Long-term domiciliary ventilation has been a growing therapeutic option in children, namely in children with special and complex health care needs. For this reason, multidisciplinar outpatient clinics became necessary. Authors’ goal was to describe the organizational model of an integrated domiciliary ventilation paediatric outpatient clinic (IDVC), describing its first 6 years of experience with a retrospective methodology.
Integrated Domiciliary Ventilation Outpatient Clinic was created in 2009 at Centro Hospitalar do Porto's Paediatric Department in Portugal. A paediatric pulmonologist (IDVC coordinator), a nurse and a physiotherapist with specialize education in paediatric pulmonology have been the core IDVC working group. Starting in the hospital evaluation, general patient assessment is done (in coordination with various medical specialities, optimizing hospital visits), respiratory monitoring support equipment is adjusted and caregivers are trained in the needed domiciliary care. Since 2012 it is also possible to start long-term ventilation in the outpatient setting, followed by a close monitoring at home. Individual follow-up care plan is performed in coordination with institutions available near home in permanent cooperation with the domiciliary team. This team is formed by health professionals trained in respiratory problems and is coordinated by IDVC physiotherapist. They perform periodic and urgent assessments at home, providing expert technical support and monitoring respiratory therapies, which strengthens therapeutic adhesion and enables a rapid and efficient approach to exacerbations and ventilation problems. The physiotherapist presence at the hospital evaluation allows integration of technical and monitoring data with the clinical assessment leading to a rapid and dynamic flow of information.
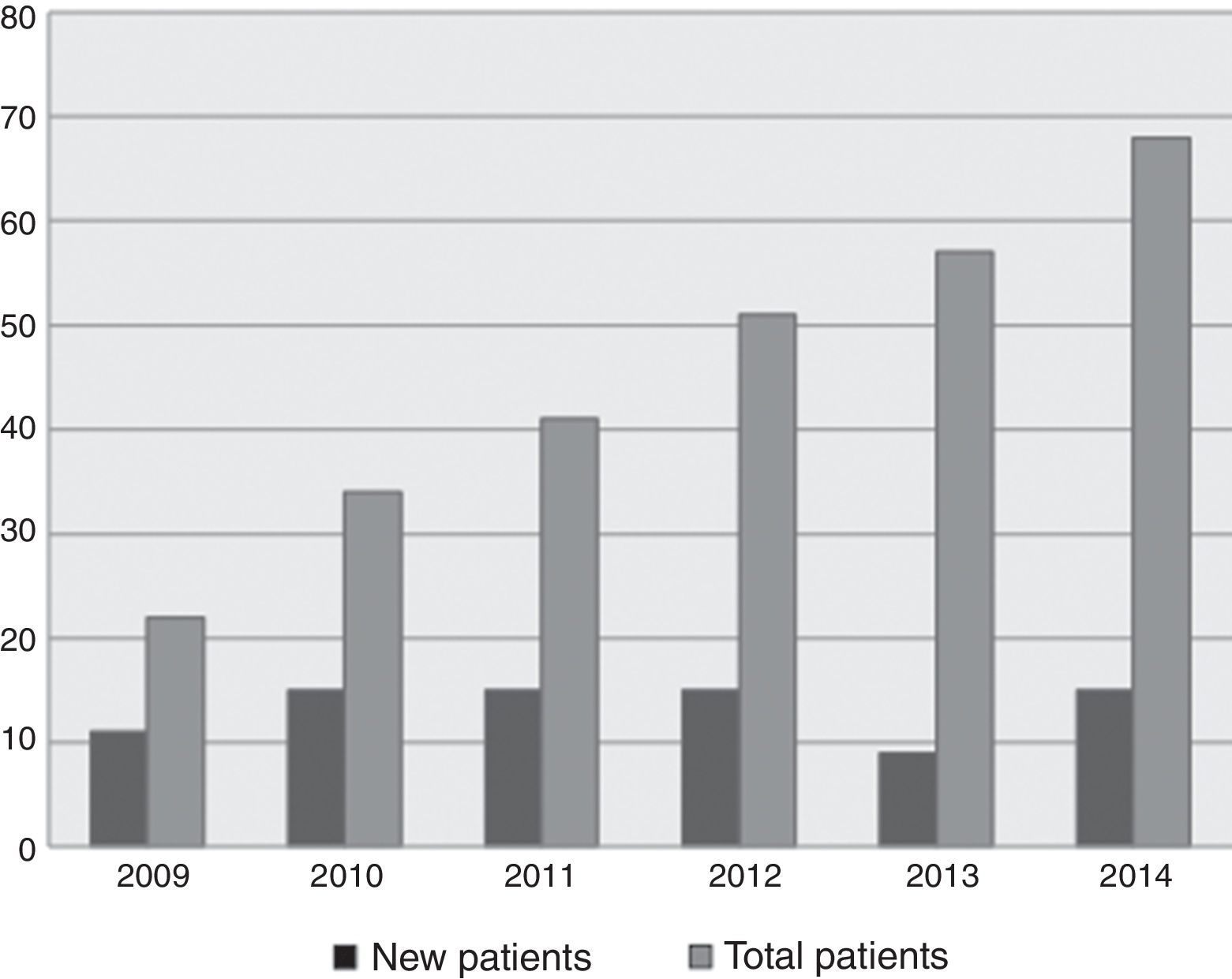
Between 2009 and 2014, 93 paediatric patients were followed at IDVC and ventilation initiated in 80 patients (9–15 new patients/year) – Fig. 1. The majority were male (58%) with neuromuscular disease (35.5%), malformative syndrome (24.7%) or cerebral palsy (20.4%). Noninvasive ventilation (NIV) was used in 95% of patients. Ventilation had palliative goal in 90.3%, was initiated at 8.1±6 years of age, with elective indication in 61%. Elective ventilation was started at hospital setting in 42 patients and outpatient setting in 15 patients since 2012. Patients under domiciliary ventilation also were provided with respiratory therapeutic equipment at home: in-exsufflater, oximeter, respiratory secretions suction device, oxygen therapy, nebulizer and glossopharyngeal breathing. During follow-up (3.1±2.8 years, maximum 12.5 years), 55.9% had no hospitalizations and 41.9% had less than two hospital stays/year. No major complications related with ventilation requiring its withdraw were described.
The exponential ventilation use in paediatric chronic patients in our IDVC follows the international trend during the last decade in developed countries,1,2 mainly by an increase of NIV. We report a higher percentage of patients under domiciliary NIV than most centers. Noninvasive ventilation advantages include lower infection risk, more independence and less vocal commitment.3
There was a reduced need of hospital admission for ventilation adaptation, which can be related to a better use of resources available in the hospital and community and the efficient home monitoring provided by the IDVC program. Ambulatory ventilation adaptation benefits have not been studied in children, but studies in adults have proven similar clinical efficacy while reducing the economic costs by 50–70%.4,5
In most of our cases there was a low number of hospital admissions (0.5 hospital admission/patient/year) in spite of patients’ disease complexity, as has been reported in other centres with paediatric multidisciplinary ventilation clinics (0.17–1.6 hospital admissions/patient/year in different demographic and clinic groups of paediatric patients).6,7
Close cooperation between patient, his family and a specialized group of health care professionals can improve clinical outcomes. Domiciliary care and monitoring in continuum with hospital multidisciplinar assessments might improve respiratory care for chronic paediatric patients needing domiciliary ventilation. Outpatient clinic models, like the IDVC described, can be integration tools between home and hospital care.
Conflicts of interestThe authors have no conflicts of interest to declare.