Chronic obstructive pulmonary disease (COPD) represents an increasing burden worldwide. COPD can no longer be considered a disease which only involves the lungs, its systemic consequences make it an important risk factor for other chronic comorbidities.
AimTo determine the frequency of comorbidities in patients with COPD undergoing a pulmonary rehabilitation program (PRP) and to evaluate the influence of baseline characteristics as well as comorbidities on the outcomes of PRP.
MethodsThe present study included all COPD patients who were admitted to a PRP in our unit. The response to PR was measured by the improvement in exercise tolerance (6min walk test), dyspnea (Mahler's Dyspnea Index) and health status (St. George's Respiratory Questionnaire).
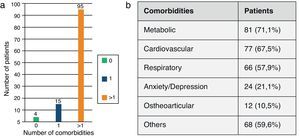
Results114 patients with COPD were included. Most patients (96.5%) had at least one comorbidity. Metabolic diseases (71.1%), cardiovascular diseases (67.5%), other respiratory conditions (57.9%) and anxiety/depression (21.1%) were the most prevalent ones. 64.9%, 64.9% and 51.1% of the patients improved in terms of exercise tolerance, quality of life and dyspnea, respectively.
The overall results were similar in all levels of the disease and in all comorbid subgroups. Logistic regression analysis showed that respiratory failure and ischemic heart disease negatively influenced improvement in health status and anxiety/depression predicted lower improvement in dyspnea.
ConclusionPR was associated with improvements in all comorbid subgroups of patients, underlining the important role of exercise training in rehabilitation of those chronic diseases associated with COPD. On the other hand, the presence of comorbidities in COPD patients, if clinically controlled, should not preclude access to PR.
A doença pulmonar obstrutiva crónica (DPOC) apresenta um impacto crescente a nível mundial. Devido ao seu impacto sistémico, e porque constitui um importante fator de risco para outras comorbilidades crónicas, a DPOC não pode já ser considerada uma doença com envolvimento exclusivamente pulmonar.
ObjetivoDeterminar a frequência das comorbilidades em doentes com DPOC que são submetidos a um programa de reabilitação respiratória (PRR) e avaliar a influência das suas características basais, bem como das suas comorbilidades nos resultados do PRR.
MétodosO presente estudo incluiu todos os doentes com DPOC que foram admitidos na Unidade de Reabilitação Respiratória para um PRR. A resposta à reabilitação respiratória (RR) foi avaliada pela melhoria na tolerância ao exercício (prova de marcha de 6min), na dispneia (índice de dispneia de Mahler) e na qualidade de vida relacionada com a saúde (questionário respiratório de St. George).
ResultadosForam incluídos 114 doentes com DPOC. A maioria dos doentes (96,5%) tinha pelo menos uma comorbilidade. As doenças metabólicas (71,1%), as doenças cardiovasculares (67,5%), outras patologias respiratórias (57,9%) e a ansiedade/depressão (21,1%) foram as mais prevalentes. Apresentaram melhoria na tolerância ao exercício, na qualidade de vida e na dispneia, respetivamente, 64,9, 64,9 e 51,1% dos doentes.
A globalidade dos resultados foi semelhante em todos os estádios da doença e em todos os subgrupos de comorbilidades. A análise por regressão logística demonstrou que a insuficiência respiratória e a doença coronária influenciaram negativamente a melhoria na qualidade de vida relacionada com a saúde, e que a ansiedade/depressão se relacionou com uma melhoria na dispneia menos acentuada.
ConclusãoA RR proporcionou melhoria nos doentes de todos os subgrupos de comorbilidades, salientando o papel fundamental do treino de exercício na reabilitação das doenças crónicas associadas à DPOC. Por outro lado, a presença de comorbilidades em doentes com DPOC, se clinicamente controladas, não deve impedir a sua inclusão na RR.
Chronic obstructive pulmonary disease (COPD) is a disease that is preventable and treatable but nevertheless continues to increase worldwide.1 The prevalence of COPD is increasing due to tobacco smoking, especially in women, and to the aging of the world population, among other factors.2 WHO predicts that COPD will become the third leading cause of death worldwide by 2030.3 Exacerbations and comorbidities contribute to the severity of the disease in individual patients.1
COPD does not affect the lungs exclusively: it is a more complex systemic disease with significant extra pulmonary effects that impact on severity and which is associated with other chronic conditions.4–6 It is estimated that two-thirds of the patients with COPD have one or two comorbidities.7 Arterial hypertension, diabetes mellitus, coronary artery disease, heart failure, respiratory infections and lung cancer are the most common comorbidities described in association with COPD.5 These chronic conditions play an important role in morbidity, representing a significant impact on health status, health care costs and prognoses. In the final analysis, many patients are more likely to die from comorbid disease than COPD itself.8–10 As recently evidenced by Divo et al., some comorbidities, like coronary disease, cancers (lung, esophageal, pancreatic and breast), anxiety, arrhythmia and interstitial pulmonary fibrosis, are independently associated with increased risk of death.11 For these reasons, the treatment of COPD should focus not only on the symptom control and prevention of exacerbations, but it should also be directed to the systemic manifestations and comorbidities.
Pulmonary rehabilitation (PR) is a non-pharmacological intervention that aims to restore the patient to his or her highest functional capacity and to promote social reintegration.12,13 PR is indicated in patients who remain symptomatic despite adequate pharmacologic therapy, at all grades of severity and among all age groups.1 PR should be considered in patients with breathlessness (while walking at their own pace on level ground) and limitation in activities of daily life. PR can improve symptoms, the quality of life, exercise tolerance, physical and emotional participation in everyday activities and it can also reduce healthcare resources utilization.1,12
ObjectivesThe aim of this study was to determine the prevalence of chronic comorbidities in patients with COPD and to evaluate the influence of baseline characteristics as well as comorbidities on the outcomes of PR.
MethodsPatient selectionThis retrospective study included all COPD patients that attended a PRP in our unit in the last 5 years.
The diagnosis and the spirometric classification were based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines.1 Patients with chronic respiratory failure were considered GOLD IV.
The clinical records were reviewed to collect demographic data (age, gender and body mass index), clinical data (smoking history, long-term oxygen therapy – LTOT, non-invasive ventilation – NIV) and diagnostic work-up (imaging, pulmonary function tests, blood gas analysis).
Comorbidities were recorded based on the patients’ clinical records, which included all medical data from different specialties and were duly confirmed by patients’ medication list and diagnostic tests, also available on their medical records.
ComorbiditiesComorbidity is defined as the coexistence of another medical condition alongside COPD, and does not imply causation.
The frequency of each chronic disease and of the combined diseases was established:
- -
cardiovascular (arterial hypertension, heart failure/cor pulmonale, coronary disease, arrhythmia, cerebrovascular disease and peripheral vascular disease),
- -
metabolic (diabetes, dyslipidemia, overweight/obesity),
- -
respiratory (pulmonary tuberculosis sequels, bronchiectasis, obstructive sleep apnea, pulmonary hypertension, interstitial lung disease, lung cancer),
- -
ostheoarticular pathology and
- -
anxiety/depression.
The patients were grouped according to the number of comorbidities (0, 1 and more than one).
Pulmonary rehabilitationAll patients underwent a PRP with optimization of pharmacological therapy and/or LTOT and/or NIV. The patients were also instructed in disease self-management education and in the modification of risk factors, along with psychosocial and nutritional support, breathing techniques and exercise training.
The PRP included 8 weeks of physical training, 3 times a week, under the supervision of a physiotherapist. The target training intensity was set at 80% of the peak work rate attained during a previous cardiopulmonary exercise test. The applied method of training was continuous, the time was steadily increased and loaded according to the degree of dyspnea (4–6 on the modified Borg scale 0–10) and vital signs, or interval training in patients with intense dyspnea. Each training session lasted approximately 30–45min. Patients on LTOT exercised under oxygen administration in order to maintain a SpO2 of at least 90%.
There were no major changes in training protocol according to comorbidities. However, if patients complained of intense breathlessness during exercise sessions, a slower intensity increment and/or interval training was implemented, instead of continuous training. Some comorbidities needed to be more closely monitored, for example blood glucose fast test in diabetes patients, or ECG monitoring in arrhythmias.
The response to PR [minimum clinically important difference (MCID)] was measured by the improvement in exercise tolerance [+30m in the 6min walking distance (6MWD)],14 dyspnea [+1 point on the Mahler Dyspnea Index (MDI)] and health status [−4 points on the St. George's Respiratory Questionnaire (SGRQ)].15,16 It was considered to have had an overall improvement when it occurred in those 3 parameters.
StatisticsData are presented as mean±standard deviation for continuous variables, and frequencies and percentages for categorical variables.
The comparison of variables was made using χ2 test for nominal variables and T student test for quantitative variables.
The significant variables were then entered in a logistic regression model, taking MCID improvement of 6MWD, SGRQ and MDI as dependent variables.
All results were considered statistically significant at p≤0.05.
All statistical analyses were performed using PASW software (version 18; SPSS inc., Chicago, IL, USA).
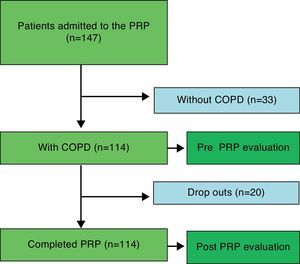
ResultsThis study included 114 patients with COPD, corresponding to 77.6% of all respiratory patients who attended PR in our unit (Fig. 1).
Most patients were male (83.3%) and the average age was 65.8±10.1. Five (4.4%), 35 (30.7%), 19 (16.7%) and 55 (48.2%) were in grade I, II, III and IV of GOLD, respectively. Mean FEV1 was 45.8±16.9% of predicted. The majority of patients (65%) had respiratory failure, with a predominance of hypoxemic respiratory failure. Forty-four (38.6%) patients were on LTOT and ten (8.8%) on NIV (Appendix Table 1).
Distribution according to number and group of comorbidities is shown in Fig. 2. Overweight/obesity (63.2%) was the most prevalent comorbidity, followed by hypertension (50.9%), pulmonary tuberculosis sequels (23.7%), anxiety/depression (21.1%), heart failure/cor pulmonale (20.2%), bronchiectasis (20.2%), dyslipidemia (19.3%) and ischemic heart disease (12.3%) (Appendix Table 2).
Among these 114 patients with COPD, 20 did not conclude the PRP. The causes of PRP withdrawal were hospitalization with exacerbations, psychiatric disorders and non-compliance with the program. There were no significant differences in baseline characteristics and comorbidities between subjects who completed the PRP and the ones who dropped out (Appendix Tables 1 and 2).
Of all the patients who concluded PRP, 64.9%, 64.9% and 51.1% improved beyond the MCID for 6MWD, SGRQ and MDI, respectively (Table 1). Only ten (10.6%) patients did not improve in any parameter and 24 (25.5%) patients reported a positive change in all 3 outcomes.
There were no statistically significant correlations between the number of comorbidities (0, 1 and more than one) and PRP outcomes (Table 1).
However, there was a significant correlation between some baseline characteristics and comorbidities and improvement in health status, dyspnea and exercise tolerance.
Respiratory failure was inversely correlated with improvement in health status (p=0.001; OR=0.17) and in overall improvement (p=0.025; OR=0.33). Being on LTOT was inversely correlated with improvement in dyspnea (p=0.016; OR=0.313), in exercise tolerance (p=0.012; OR=0.32) and in overall improvement (p=0.05; OR=0.337). Patients with lower arterial carbon dioxide tension (p=0.016) and higher baseline SGRQ score (p=0.006) had a more pronounced improvement of dyspnea. Patients with lower FEV1/FVC (p=0.01) had less improvement in exercise tolerance and those with lower DLCO had less improvement in exercise tolerance (p=0.032) and in dyspnea improvement (p=0.05) (Appendix Table 3).
In terms of comorbidities, ischemic heart disease correlated inversely with improvement in health status (p=0.003; OR=0.142), anxiety/depression with improvement in dyspnea (p=0.012; OR=0.247), bronchiectasis correlated positively with improvement in dyspnea (p=0.04; OR=3.843) and dyslipidemia with improvement in exercise tolerance (p=0.013; OR=5.86) (Appendix Table 4).
Significant variables were then entered into logistic regression model (Table 2). Respiratory failure and ischemic heart disease negatively influenced improvement in health status. Anxiety/depression predicted a lower improvement in dyspnea.
Factors predicting PRP outcomes.
| Dependent variables | Variables | B | SE | OR | 95% CI | p | |
| Less | Upper | ||||||
| Exercise tolerance improvement | LTOT | −0.452 | 0.616 | 0.636 | 0.190 | 2.121 | 0.463 |
| Dyslipidemia | 1.520 | 0.823 | 4.573 | 0.911 | 22.954 | 0.065 | |
| FEV1/FVC | −0.049 | 0.028 | 0.952 | 0.902 | 1.005 | 0.073 | |
| DLCO | −0.017 | 0.016 | 0.983 | 0.952 | 1.014 | 0.279 | |
| Quality of life improvement | Respir. failure | −1.1588 | 0.608 | 0.204 | 0.062 | 0.673 | 0.009 |
| Ischemic heart disease | −1.632 | 0.747 | 0.196 | 0.045 | 0.846 | 0.029 | |
| Dyspnea improvement | LTOT | −1.463 | 0.754 | 0.232 | 0.053 | 1.015 | 0.52 |
| Bronchiectasis | 1.959 | 1.126 | 7.090 | 0.780 | 64.477 | 0.082 | |
| Anxiety/Depression | −2.357 | 0.921 | 0.095 | 0.016 | 0.576 | 0.011 | |
| PaCO2 | 0.119 | 0.067 | 1.127 | 0.988 | 1.285 | 0.076 | |
| DLCO | −0.016 | 0.018 | 0.984 | 0.949 | 1.020 | 0.373 | |
| SGRQ | 0.03 | 0.025 | 1.031 | 0.982 | 1.082 | 0.224 | |
| Overall improvement | LTOT | −0.580 | 0.715 | 0.56 | 0.138 | 2.275 | 0.417 |
| Respir. failure | 0.778 | 0.631 | 0.459 | 0.133 | 1.582 | 0.218 | |
LTOT, long term oxygen therapy; FEV1, forced expiratory volume in one second; FVC, forced vital capacity; PaCO2, arterial carbon dioxide tension; DLCO, diffusion lung capacity for carbon monoxide; SGRQ, St. George's Respiratory Questionnaire.
This study confirms that comorbidities are prevalent among COPD patients who are referred to PRP. Other authors, like Mapel and colleagues, found an average of 3.7 comorbidities in COPD patients compared with 1.8 in healthy controls.17
The most common conditions associated with COPD were cardiovascular diseases, other respiratory diseases and anxiety/depression, similar to what has been described in the literature.5,11 Following overweight/obesity, arterial hypertension was the second most prevalent comorbidity in our sample, and the first one found by Divo et al.11 On the other hand, a significant number of our patients presented comorbidities associated by these authors with a major risk of mortality, such as congestive heart failure, coronary artery disease and anxiety.11
The association with cardiovascular diseases is already known.18 FEV1 is an independent predictor of death from myocardial infarction. Systemic arterial stiffness is a good predictor of vascular disease19 and is increased in COPD. The presence of systemic inflammation accelerates coronary atherosclerosis, resulting in ischemia. Thus, COPD is an independent risk factor for coronary disease.18
Approximately 40–50% of individuals of 60 years or more in industrialized countries meet the criteria for metabolic syndrome.20 This syndrome represents a cluster of risk factors (abdominal obesity, atherogenic dyslipidemia, hypertension and insulin resistance) that predispose patients to systemic inflammation, cardiovascular disease and physical inactivity, and frequently coexist with COPD.20–22
Other respiratory diseases were frequently identified in our patients. The high frequency of pulmonary tuberculosis sequels and bronchiectasis reflects the fact that tuberculosis is still common in Portugal, although it has decreased in recent decades.23,24 On the other hand, prevalence of obstructive sleep apnea is probably due to the fact that a large part of the studied population is overweight.
Anxiety/depression is a highly prevalent comorbidity in COPD. Hill et al. also concluded that over 42% of COPD patients had symptoms of anxiety/depression.25 It is known that anxiety/depression is related with the degree of dyspnea and feeling of incapacity in COPD patients. Dyspnea is the most disturbing symptom that causes patients to reduce physical activity in order to avoid it. This leads to a sedentary existence, with less emotional and physical involvement in the activities of daily life, and to the worsening of health status as well as to isolation. Anxiety and depression are associated with higher morbidity of COPD, with worse quality of life, more dyspnea, an increase in the utilization of healthcare resources and even higher mortality.26 Previous studies show negative impact of anxiety/depression on 6MWD and quality of life.27,28 Similarly we found that anxious/depressed patients present lower improvement in dyspnea.
Patients with ischemic heart disease showed less gain in health status. Crisafulli et al. also concluded that cardiac pathology was inversely related with improvement of health status.29 Dyspnea, fatigue and reduced muscle strength may explain a lower quality of life in these patients. Vanfleteren et al. concluded that ischemic ECG changes are common in patients with COPD and are associated with poor clinical outcomes in PRP.30 However, rehabilitation has well known benefits in patients with coronary heart disease and chronic heart failure, such as the improvement in functional capacity, prognosis and well-being.31
The prevalence of at least one comorbidity in our cohort was higher (96.5%) than the prevalence reported in other studies (65%, Crisafulli et al.29), but similar to what Mapel documented (only 6% of patients with COPD did not have another chronic medical condition17).
The high prevalence of comorbidities in our sample can be explained by the fact that the majority of patients had a history of smoking, an average age of over 60 years and a predominance of grade IV COPD, all factors that contribute to a more pronounced systemic inflammation. Systemic inflammation is a common potential mechanism shared by several COPD systemic consequences and comorbidities.5,32–35
The outcomes of PRP were similar across the comorbidity categories (0, 1 and more than one), contrary to what was reported by Crisafulli et al.29; he reported that benefits in dyspnea and quality of life were higher in those with fewer comorbidities. However, it should be said that the present study has a limitation concerning the number of patients without comorbidities. This number is very small, and there is an important sample size difference between the comorbid subgroups (4 patients – 0 comorbidities; 15 patients – 1 comorbidity; 95 patients – >1 comorbidity) which mitigates against reaching a definite conclusion on the impact of comorbidities in PRP outcomes in this particular patient population. This limitation might have been solved if there had been a larger patient sample.
Almost half (48.2%) of our patients were GOLD IV and only 16.7% were GOLD III. Even though this is not the usual severity distribution observed in PRP in most centers, this difference may be explained by the fact that our Respiratory Rehabilitation Unit also admits patients after acute exacerbations with respiratory failure (65%). The authors included patients with chronic respiratory failure in GOLD IV, as classified in GOLD guidelines previous to 2011. Although in our sample we have a predominance of GOLD stage IV patients, there were no statistically significant differences in the PRR outcomes concerning spirometric degrees of COPD, reflecting the benefits at all grades of severity.
We noted that 83% of our sample was composed of men, and this is not the typical gender distribution observed in PRP in most centers. However, COPD in Portugal is more prevalent in men (18.7% versus 10.5%).36
However, the comorbidities (both their number and their type) did not differ between male and female patients (data not shown).
Some baseline characteristics correlated with the outcomes. Patients with respiratory failure presented a smaller gain in health status. Hypoxemia might cause a low anaerobic threshold during exercise, which determines an early increase of breathing frequency, with a consequent increase in dynamic hyperinflation, a greater degree of dyspnea and a major limitation in activities of daily life, which, in turn, leads to further deconditioning and sedentarism.37,38
Despite the correlations described, patients with COPD and other chronic conditions are not poor candidates for PR and it does not necessarily mean they will improve less. All patients can benefit from PR, which is a holistic therapeutic approach of COPD, and the benefits of exercise training in several comorbidities are already known.39
ConclusionsIn patients with COPD, comorbidities are important determinants of health status and prognosis.
Our study confirms that most patients referred to PRP present one or more comorbidities, including metabolic, cardiovascular, respiratory, anxiety/depression and ostheoarticular pathology.
Management of patients with COPD should include the active identification of comorbidities, in order to optimize the therapeutic strategy. PR is a holistic approach that not only deals with respiratory symptoms, but also with systemic effects.
Although some conditions such as respiratory failure and ischemic heart disease may reduce the impact of rehabilitation benefits, this study emphasizes that comorbidities, either alone or in combination, if clinically controlled, do not preclude access to rehabilitation.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
AuthorshipAlexandra Carreiro collected and analyzed data (including a statistical analysis), and wrote the draft text.
Joana Santos collected and analyzed data and collaborated in the writing up of the text.
Fátima Rodrigues conceived the study, collected data, conducted its analysis and supervised all aspects of the work.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Carreiro A, et al. Impacto das comorbilidades num programa de reabilitação respiratória em doentes com DPOC. Rev Port Pneumol. 2013. http://dx.doi.org/10.1016/j.rppneu.2012.12.004.