Idiopathic pulmonary fibrosis (IPF) is a progressive, life-threatening interstitial pneumonia of unknown cause1, affecting elderly, frail individuals with a median age at diagnosis of 661 and a median estimated survival of 2.5–3.5 years after diagnosis.2-3
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) rapidly spread worldwide and the absence of effective therapies or vaccines at the beginning of the pandemic led Governments to enforce strict measures in their efforts to limit the virus transmission.4 On March, 9th 2020 Italy went into a full lockdown. In parallel, hospital infrastructures were redirected towards maximizing intensive care resources which resulted in routine clinical practice, including IPF outpatient clinics, being considerably reduced.5
The aim of our study was to assess the mortality of IPF patients included in the cohort of the tertiary outpatient IPF clinic at the “San Gerardo” Hospital, located in Monza (Lombardy, the most populated Italian region) in relation to the social and healthcare changes due to COVID-19 pandemic.
We analyzed a cohort of 212 patients recruited between May 2008 and April 2021 and alive on January 1st 2018. We recorded mortality data comparing the characteristics between patients who died in January 1st, 2018 and February 28th, 2020 (pre-pandemic and pre-lockdown period) to those who died between March 1st, 2020 and April 30th, 2021 (pandemic and post-lockdown period) using Chi-square or Fisher's exact tests for categorical variables and Mann–Whitney U test for continuous ones. Thereafter, we computed monthly average crude mortality rates for each of the two periods, with related exact 95% confidence intervals (95%CIs) based on a Poisson distribution, and we compared them through incidence rate ratios (IRR). Similarly, we computed trimestral-specific monthly average mortality rates for the biennium 2018-2019, and we compared them with those of 2020. Person-time at risk (in months) was computed for each subject from January, 1st 2018 or the day of IPF diagnosis, until death or the end of the period of interest. 95%CIs for IRR were based on the exact distribution of the rate of two Poisson counts, as well as 2-sided p-values. All analyses were performed using SAS version 9.4 (The SAS institute, Cary, NC) and R version 4.0.3 (R Core Team, Vienna, Austria) with the packages epitools and rateratio.test. The study received Ethics Committee approval (ASST Monza, 1538, November 14th 2019).
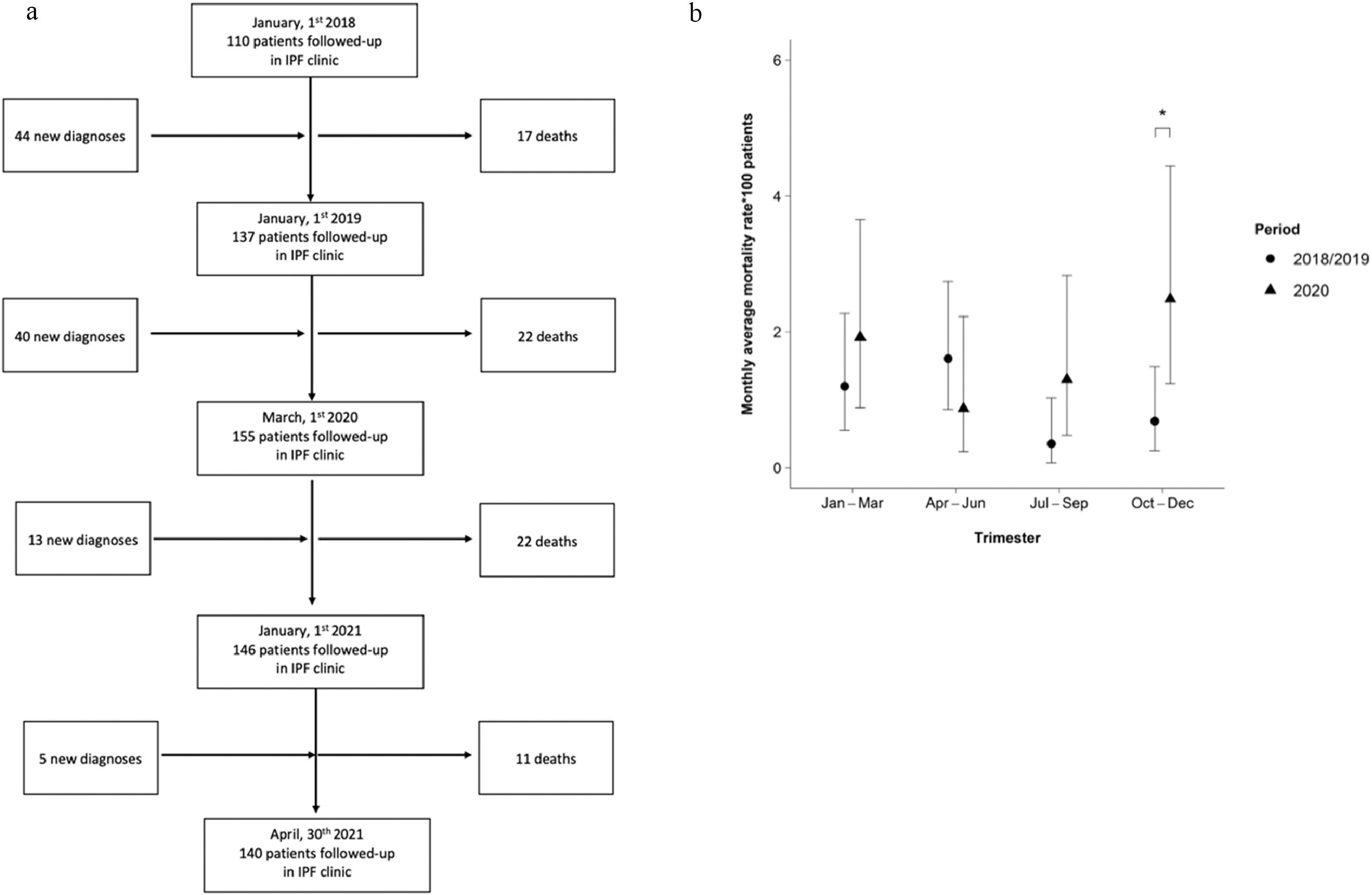
In the pre-lockdown period, we documented 39 deaths in our IPF cohort; in contrast, in the post-lockdown period, 33 IPF patients died (Fig. 1a). We observed a significantly younger median age at death and a trend toward younger median age at diagnosis in the pre-lockdown compared to the post-lockdown period with similar median disease duration, pulmonary function tests and severity of the disease evaluated through Gender-Age-Physiology (GAP) index (Table 1). We did not detect statistically significant differences regarding gender or antifibrotic treatment. The burden of comorbidities was similar between the two groups with the exception of pulmonary hypertension that was more common in the post-lockdown period.
Demographics and clinical characteristics of study population.
DLCO= diffusing capacity for carbon monoxide; FVC= Forced Vital Capacity; GAP= Gender-Age-Physiology
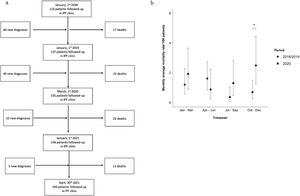
We estimated that monthly average mortality rates rose from 1.03 per 100 person-months (95%CI: 0.72-1.42) during the pre-lockdown period to 1.67 (95%CI: 1.17-2.33) post-lockdown: such increase was borderline significant, corresponding to an IRR of 1.63 (95%CI: 1.00-2.66, p=0.05). In detail, comparing the various trimestral periods, we observed a statistically significant increase in mortality in the last trimester (October/December) of 2020, as compared to the last trimester 2018: monthly average mortality rates increased from 0.68 (95%CI: 0.25-1.48) to 2.48 (1.24-4.44) per 100 person-months (IRR: 3.64, 95%CI: 1.24-12.00, p=0.008, Fig. 1b).
In the lockdown periods, patients included in our IPF cohort were regularly followed-up with telephone calls and continuously received antifibrotic treatment. Asking family members, we were able to determine that 3 out of 33 patients (9.1%) were hospitalized and died because of a confirmed diagnosis of Coronavirus disease (COVID-19) and that the great majority, 30/33 (90.9%), died at home or in long-term facilities without signs or symptoms suggestive of COVID-19.
This study showed a significant increase in mortality in our IPF cohort during the post-lockdown period that, in most of the cases, did not appear directly related to COVID-19.
In line with our results, Marcon and colleagues showed an excess of IPF-related deaths during the first wave of the COVID-19 pandemic.6 However, the authors did not differentiate between deaths directly related to COVID-19 and other etiologies.
In our study, we observed a marginally significant increase in mortality during post-lockdown period compared to pre-lockdown. We believe that the increase in mortality is mainly related to the increased frailty and to limitation of access to the IPF Referral Center for a worsening of the disease during the peak of the pandemic. This is corroborated by the results of the trimestral analysis which shows an increase in the period of the COVID-19 second wave (October/December 2020), when our province (Monza-Brianza) reached the highest level of incidence of SARS-CoV-2 infection.
In our study, a number of limitations should be acknowledged. The cause of death was not confirmed for the majority of the patients. Moreover, this study was performed in a single center, limiting the generalizability of the results. Finally, given the small sample size, we were not able to run a Cox-analysis that would have been the best way to address the risk factors for mortality adjusting for possible confounders.
In conclusion, we report a statistically significant increase in mortality within our IPF cohort during the COVID-19 second wave. To the best of our knowledge, only in a minority of patients was the cause of death directly related to SARS-CoV-2 infection. In most patients, the cause of death was possibly related to the limitations to reaching the hospital and ILD-physicians of the IPF referral Center in relation to the COVID-19 pandemic in case of worsening of the disease.
Authors’ contributionsFL is the guarantor of this research. PF, SC, GF, FM, LGM and FL were responsible for study concept and design. PF, SC, GF, FM and FL contributed to data acquisition. PF, SC, GF, FM, LGM and FL performed data analysis. PF, SC, GF, FM, ER, LGM and FL contributed to the drafting of this manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participateThe study received Ethics Committee approval (ASST Monza, 1538, November 14th 2019).
Consent for publicationWritten informed consent was waived given the retrospective design of the study.