Non-small cell lung cancer (NSCLC) accounts for approximately 85% of all cases of lung cancer. In spite of the progress achieved in treatments, patients with advanced disease still have a poor prognosis. Prognostic evaluation in cancer is a challenging process. Features such as age, gender, histopathology and stage are known prognostic factors, but are not enough to explain the global prognosis.1 Therefore, new prognostic markers are needed. The use of biological markers easily collected through a simple method like a peripheral blood sample is appealing. The ideal biomarker should have a long half-life, be measured precisely by an inexpensive and simple test, and be sensitive to change so that it can be followed over time. C-reactive protein (CRP) and neutrophil-to-lymphocyte ratio (NLR) meet these criteria and elevated levels of these biomarkers have been linked to poor prognosis in several cancers.2
The aim of this work was to evaluate the relationship between CRP and NLR values at the time of diagnosis and the overall survival (OS) in patients with NSCLC at stages IIIB and IV.
We performed a retrospective study that included patients diagnosed with NSCLC at stages IIIB and IV (based on the tumor-node-metastasis classification, 7th edition) between January 2012 and March 2016, who were treated with palliative systemic therapy. Patients with clinical evidence of infection at the time of diagnosis were excluded since infection is a non-cancer inflammatory marker-modifying factor. CRP and NLR values at the time of diagnosis and other clinical variables were retrieved from patients’ medical records. The NLR ratio was calculated dividing the absolute neutrophil count by the absolute lymphocyte count. In accordance to previous studies,3,4 a cut-off value of 3.5 was evaluated as a potential prognostic biomarker. The cut-off value of CRP varies among different studies, but a systematic review verified that 10mg/L was the most frequently selected.2 Accordingly, we adopted this value as cut-off.
Kaplan–Meier analysis with log-rank test was performed to calculate median OS. Univariate and multivariate analyses for OS were performed using the Cox proportional hazards model and was expressed as hazard ratios (HRs) and 95% confidence intervals (CIs). A p-value <0.05 was considered statistically significant. Statistical analyses were performed using SPSS® for Windows® (version 24.0, Chicago, Illinois).
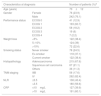
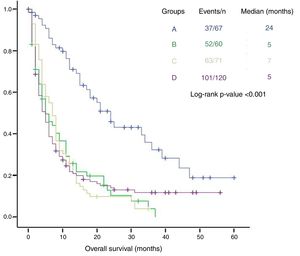
Patient characteristics are shown in Table 1. From a total of 569 patients diagnosed with NSCLC, 318 fulfilled the required criteria, 262 (82.4%) of which at stage IV. Most patients had increased values of CRP (60.1%) or NLR (56.6%) at the time of diagnosis. Male gender, loss of 5% or more of body weight before diagnosis, an Eastern Cooperative Oncology Group (ECOG)≥2, NRL>3.5 and CRP>10mg/L were significantly associated with worse OS (Table 2). NLR and CRP were independent prognostic factors for OS when adjusted by the other clinical factors. Patients with NLR>3.5 had increased risk of death (HR 1.350; 95% CI 1.036–1.760; p=0.026). The same was verified with CRP, with values >10mg/L predicting worse survival (HR 1.462; 95% CI 1.113–1.920; p=0.006). Among the other clinical variables, ECOG≥2 and male gender also independently predicted worse survival. The two biomarkers were then combined to obtain four subgroups: group A with decreased values of both markers (67 patients), group B with CRP≤10mg/L and NLR>3.5 (60 patients), group C with CRP>10mg/L and NLR≤3.5 (71 patients), and group D with both markers increased (120 patients). Patients from group A had a median survival of 24 months, significantly higher than those with at least one increased biomarker (p<0.001). Patients from groups B, C and D had similar median survival times (5, 7 and 5 months, respectively, p>0.05) (Fig. 1).
Clinicopathological features at diagnosis.
| Characteristics at diagnosis | Number of patients (%)a | |
|---|---|---|
| Age (years) | 70±12 | |
| Gender | Female | 76 (23.9) |
| Male | 242 (76.1) | |
| Performance status | ECOG 0 | 41 (12.9) |
| ECOG 1 | 193 (60.7) | |
| ECOG 2 | 58 (18.2) | |
| ECOG 3 | 19 (6) | |
| ECOG 4 | 7 (2.2) | |
| Weight loss | <5% | 122 (38.4) |
| 5–10% | 124 (39) | |
| >10% | 72 (22.6) | |
| Smoking status | Never smoker | 78 (24.5) |
| Ex-smoker | 118 (37.1) | |
| Current smoker | 122 (38.4) | |
| Histopathology | Adenocarcinoma | 215 (67.6) |
| Squamous cell carcinoma | 67 (21.1) | |
| Others | 36 (11.3) | |
| TNM staging | IIIB | 56 (17.6) |
| IV | 262 (82.4) | |
| NLR | ≤3.5 | 138 (43.4) |
| >3.5 | 180 (56.6) | |
| CRP | ≤10mg/L | 127 (39.9) |
| >10mg/L | 191 (60.1) | |
Prognostic factors for overall survival estimated by univariate and multivariate Cox regression analyses.
| Characteristics | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Male gender | 1.553 | 1.146–2.105 | 0.003 | 1.408 | 1.032–1.921 | 0.031 |
| Ever smoker | 1.150 | 0.866–1.528 | 0.335 | |||
| ECOG≥2 | 1.897 | 1.451–2.480 | <0.001 | 1.711 | 1.289–2.272 | <0.001 |
| Weight loss≥5% | 1.348 | 1.043–1.741 | 0.022 | |||
| NSCLC other than adenocarcinoma | 1.211 | 0.934–1.571 | 0.148 | |||
| NLR>3.5 | 1.694 | 1.315–2.183 | <0.001 | 1.350 | 1.036–1.760 | 0.026 |
| CRP>10mg/L | 1.766 | 1.361–2.291 | <0.001 | 1.462 | 1.113–1.920 | 0.006 |
CRP – C-reactive protein; ECOG – Eastern Cooperative Oncology Group; HR – hazard ratio; NLR – neutrophil–lymphocyte ratio; NSCLC – non-small cell lung cancer.
Statistically significant values are in bold.
Several studies have demonstrated a relationship between CRP and NLR values and survival in cancer patients.2,3 It has been reported that inflammation could facilitate cancer development and is associated with a worse outcome.5 Systemic inflammation can be accessed by NLR and CRP blood levels, two minimally invasive and inexpensive biomarkers.2
We observed that the presence of NRL>3.5 or CRP>10mg/L was independently associated with shorter OS. We found no cumulative effect on OS when both biomarkers are increased. Besides, each of these markers increases the hazard of death in the same magnitude. Our results suggest that it is the presence of inflammation in lung cancer that is associated with worse prognosis, rather than the marker chosen for its evaluation. Cancer-related inflammation affects many aspects of cancer including proliferation and survival of tumor cells, angiogenesis, metastization and tumor response to therapy.6 Previous studies have also evaluated this association between increased inflammation and worse survival in lung cancer. As in ours, the majority have identified increased values of NLR or CRP to be associated with worse OS.1,2,7
These results highlight the importance of routinely assessing the presence of systemic inflammation as a part of the global approach of patients with lung cancer.
We recognize some limitations in our study. First, it is a retrospective and single center study, with inherent selection bias. Second, although patients with evidence of infection were excluded, we cannot ensure that other non-cancer CRP and NLR modifying factors were present. Third, mutational status and treatment regimens were not reported and may have influenced results.
In conclusion, the results of this study demonstrated that CRP and NLR are independent prognostic factors for advanced stage NSCLC patients, but additional studies are necessary to assess if long term monitoring of these biomarkers will be helpful in outcomes evaluation.
Funding sourcesThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interestDr. Barroso reports personal fees from AstraZeneca, Boehringer Ingelheim, Lda, Eli Lilly and Company, Pierre Fabre Portugal, Roche Farmacêutica Química, Lda, Merck and Bristol-Myers Squibb, outside the submitted work. The other authors have no conflicts of interest to declare.
None.