Obstructive sleep apnea syndrome (OSAS) is a systemic inflammatory disease associated with cardiovascular consequences. Red blood cell distribution width (RDW), mean platelet volume (MPV), and platelet distribution width (PDW) are recognized biomarkers of cardiovascular morbidity/mortality. Limited data is available on the association between these parameters and OSAS severity and the relationship with positive airway pressure therapy (PAP). In this prospective study of male OSAS patients we analyzed hematological data in order to evaluate their value in predicting OSAS severity, the relationship with sleep parameters, and their behavior under PAP. Seventy-three patients were included (mean age 46.5 years), of which 36 were mild (49.3%), 10 moderate (13.7%), and 27 severe (37%). The mean RDW increased significantly with OSAS severity and showed a positive correlation with respiratory disturbance index and hypoxemic burdens. Additionally, a group of 48 patients (mean age 47.2 years) were submitted to PAP. After six months, red blood cell count, hemoglobin, hematocrit, and platelet count showed a significant decrease (p<0.0001; p<0.0001; p=0.001; p<0.0001; respectively). Concerning OSAS severity, these parameters also significantly decreased in mild patients (p=0.003; p=0.043; p=0.020; p=0.014; respectively) but only hemoglobin, hematocrit, and platelet count decreased in severe cases (p<0.0001; p=0.008; p=0.018; respectively). This study demonstrated an association between RDW values and OSAS severity. Moreover, red cell and platelet parameters changed significantly after PAP, supporting its cardiovascular protective effect. RDW may become a simple/inexpensive blood biomarker, making it useful in prioritizing OSAS patients waiting for polysomnography, and red cell and platelet parameters could be useful in PAP follow up.
Obstructive sleep apnea syndrome (OSAS) is characterized by recurrent obstructive events and intermittent hypoxia, which in turn contributes to the systemic inflammation that underlies this disease and its consequences.1–3 In concrete terms, the inflammation leads to endothelial dysfunction, which contributes to the pathogenesis of cardiovascular complications in OSAS, in addition to the exposure to risk factors, such as male gender, older age, obesity, and lack of exercise.4
Some red blood cells (RBC) and platelets indices have emerged as inflammatory biomarkers in various diseases, namely chronic obstructive pulmonary disease.5 RBC distribution width (RDW) is a laboratory measure of size variability and respective heterogeneity of circulating erythrocytes. This parameter is calculated by division of standard deviation of RBC volume by mean corpuscular volume (MCV)6 and is widely used to identify potential causes of anemia. In addition, increased RDW contributes to platelet activation. It may affect the outcomes in chronically ill patients as a strong predictor of all-cause mortality in population cohorts.7,8 Hematocrit is expressed as the percent of a blood sample occupied by intact RBC, playing an important role in blood coagulability as it affects blood viscosity and platelet aggregation. Platelet size, as measured by mean platelet volume (MPV), is the best known of the platelet indices and has been a marker of platelet activity and aggregation. Increased MPV may reflect either increased platelet activation or increased numbers of large, hyper-aggregated platelets,9 and may represent a link between hypercoagulability and inflammation.10 Another marker of platelet activation is the platelet distribution width (PDW)11 and is derived from direct flow cytometric measurements of platelet cell volume.
To understand OSAS pathophysiology better, a number of studies have recently appeared evaluating the behavior of hematological parameters, specifically RDW, MPV, and PDW, in this disease. However the information on the association between red cell12–16 and platelets12,15,17–21 indices and OSAS severity is controversial. Therefore, the aim of this study was to investigate the hematological parameters in OSAS, to assess their correlation with the disease severity, and their response to PAP therapy.
Material and methodsThis prospective study consisted of 103 consecutive male subjects with suspected OSAS, who were evaluated through interviews at a Sleep Clinic.
Exclusion criteria were female gender (to avoid hormonal influence), other sleep disorders, chronic disorders such as anemia, polycythemia, other hematological diseases, hepatic, kidney, and neuromuscular disease. Also excluded were patients with heart failure, neoplasia, acute disease, hypoxemia, and previous PAP treatment.
Demographic and clinical data were collected in all selected patients. Additionally, these patients underwent an overnight polysomnography (PSG) study using Embla S7000 System (Embla; USA) with continuous sleep-technician monitoring. Sleep recordings and events were analyzed manually according to standard criteria.22 The respiratory disturbance index (RDI), oxygen desaturation index (ODI), percentage of time with saturation under 90% (T90) and lowest oxygen saturation (SpO2) were calculated.
Based on the RDI≥5events/hour, patients were diagnosed as OSAS (n=73) and grouped into mild (RDI 5–14.9), moderate (RDI 15–29.9), and severe (RDI≥30). Further, in pretreatment analysis of 73 patients, moderate and severe groups were combined (RDI≥15).
After diagnosis, PAP therapy with automatic devices (S9, Resmed, Australia) was prescribed for 48 patients according to clinical and polysomnographic criteria,23 in severe disease or in disease of any severity when associated with excessive diurnal sleepiness and/or cardio/cerebrovascular complications. Further, in pre/post treatment analysis of 48 patients, moderate and severe groups were combined (RDI≥15).
Venous blood samples were collected during the morning after PSG (between 7:30am and 09:00am) and a 12h fasting, into EDTA-coated polypropylene tubes. From patients who had undergone PAP treatment, and were free of any acute disease, a second morning blood sample was collected after six months under the same conditions as above described. In all samples, the collected blood was processed between one and two hours in the same equipment (ADVIA 2120i – Siemens). From routine complete hemogram, RBC count, hemoglobin, hematrocrit, MCV, RDW, platelets count, MPV, and PDW were determined.
At six months, patients under PAP were evaluated for compliance based on PAP software data. More than 4h use/night for at least five days/week was accepted as compliance, as described previously.24
The study protocol was approved by the local ethics committees and all patients gave written informed consent.
Statistical analyses were performed using SPSS for windows software (SPSS Inc., Chicago, IL, USA). All variables were tested for normality of the distribution using Kolmogorov–Smirnov test. Continuous variables with normal distributions were expressed as mean±standard deviation (SD). Continuous variables with non-normal distributions were summarized as medians (interquartile rang, IQR). Categorical variables were expressed as numbers (percentages). Spearman analysis was performed for correlations between nonparametric variables. Pearson's analysis was performed for correlations between parametric variables. Student t-test was used for comparisons between independent groups for the values that were normally distributed and Mann–Whitney U-test for comparisons between values not normally distributed. Paired t-test was used when comparing mean values before and after PAP treatment. Categorical variables were compared using ¿2 test. To compare variables not normally distributed before and after PAP treatment, such as MPV and PDW, the Wilcoxon test was used. Results were considered statistically significant when p value was <0.05.
ResultsHematological evaluation in OSAS before treatmentClinical and hematological parameters of OSAS patients are shown in Table 1. A total of 73 male patients with OSAS were included, where 36 were mild (49.3%), 10 were moderate (13.7%), and 27 were severe (37%). There were not statistically significant differences between mild and moderate–severe groups regarding demographic parameters, medical history and Epworth sleepiness scale score.
Clinical and hematological data of OSAS patients before treatment.
| Total (N=73) | Mild OSAS (N=36) | Moderate OSAS (N=10) | Severe OSAS (N=27) | Mild vs. moderate-severe (p) | |
|---|---|---|---|---|---|
| Age (years) [mean (SD)] | 46.5 (7.7) | 47.3 (8.2) | 42.5 (7.7) | 47 (7) | 0.289 |
| Active smoking habits [n (%)] | 16 (22.2) | 6 (16.7) | 3 (33.3) | 7 (25.9) | 0.398 |
| Pack years [mean (SD)] | 21.5 (31.8) | 30 (22.3) | 20 (–)a | 20 (35) | 0.177 |
| Cardiac disease [n (%)] | 39 (53.4) | 18 (50) | 2 (20) | 19 (70.4) | 0.563 |
| Respiratory disease [n (%)] | 17 (23.3) | 8 (22.2) | 3 (30) | 6 (22.2) | 0.832 |
| Diabetes [n (%)] | 11 (15.1) | 4 (11.1) | 1 (10) | 6 (22.2) | 0.351 |
| Dyslipidemia [n (%)] | 54 (74) | 25 (69.4) | 6 (60) | 23 (85.2) | 0.384 |
| BMI (kg/m2) [median (IQR)] | 30.3 (4.8) | 28.0 (3.2) | 28 (4.4) | 31.6 (4.4) | 0.005 |
| EPW scale [mean (SD)] | 9.5 (4.7) | 9.2 (4.6) | 11.6 (4.6) | 9 (5) | 0.748 |
| RDI (events/hour) [median (IQR)] | 17 (29.3) | 8.9 (4) | 21.6 (6) | 47.3 (34) | <0.0001 |
| T90 (%) [median (IQR)] | 0.7 (8) | 0.2 (0.7) | 0.5 (3.0) | 10.8 (28.9) | <0.0001 |
| Sleep efficiency (%) [median (IQR)] | 84.5 (17.0) | 84 (15) | 87 (13) | 83 (24) | 0.886 |
| ODI (desaturation/h) [median IQR)] | 10.8 (26.3) | 6.9 (5.8) | 15.3 (10.7) | 46.6 (38.7) | <0.0001 |
| Lowest SpO2 (%) [median (IQR)] | 85 (9) | 86 (7) | 86 (12.5) | 79 (12) | <0.0001 |
| Diurnal SpO2 (%) [median (IQR)] | 97 (1) | 97 (1) | 97 (2) | 97 (1) | 0.403 |
| RBC count (×1012/L) [mean (SD)] | 5.0 (0.4) | 5.0 (0.3) | 5.0 (0.5) | 5.1 (0.4) | 0.517 |
| Hemoglobin (g/dL) [mean (SD)] | 15.3 (1.1) | 15.2 (1.0) | 14.7 (1.3) | 15.7 (1.1) | 0.486 |
| Hematocrit (%) [mean (SD)] | 45.0 (3.2) | 45.0 (2.9) | 43.2 (3.7) | 45.8 (3.3) | 0.895 |
| MCV (fL) [mean (SD)] | 89.4 (4.1) | 89.8 (3.9) | 87 (3.3) | 89.7 (4.5) | 0.414 |
| RDW (%) mean (SD)] | 13.4 (0.7) | 13.2 (0.6) | 13.5 (0.7) | 13.5 (0.8) | 0.029 |
| Platelet count (×109/L) [mean (SD)] | 231.6 (57.4) | 229.2 (51.7) | 226.2 (37.4) | 236.8 (70.7) | 0.726 |
| MPV (fL) [median (IQR)] | 8.8 (1.3) | 8.6 (1.2) | 8.7 (1.1) | 9.2 (1.6) | 0.302 |
| PDW (%) [mean (SD)] | 49.0 (7.5) | 48.4 (9.0) | 48.7 (3.8) | 51.2 (9.7) | 0.074 |
BMI: body mass index; RDI: respiratory disturbance index; T90: % of time with saturation under 90%; SpO2: oxygen saturation; ODI: oxygen desaturation index; RBC: red blood cell count; MCV: mean corpuscular volume; RDW: red blood cell distribution width (RDW). MPV: mean platelet volume; PDW: platelet distribution width.
Considering hematological parameters, only RDW was statistically higher in moderate–severe OSAS patients compared to mild (p=0.029). The mean RDW increased significantly with OSAS severity, the difference between mild and moderate–severe groups being statistically significant (p=0.029). In addition, RDW showed a positive mild correlation with RDI, ODI, and T90 and a negative mild correlation with lowest SpO2 (Table 2), and was more affected by ODI.
Correlation analysis between RDW and sleep parameters.
| Spearman correlation coefficient (rs) | p | |
|---|---|---|
| RDI (events/h) | 0.248 | 0.034 |
| Lowest SpO2 (%) | −0.261 | 0.025 |
| T90 (%) | 0.292 | 0.012 |
| ODI (desaturation/h) | 0.338 | 0.003 |
RDI: respiratory disturbance index; SpO2: oxygen saturation; T90: desaturation time under 90%; ODI: oxygen desaturation index.
Clinical and hematological parameters of OSAS patients under treatment are shown in Table 3. A total of 48 OSAS patients underwent PAP therapy, where 18 were mild (37.5%), 5 were moderate (10.4%), and 25 were severe (52.1%). There were not statistically significant differences between mild and moderate–severe groups regarding demographic parameters, medical history, Epworth sleepiness scale score, and PAP compliance. However, BMI was higher in moderate–severe group compared with mild group (p=0.023).
Clinical and hematological data of OSAS patients with criteria for PAP therapy (before treatment).
| Total (N=48) | Mild OSAS (N=18) | Moderate OSAS (N=5) | Severe OSAS (N=25) | Mild vs. moderate-severe OSAS (p) | |
|---|---|---|---|---|---|
| Age (years) [mean (SD)] | 47.2 (7.6) | 48 (9) | 47 (7) | 47 (7) | 0.638 |
| Active smoking habits [n (%)] | 9 (19.9) | 1 (5.6) | 2 (50) | 6 (24) | 0.071 |
| Pack years [mean (SD)] | 5 (20) | –a | 15 (–) | 35 (41) | 0.065 |
| Cardiac disease [n (%)] | 30 (62.5) | 11 (61.1) | 2 (40) | 17 (68) | 0.492 |
| Respiratory disease [n (%)] | 10 (20.8) | 2 (11.1) | 2 (40) | 6 (24) | 0.317 |
| Diabetes [n (%)] | 9 (18.8) | 3 (16.7) | 1 (20) | 5 (20) | 0.960 |
| Dyslipidemia [n (%)] | 34 (70.8) | 12 (66.7) | 2 (40) | 20 (80) | 0.176 |
| BMI (kg/m2) [median (IQR)] | 31.1 (4.3) | 29.5 (4.7) | 29 (4.2) | 31.6 (4.1) | 0.023 |
| EPW scale [mean (SD)] | 10.4 (4.7) | 12 (4) | 11 (7) | 9 (5) | 0.078 |
| RDI (events/h) [median (IQR)] | 32.9 (42) | 9.0 (3) | 21.4 (7) | 48.7 (35) | <0.0001 |
| T90 (%) [median (IQR)] | 1.7 (11.1) | 0.3 (0.6) | 2.7 (5.5) | 10.8 (30.1) | <0.0001 |
| Sleep efficiency (%) [median (IQR)] | 80.5 (23.3) | 78.2 (23.7) | 83.5 (28) | 79.7 (23.4) | 0.670 |
| ODI (desaturation/h) [median (IQR)] | 19.3 (41.5) | 7.2 (4) | 18.6 (16.8) | 49.7 (41.5) | <0.0001 |
| Lowest SpO2 (%) [median (IQR)] | 80.0 (8.2) | 86 (6.3) | 76 (19) | 79 (14.5) | 0.001 |
| Diurnal SpO2 (%) [median (IQR)] | 96 (1) | 97 (1.1) | 98 (3) | 97 (2) | 0.689 |
| RBC count (×1012/L) [mean (SD)] | 5.1 (0.4) | 5.0 (0.3) | 5.0 (0.6) | 5.1 (0.4) | 0.400 |
| Hemoglobin (g/dL) [mean (SD)] | 15.4 (1.2) | 15.2 (1.0) | 14.6 (1.9) | 15.7 (1.1) | 0.263 |
| Hematocrit (%) [mean (SD)] | 45.0 (3.3) | 44.5 (2.6) | 43.4 (2.1) | 45.7 (3.3) | 0.233 |
| MCV (fL) [mean (SD)] | 88.9 (4.4) | 88.6 (4.3) | 86.4 (2.1) | 89.7 (4.6) | 0.749 |
| RDW (%) [mean (SD)] | 13.4 (0.7) | 13.0 (0.5) | 13.6 (0.9) | 13.6 (0.7) | 0.005 |
| Platelet count (×109/L) [mean (SD)] | 232.4 (59.7) | 235.6 (75.3) | 234.2 (31.3) | 229.6 (68.4) | 0.537 |
| MPV (fL) [median (IQR)] | 9.0 (1.3) | 8.6 (1.3) | 8.5 (2.6) | 9.2 (1.8) | 0.594 |
| PDW (%) [mean (SD)] | 50.2 (8.2) | 49.3 (6.3) | 49.8 (5.8) | 51.0 (1.0) | 0.975 |
BMI: body mass index; RDI: respiratory disturbance index; T90: desaturation time under 90%; SpO2: oxygen saturation; ODI: oxygen desaturation index; RBC: red blood cell count; MCV: mean corpuscular volume; RDW: red blood cell distribution width (RDW). MPV: mean platelet volume; PDW: platelet distribution width.
Considering hematological parameters, there were not statistically significant differences between mild and moderate–severe groups
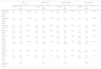
After six months of compliant PAP treatment (Table 4) the hemogram data, although showing normal reference values, revealed a significant decrease in the RBC count, hemoglobin, hematocrit, and platelet count in all patients (p<0.0001; p<0.0001; p=0.001; p<0.0001; respectively). Considering each severity group, these same parameters significantly decreased after PAP treatment in mild patients (p=0.003; p=0.043; p=0.020; p=0.014; respectively) and in severe patients only hemoglobin, hematocrit, and platelet count decrease significantly (p<0.0001; p=0.008; p=0.018; respectively).
Hematological data of OSAS patients before and after treatment.
| Total (N=48) | Mild OSAS (N=18) | Moderate OSAS (N=5) | Severe OSAS (N=25) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-PAP | Post-PAP | p | Pre-PAP | Post-PAP | p | Pre-PAP | Post-PAP | p | Pre-PAP | Post-PAP | p | |
| RBC Count (×1012/L) [mean (SD)] | 5.1 (0.4) | 4.9 (0.3) | <0.0001 | 5.0 (0.3) | 4.9 (0.3) | 0.003 | 5.0 (0.6) | 5.0 (0.42) | 0.684 | 5.1 (0.4) | 5.0 (0.3) | 0.005 |
| Hemoglobin (g/dL) [mean (SD)] | 15.4 (1.2) | 14.9 (1.0) | <0.0001 | 15.2 (1.0) | 14.9 (0.9) | 0.043 | 14.6 (1.9) | 14.6 (1.5) | 0.908 | 15.7 (1.1) | 15.0 (1.0) | <0.0001 |
| Hematocrit (%) [mean (SD)] | 45.0 (0.3) | 43.9 (3.0) | 0.001 | 44.5 (2.6) | 43.2 (3.0) | 0.020 | 43.4 (5.2) | 43.5 (4.1) | 0.981 | 45.7 (3.3) | 44.5 (2.9) | 0.008 |
| MCV (fL) [mean (SD)] | 88.9 (4.4) | 88.9 (3.8) | 0.908 | 88.6 (4.3) | 88.8 (3.7) | 0.780 | 86.4 (2.1) | 86.8 (1.2) | 0.339 | 89.7 (4.6) | 89.5 (4.2) | 0.674 |
| RDW (%) [mean (SD)] | 13.4 (0.7) | 13.6 (0.8) | 0.070 | 13.1 (0.5) | 13.6 (0.9) | 0.059 | 13.6 (0.9) | 13.9 (1.2) | 0.621 | 13.6 (0.7) | 13.7 (0.7) | 0.711 |
| Platelet Count (×109/L) [mean (SD)] | 232.4 (59.7) | 212.0 (51.6) | <0.0001 | 235.6 (75.3) | 217.6 (52.9) | 0.014 | 234.2 (31.3) | 201.6 (28.0) | 0.097 | 229.6 (68.4) | 210.0 (55.2) | 0.018 |
| MPV (fL) [median (IQR)] | 9.0 (1.2) | 9.0 (1.7) | 0.900 | 8.6 (1.3) | 8.7 (1.2) | 0.736 | 8.7 (1.1) | 9.2 (1.2) | 0.242 | 9.2 (1.2) | 9.0 (2.3) | 0.737 |
| PDW (%) [mean (SD)] | 50.2 (8.5) | 49.5 (15.3) | 0.781 | 49.3 (62.5) | 51.4 (9.4) | 0.287 | 49.6 (2.9) | 51.4 (10.1) | 0.631 | 51.0 (10.0) | 49.5 (17.1) | 0.727 |
| PAP compliance (h) [mean (SD)] | – | 4.7 (1.9) | – | – | 4.3 (1.4) | – | – | 6.1 (1.8) | – | – | 4.9 (2.3) | – |
RBC: red blood cell count; MCV: mean corpuscular volume; RDW: red blood cell distribution width (RDW). MPV: mean platelet volume; PDW: platelet distribution width.
In conclusion, concerning hematological evaluation in OSAS patients before PAP therapy, only RDW showed statistical increase according to OSAS severity. However, after six months of PAP therapy RDW values had not changed, which may be due to a small sample size.
DiscussionThis study reinforces the importance of hematological evaluation as an easy complementary tool to the global approach to OSAS patients by showing that RDW increased significantly with OSAS severity and that red cell count, hemoglobin, hematocrit, and platelet count mean values significantly decreased after PAP treatment. These findings suggest that RDW might be used as marker of OSAS severity and RBC and platelets count, hemoglobin, and hematocrit used as markers of response to treatment. In this study, the possible confounding effects of several factors/diseases on the studied parameters were excluded, such as age, smoking habits, and co-morbidities since there were no statistical differences regarding these factors between different OSAS severity levels, and neither group showed the presence of anemia.
Hematological evaluation in OSAS before treatmentThere has not been consensus in previous studies in literature about RDW expression in OSAS. Some authors showed that RDW values were higher in OSAS patients than in controls13,14 and also higher in those with cardiovascular diseases.13 While others reported that RDW mean values were similar in OSAS patients compared to snorers.16
Considering these facts, we intended to evaluate the expression of RDW according to OSAS severity and in our study RDW increased significantly with severity of OSAS. Additionally, RDW showed a positive correlation with RDI and hypoxemic burdens (ODI, T90 and lowest SpO2). The exact mechanism of these results is not clear; however, this may be related to the existence of chronic inflammation. In fact, chronic inflammation promotes red blood cell membrane deformability and changes in erythropoiesis, thus increasing RDW.25
Moreover, the fact that RDW was also associated with hypoxemic burdens could be explained by the effect of hypoxia. In OSAS, sustained hypoxia, leads to activation of hypoxia inducible factor 1 resulting in increased erythropoietin expression26 and consequently higher RDW. These results, taken altogether, support our proposed role of RDW as a simple surrogate marker for OSAS severity.
A previous study, which compared controls with OSAS patients, reported a significant correlation between RDW and the apnea-hypopnea index (AHI), age, and mean SpO2.13 Also, the study of Sökücü and co-workers found that RDW was higher in patients with OSAS and increased significantly with severity, even after correction for anemia.14 Recently, Gunbatar and coworkers showed that RDW in OSAS patients was similar compared to snorers. They, also, reported that BMI, AHI, pulmonary artery pressure, and T90 were positively correlated with RDW in patients with OSAS.16 However, age and BMI were different between patients and controls, which could be confounding factors. Another recent study reinforced the idea that RDW could be a marker for OSAS severity27 because it was positively correlated with AHI, ODI, Epworth sleepiness scale, hematocrit and negatively correlated with minimum SpO2 and rapid eye movement sleep. However, in this multivariable analysis, only ODI was an independent predictor of RDW, which means a higher ODI will predict a higher RDW.
Additionally, in our study other hematological parameters did not significantly change with OSAS severity. In literature there are controversial results about the expression of these parameters in OSAS.16–19 Some authors have reported that the hematocrit, platelet count, MPV, and PDW increased in OSAS and correlated positively with severity,27 even after controlling for possible confounding factors. However, OSAS patients usually do not show clinical polycythemia.28 Our results, concerning the PDW and MPV tendency to increase with OSAS severity, could be explained by increased platelet activation and aggregation.29,30 In fact, MPV is an indicator of platelet activation which could result from sympathetic overactivity,31 hypoxia,32 and inflammation,33,34 all being well-known features of OSAS.2,3,35 Additionally, platelet activation may contribute to the increased incidence of cardiovascular events in patients with OSAS.36,19
Hematological evaluation in OSAS under treatmentAfter six month of PAP treatment, patients showed a significant decrease in RBC count, hemoglobin, hematocrit, and platelet count. Sustained hypoxia results in increased expression of erythropoietin26 inducing erythropoiesis with consequent increase in hematological parameters. PAP correction of respiratory events and consequent hypoxia and inflammation can translate in a decrease in RBC and platelets counts, hemoglobin, and hematocrit as obtained in our study. On the other hand, the tendency to decrease MPV and PDW could be also explained by the fact that besides PAP decreasing hypoxia and inflammation, it also improves platelet aggregability.37
Our results agree with previous studies that showed decreases in hematocrit after PAP treatment.38,39 A recent study20 reported a significant reduction of hematocrit and MPV, while RDW and PDW increased after six months of PAP treatment in patients with severe OSAS.
There are potential limitations of this study, such as the small sample size, exclusion of women, and lack of comparison with a group of OSAS patients under sham PAP. Also, in this study we did not evaluate the correlation of some markers of inflammation, neurohormonal activation, or oxidative stress with these hematological parameters. The lack of exclusion of OSAS patients with hypertension, diabetes or chronic medication such as anti-coagulation, anti-aggregation, anti-inflammation or immunosuppression agents is also an additional limitation. Finally, although our study population was not anemic, we did not measure nutritional status, which could be a potential cause of increased RDW.
ConclusionsOur study has established the importance of hematological evaluation as complementary tool for diagnosis and treatment response in OSAS patients.
RDW, as a marker of OSAS severity, can be used as an easy/inexpensive tool for triaging OSAS patients in laboratories with long waiting lists. While RBC and platelets count, hemoglobin, and hematocrit could be used as markers of response to treatment, both in primary and secondary care settings.
Further studies, with a bigger sample, inclusion of women (before and after menopause), hematological cut-off points for diagnosis and treatment, are needed.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflict of interest to declare.
To patients that voluntarily collaborated in this study. Project partially supported by Harvard Medical School-Portugal Program (HMSP-ICJ/0022/2011).