Cystic lung disease (CLD) encompasses a broad set of uncommon disorders that can represent a diagnostic challenge, in part due to an increasing number of diseases with similar presentation.1 Hypersensitivity pneumonitis (HP) is a complex and heterogeneous interstitial lung disease (ILD) caused by an exaggerated immune response to an inhaled antigen in predisposed individuals.2
Cysts have been reported in a small percentage of patients with non-fibrotic HP3; they are typically few (less than 5% of lung parenchyma), range from 3 to 25 mm in diameter and are associated with ground-glass opacities. The cysts resemble those of lymphoid interstitial pneumonia and are presumably caused by partial bronchial obstruction due to peribronchiolar lymphocytic infiltrate present in patients with HP.4,5
HP diagnosis is often difficult to achieve in part due to nonspecific clinical manifestations but also because radiological and histological patterns can mimic other interstitial and small airway disease. Taking this into account, a minority of patients may present thin-walled lung cysts as the main chest high-resolution computed tomography (HRCT) characteristic, which requires a differential diagnosis with others CLDs.
We present a case of a 54-year-old women, non-smoker, who owned parakeets and goldfinches and lived near a square frequently occupied by pigeons; her personal medical history included chronic kidney disease and dyslipidemia.
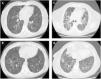
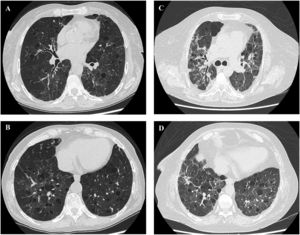
She was referred to our outpatient clinic complaining of fatigue and progressive dyspnea with moderate exertion in the previous year. Chest HRCT showed bilateral multiple cysts predominantly in the pulmonary inferior lobes (Fig. 1A,B), some traction bronchiectasis and limited areas of emphysema and mosaic attenuation. Serum specific IgGs were positive for parakeets and pigeons. Complete autoimmune study and VEGF-D were normal. Pulmonary function tests revealed FVC 89,9% and a severe-moderate decrease in DLCO (DLCO 49,4%, KCO of 57,3%). Bronchoalveolar lavage with differential cell count showed 15% of lymphocytes. The nonspecific nature of these results combined with the possibility of other CLD, like lymphocytic interstitial pneumonia, prompted a request for a lung biopsy; the histological examination revealed a cellular interstitial pneumonitis with peribronchiolar pattern and microgranulomas compatible with HP.
Once the diagnosis of HP was established, the patient was advised to avoid any contact with possible allergens and inhaled corticosteroid and bronchodilators were prescribed. Initially, the patient improved and remained stable, reporting only mild dyspnea (mMRC 0-1) during moderate/ hard exercises, especially after being in the square and exposed to pigeons and other birds; over time there was a substantial improvement in the respiratory functions tests, with a FVC of 93%, a DLCO of 66% and a KCO of 80%.
After ten years the patient experienced clinical and functional worsening (FVC 74%, DLCO 48% and KCO 66%) and was put on oral corticosteroids (prednisolone 5mg/day), with favorable response.
Currently, the patient is clinically and functionally stable (FVC 84%, DLCO 55% and KCO 72%); although HRCT shows no changes regarding multiple cysts, there are extensive areas with mosaic attenuation associated with ground glass opacities, traction bronchiectasis and loss of lobar volume (Fig. 1C,D).
Cystic lung diseases are increasingly recognized as a heterogeneous group of ILD with a broad spectrum of outcomes and consequences; the widespread use of HRCT has had an important role in this increased knowledge and understanding.1 HP is a good prognosis disease often diagnosed by a combination of typical clinical history, positive serum precipitins and a characteristic bronchoalveolar lavage.3 Cystic HP is a rare form of HP frequently associated with a challenging diagnosis4; in these cases, where there is an extensive overlap between clinical and radiographic features, lung biopsy and histopathologic evaluation may be crucial to establishing a confident diagnosis. Faced with this scenario it is important to weigh the need for a secure histopathological diagnosis against the risks of the medical procedure. In recent years and in part due to an increasing demand for histological evaluations in patients with comorbid conditions, poor overall health status, physical frailty and a more severe degree of lung function impairment the role of transbronchial cryobiopsy (TBLC) in ILD patients has grown. Nowadays, compared to surgical lung biopsy, TBLC offers a less invasive diagnostic method that is almost as accurate as surgical lung biopsy but has a better safety profile.6
Furthermore, and similar to other non-cystic forms of HP, cystic HP can slowly progress over time, especially the inflammatory-fibrotic component, even after removing exposures and treating acute exacerbations; interestingly, the cystic component of the disease seems to remain stable.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical considerationsWritten informed consent was obtained from the patient for publication of the article.
CRediT authorship contribution statementE.M. Tinoco: Writing – original draft, Writing – review & editing. G. Bermudo: Methodology, Writing – review & editing. V. Vicens-Zygmunt: Methodology, Writing – review & editing. P. Luburich: Writing – review & editing. R. Llatjós: Writing – review & editing. M. Molina-Molina: Writing – original draft, Methodology, Writing – review & editing.