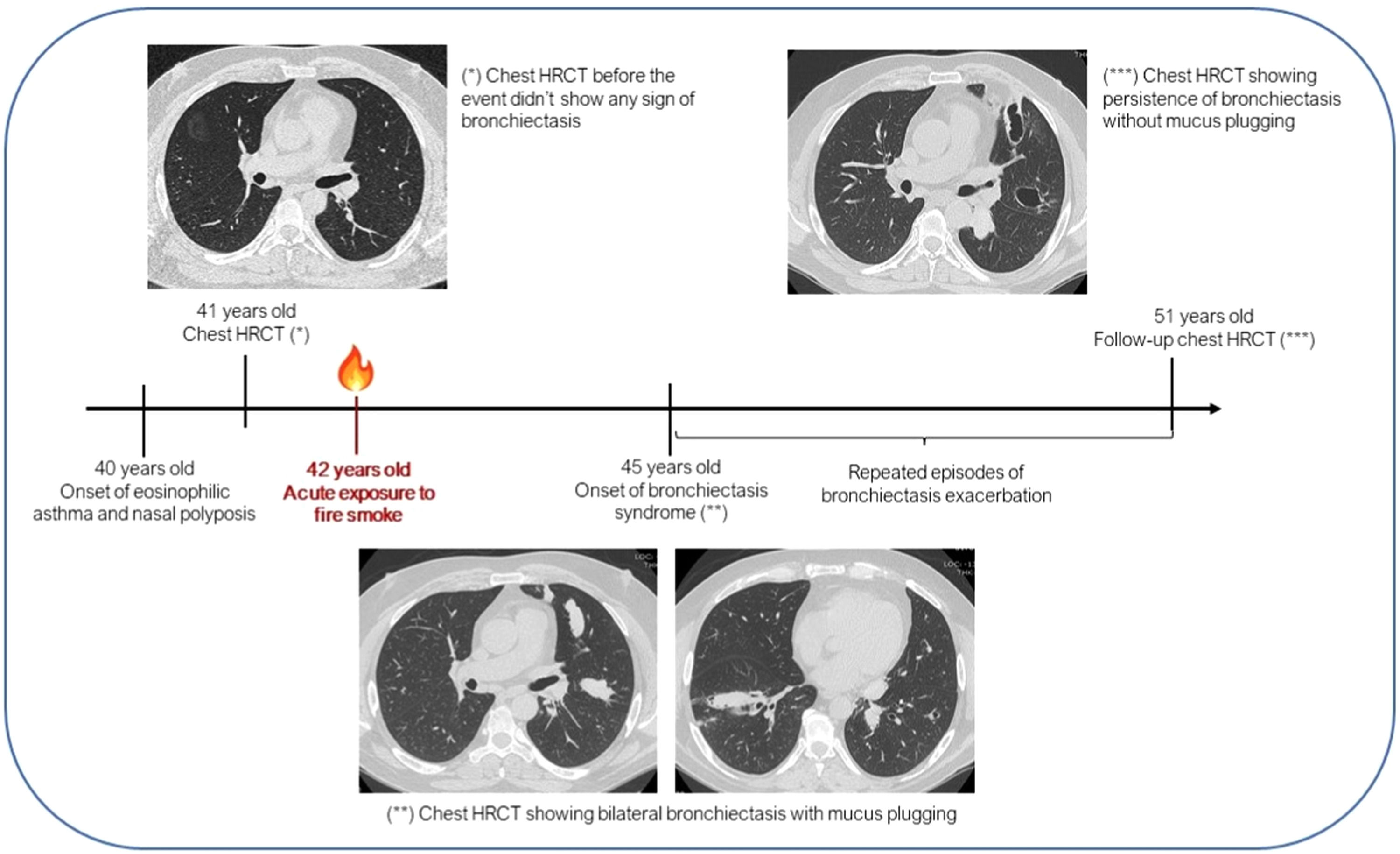
Inhalation injury remains one of the most challenging injuries for burn care providers. Long-term complications of smoke inhalation have rarely been reported in literature and these may be an unusual cause of bronchiectasis.1 In this letter to editor, we discuss the occurrence of radiological and clinical evidence of bronchiectasis syndrome three years after acute exposure to fire smoke in a Caucasian non-smoker asthmatic patient. At the age of 40, he was diagnosed with mild persistent eosinophilic asthma and nasal polyposis and started ICS/LABA (inhaled steroids and long acting beta2-agonist receptor) therapy. Nasal polypectomy was performed three years after asthma onset without any histologic evidence of vasculitis. Family history for pulmonary disease was unremarkable. At the age of 41, in the follow-up of previous papillary thyroid cancer, he underwent a chest high-resolution computed tomography (HRCT), which excluded any pulmonary or bronchial abnormalities. One year later he aided during a house fire where he was exposed to fire burn over 15-minute and he inhaled large amounts of smoke without wearing adequate protective equipment. At the end of the intervention, he did not complain of physical injuries, therefore he didn't seek referral to any physician. Three years later he presented to pneumological visit for worsening of respiratory symptoms, complaining about productive cough, worsening of dyspnoea, wheezing and chest tightness. Chest auscultation revealed inspiratory and expiratory wheezes. Lung function tests showed a mild restrictive ventilatory defect and a mild reduction of DLCO (Diffusion Lung CO), that were not present in previous tests. Chest x-ray showed bilateral opacities. On the hypothesis of asthma exacerbation with pneumonia, the patient was treated with oral corticosteroids and antibiotic therapy, with improvement of symptoms. For diagnostic purposes he repeated a chest HRCT that showed the presence of bilateral, large and saccular bronchiectasis with mucoid impact (Fig. 1). Moreover, it confirmed the presence of left basal pneumonia. To identify the bronchiectasis aetiology, several tests were performed. Blood analysis showed high eosinophil cell count (Eos 1.22 × 10^3/mmc), normal immunoglobulin levels (except for total IgE 218 UI/ml), negative autoimmunity screening (in particular Anti-nuclear antibody (ANA) and Antineutrophil Cytoplasmic Antibodies (ANCA)). No specific IgE for Aspergillus fumigatus were identified. Sweat test was also performed, with a negative result. Bronchoscopy with broncho-alveolar lavage (BAL) and transbronchial biopsies showed non-specific lymphocytic, histiocytic and eosinophilic inflammation, with negative microbiologic findings (including bacterial, mycobacterial and fungal culture, bacterial and virus PCR assays, and galactomannan on BAL). Several sputum cultures were also performed, always with negative results for bacteria, fungi and mycobacteria. In summary, the extensive diagnostic workup excluded immune deficiency, rheumatologic diseases (in particular eosinophilic granulomatosis with polyangiitis), cystic fibrosis, allergic bronchopulmonary aspergillosis, chronic bacterial or mycobacterial infections. In subsequent years the patient reported several episodes of bronchiectasis exacerbation for which he underwent several courses of antibiotic therapy. Radiological follow-up by chest HRCT confirmed the persistence of saccular bronchiectasis (Fig. 1), which remained stable overtime.
There are no standardised criteria for inhalation injury diagnosis, which is usually based on clinical history and findings, with the help of instrumental tests (i.e. HRCT, carboxyhaemoglobin measurement and fiberoptic bronchoscopy).2 Many of the airway consequences of smoke inhalation result from an inflammatory response and they depend on the duration and the magnitude of the exposure, the presence of particulate matter and individual host factors. Many products of combustion, such as halogen acids, formaldehyde, and unsaturated aldehydes act as respiratory irritants.3 Long-term complications have been poorly studied and include bronchiectasis, bronchiolitis obliterans, endobronchial polyposis, tracheal and main bronchial stenosis. These complications have been mainly described as chronic consequences of an acute pulmonary manifestation (i.e. endobronchial steam burns, pneumonia and acute respiratory distress syndrome ARDS).1 It is worth noting that our patient developed clinically significant BE three years after acute smoke exposure, apparently without acute pulmonary manifestations. Few cases like the one presented have been described in the literature. Putman et al.4 analysed radiographic manifestations in a cohort of 21 patients after acute smoke inhalation and noted that one patient subsequentially developed significant chronic lung disease with BE at a 10-months follow-up evaluation. Slutzker et al.5 described a patient with progressive dyspnea and chronic productive cough with multiple exacerbations for 11 years after acute smoke inhalation injury, who was finally diagnosed with saccular bronchiectasis.
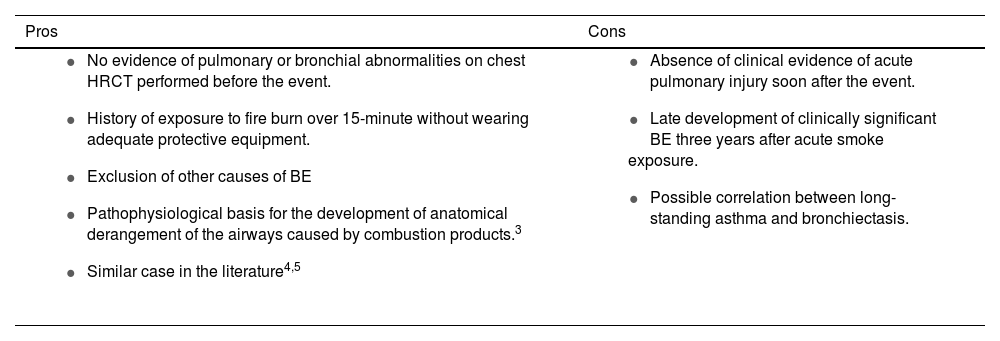
In our patient, some important points should be addressed: first of all, the lack of a medical evaluation soon after the event; second, the possibility of an interrelationship between asthma and bronchiectasis, even in the absence of ABPA. Indeed, long-standing asthma per se might have complicated with bronchiectasis on chest imaging.6,7 However, our patient had normal chest HRCT at baseline. The presence of eosinophilic asthma may have caused predisposition to the development of bronchiectasis in which smoke and irritants inhalation may have acted as a trigger. Arguments in favour and against our hypothesis are summarized in Table 1.
Bronchiectasis as long-term complication of acute fire smoke inhalation: Pros and Cons.
| Pros | Cons |
|---|---|
|
|
Possible interpretation: The presence of eosinophilic asthma may have caused predisposition to the development of bronchiectasis, where smoke and irritants inhalation might have acted as a trigger.
In conclusion, we hypothesise a causal correlation between acute exposure to fire smoke inhalation and development of bronchiectasis as a long-term complication, without any other apparent cause. However more evidence is needed to corroborate our hypothesis.