58 | 5.05±0.29 | 0.18±0.46 | Group | 0.63 | 0.47 | 0.03 | |
| BQ (score) | ETG | 4.49±0.73 | 4.32±0.65 | -0.20±0.22 | 4.28±0.52 | 0.35±0.30 | Group x time | 0.98 | 0.12 | 0.01 |
| CG | 5.03±0.58 | 4.93±.0.53 | -0.24±0.40 | 5.28±0.52 | 0.35±0.29 | Time | 0.50 | 0.70 | 0.02 |
EBG: Elastic band group; ETG: Elastic tube group; CG: Training group with conventional weight machine; 6MWT: Six-minute walk test; IWM: Intracellular water mass; PM: Protein mass; FFM: Fat free mass; CAT: COPD Assessment Test; MSQ: Mini-Sleep Questionnaire; BQ: Baecke Questionnaire; m: meters; Kg: Kilogram; Δ post-pre: difference between baseline and 12 weeks evaluations of each group expressed as mean and standard error; Δ follow-up-post: difference between 3 months of follow-up and 12 weeks evaluations of each group expressed as mean and standard error; Effect: Comparisons of group (EBG, ETG and CG) and responses of time (Baseline, 12 weeks and 3 months of follow-up);
*: statistical significance p<0.05.
Patients with COPD maintained their body composition and PA levels at 3 months follow-up using elastic components. However, although not significant, there was a decrease in functional capacity. The QoL was also maintained, and MCID was observed in EBG and ETG after 12 weeks of intervention.
It is known that the elderly associated to chronic diseases have a predisposition to functional disability5,6. The results of the present study showed a decrease in functional capacity at 3 months follow-up when using elastic components, suggesting the importance of the continuity of program performed to maintain functional capacity6. This may be explained by age and pulmonary function, that even if these values were not statistically different between groups, the ETG presented higher age and lower pulmonary function values.
Pulmonary Rehabilitation Program (PRP) promotes QoL improvements in patients with COPD7 while sleep disturbances are detrimental to QoL and can lead to mental and physical illness, increasing health expenditure and mortality8. PA is an important protective factor for sleep disorders in the elderly9. Maintenance of body composition in patients with COPD is of extreme importance to reduce mortality10. Ribeiro et al. found that resistance training does not promote increases in fat-free mass when not associated with nutritional support11, which may justify the results found in our study.
In this context, interventions that can promote the maintenance of these variables in patients with COPD are important for functional independence6, QoL7, decrease in hospitalizations and mortality8. In addition, the similar behavior of maintenance of these variables at 3 months follow-up in resistance training using elastic components and conventional training with weight machines is very important, because elastic components have advantages such as low cost, high portability and little demand for space3 compared with the conventional training. Considering this, it is much easier for patients to use such equipment at home if going to rehabilitation center is not possible. In conclusion, in the present study, at 3 months follow-up of resistance training with elastic components, there was maintenance of body composition, health status and PA levels in patients with COPD. However, there was a decrease in functional capacity, but only with minimum clinically important differences, in the ETG group.
The authors would like to thank all the volunteers, the São Paulo State University (UNESP) for allowing the development of this research and for the funders of this research: São Paulo Research Foundation (FAPESP) (#2017/10925-2 #2017/10145-7), National Council for Scientific and Technological Development (CNPq) (#470742/2014-3) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES)001.
Please cite this article as: Silva IG, Silva BSdA, Freire APCF, Santos APSd, Lima FFd, Ramos D, et al. Functionality of patients with Chronic Obstructive Pulmonary Disease at 3 months follow-up after elastic resistance training: a randomized clinical trial . https://doi.org/10.1016/j.pulmoe.2018.09.005