Maintaining the benefits of pulmonary rehabilitation (PR) in the long-term is challenging.1 Community-based physical activity (PA) programmes have emerged as promising strategies to extend these benefits, accommodating different PA facilitators (e.g., supervision, peer support, accessibility, or adequate equipment/infrastructures).2-4 In addition, community-based PA programmes enable individuals to integrate PA modalities according to their preferences and needs. Nevertheless, community-based PAs should be safe and of at least moderate intensity to align with the PA guidelines.5
We examined safety and the intensity level of different community-based PAs in people with COPD who had completed a PR programme.
This observational cross-sectional study, part of two larger trials (PICk UP - NCT04223362, CENTR(AR) - NCT04711057), was approved by the Ethics Committees of Centro Hospitalar do Baixo Vouga (Ref.15–05–2019), Unidade Investigação em Ciências da Saúde – Enfermagem (Ref.P620–10/2019), and Administração Regional de Saúde do Centro (Ref.16/2020). All participants provided informed consent. Privacy policy followed the European Union General Data Protection Regulation 2016/679.
People with stable COPD with a positive risk-benefit analysis (the PA attributes aligned with their characteristics and needs) conducted by the healthcare professionals, who advised their inclusion in community-based PAs, were recruited from five community-based PR programmes. Further details regarding the risk-benefit analysis are provided within the supplementary material. Participants were given a list of available PAs (Table 1 of the supplementary material) and could select those they wanted to try.
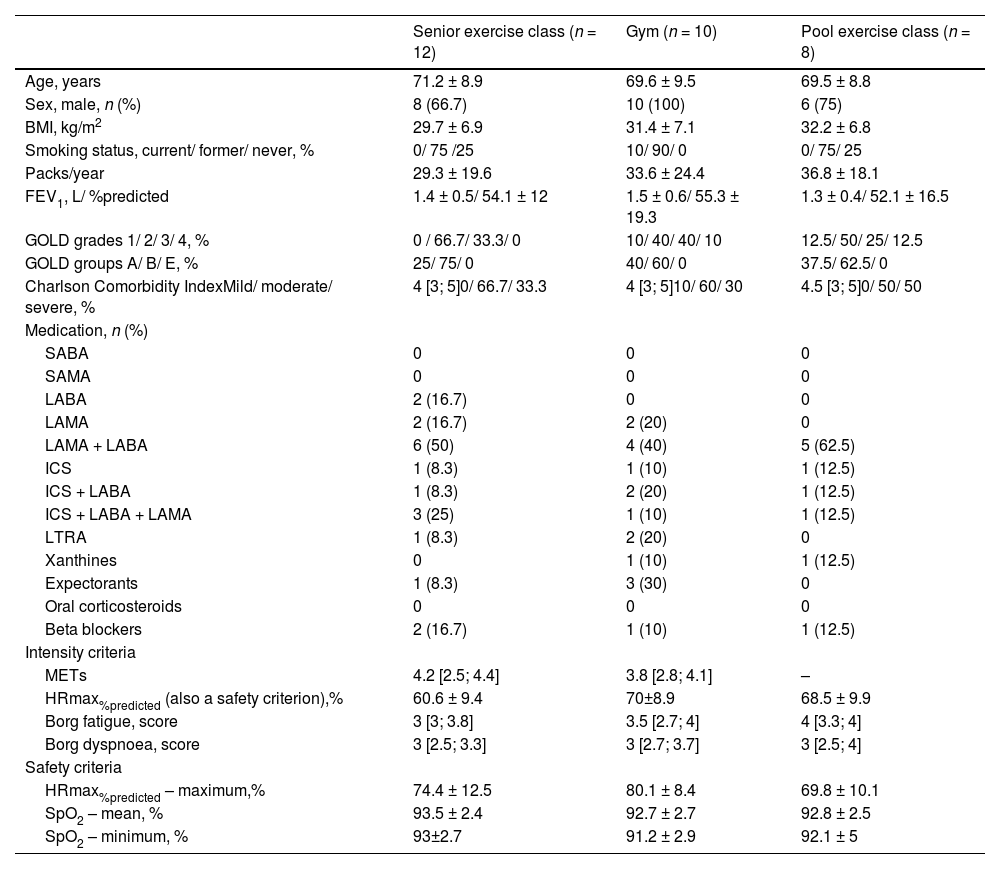
Participants’ characteristics as well as results of intensity and safety criteria per type of community-based physical activity.
Values are presented as n (%), mean±standard deviation or median [interquartile range], unless otherwise stated. Due to technical problems, metabolic equivalent tasks were missing in two participants of the senior exercise classes and in one participant integrating gym.
Legend: BMI: body mass index; FEV1: forced expiratory volume in one second; GOLD: Global Initiative for chronic obstructive lung disease; HRmax%predicted: maximum HR percentage predicted; ICS: inhaled corticosteroid; LABA: long-acting beta-agonists; LAMA: long-acting muscarinic antagonist; LRTA: leukotriene receptor antagonist; METs – metabolic equivalent tasks; SABA: short-acting beta-agonists; SAMA: short-acting muscarinic antagonist; SpO2: percentage of peripheral oxygen saturation.
Intensity and safety of the community-based PAs were assessed based on data collected from a single exercise session. Heart rate (HR, Polar H10) and percentage of peripheral oxygen saturation (SpO2, WristOx2®3150) were continuously monitored during the community-based PAs. Participants’ perception of dyspnoea and overall fatigue were assessed every 20-minutes with the modified Borg 0–10 scale. PAs Metabolic Equivalent Tasks’ (METs) were estimated using a SenseWear Armband worn by participants during the entire exercise sessions. Due to equipment constraints SenseWear was not used during pool exercise classes.
Intensity of community-based PAs was determined based on four criteria:
- i.
METs: light≤2.9; 3≤moderate≤5.9; vigorous≥6.6
- ii.
maximal HR percentage predicted (HRmax%predicted): light≤63; 64≤moderate≤76. vigorous≥77,6 using averaged values collected every 1-second; HRmaxpredicted=220-age.
- iii.
iii-iv) dyspnoea and fatigue Borg scores: light≤2; 3≤moderate≤6; vigorous≥7,6,7 using averaged scores collected every 20 min.
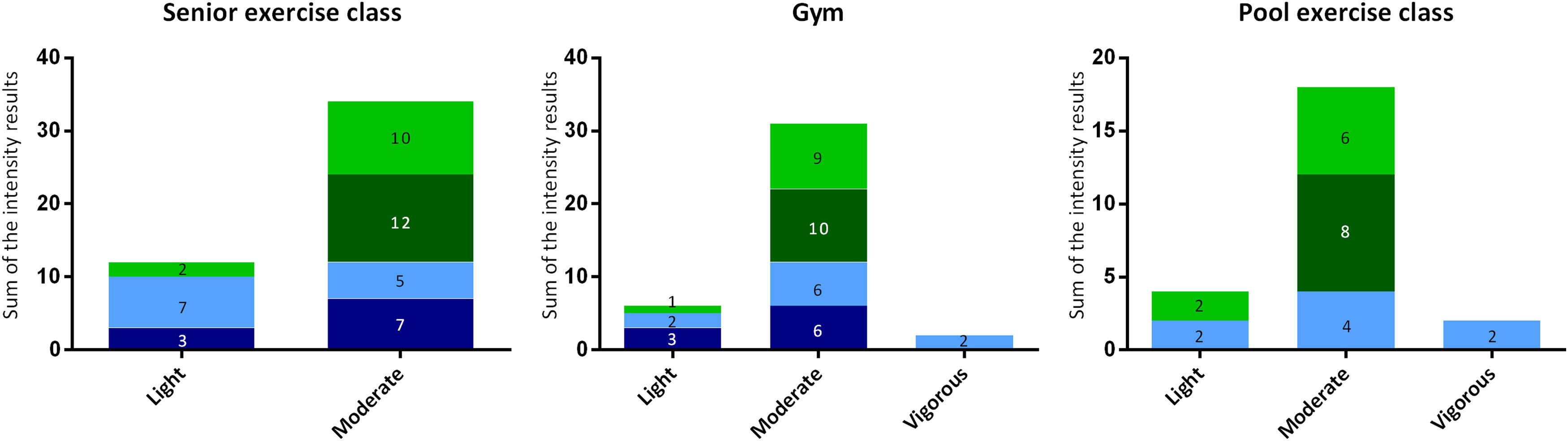
The final PA intensity level was obtained by summing the number of participants categorized within each intensity level (light, moderate and vigorous) according to the four intensity criteria (equally weighted). Safety of community-based PAs was assessed based on SpO2 and HRmax%predicted. Average and minimum values of SpO2, and average and maximum values of HRmax%predicted were computed for each participant during PAs. Occurrences of SpO2<88 %, HRmax%predicted>85 % or any adverse events during the PAs were registered.
Descriptive analyses were conducted. For intensity criteria, absolute frequencies were used and summation presented in bar plots. For safety criteria, mean and 95 % confidence intervals [CI] were displayed. Data analysis was performed using SPSS v.29.0.0.0 and graphs were created using GraphPad Prism 6.
Thirty-two individuals were recruited for this study and 21 agreed to participate. Within these, twelve participants attended senior exercise classes, 10 the gym, and eight pool exercise classes. Participants’ characteristics are presented in Table 1.
All community-based PAs were classified as moderate intensity (Fig. 1). During gym, one participant desaturated below 88 %, reaching a minimum of 86 % but recovered within one minute. The 85 % of the HRmax%predicted threshold was surpassed by two participants at the gym (during 58 and 106 s reaching maximum HRmax%predicted of 94 and 89 %, respectively) and by two participants at the senior exercise classes (during 22 and 160 s reaching maximum HRmax%predicted of 88 and 91 %, respectively). No adverse events were registered, however, due to fatigue one participant had to rest once during gym (two minutes) and twice during the senior exercise class (one and two minutes). Intensity and safety criteria results are presented in Table 1.
Intensity level of community-based physical activities (senior exercise classes [n = 12], gym [n = 10], and pool exercises classes [n = 8]) in people with COPD. Bar graphs represent the sum of the intensity results, i.e., sum of the number of participants categorized within each intensity level (light, moderate and vigorous), according to the four intensity criteria (METs, maximal heart rate percentage predicted [mean values] and dyspnoea and fatigue Borg scores). For each community-based physical activity modality, the total possible sum of intensity results was obtained by multiplying the number of participants by the number of intensity criteria used (senior exercise classes: 12×4 = 48; gym: 10×4 = 40; and pool exercise classes: 8 × 3 = 24). Due to technical problems, METs were missing in two participants of the senior exercise classes (46 intensity results) and in one participant integrating gym (39 intensity results). Within each coloured rectangle are represented the number of participants categorized according to that intensity criteria in that physical activity intensity level (e.g., within the 12 participants included in the senior exercise classes, according to the Borg dyspnoea criteria [light green], 10 fell within the moderate intensity level and 2 within the light intensity level). Graphs should be read as follows, e.g., in the pool exercise classes, within the 24 intensity results obtained, 18 (6 + 8 + 4) fell within the moderate intensity level, 4 (2 + 2) within the light intensity level and 2 within the vigorous intensity level.
Legend: HRmax %predicted: maximum HR percentage predicted; METs – metabolic equivalent tasks.
Senior, gym and pool exercise classes seem to be safe and of moderate intensity for people with COPD.
Previous studies have found that similar structured senior, gym, or pool exercise classes were safe,8,9 with comparable intensity levels reported for aquatic exercises.8
Some limitations must be recognized. This was a secondary analysis of larger trials, and no sample size calculation was previously conducted. Our sample included mainly elderly, overweight males with moderate COPD severity and a lower risk of exacerbations. Intensity of PA is influenced by all these individual factors.10 Additionally, participants were recruited from community-based PR programmes, thus, our results may not be valid for people with COPD recruited from hospital-based programmes, as the disease severity and complexity are likely to differ.11 Although three relative intensity criteria were used, future studies with larger and more heterogenous samples are needed. Pooling PA intensity by using different criteria is a strength of this study, as formal guidance on how to assess intensity of community-based PAs is still lacking.12 To the best of our best knowledge this was the first study assessing intensity of different community-based PA modalities in COPD, in real world settings.
Following PR, based on a careful patient selection, healthcare professionals can now advise people with COPD to integrate gym, senior or pool exercise classes, as these seem to be safe, of moderate intensity, and may enhance long-term maintenance of PR benefits.
CRediT authorship contribution statementP.R., D.B. and A.M. - conceptualization; P.R., A.T., R.P. and C.S. - data curation; P.R., D.B. and A.M. - formal analyses, investigation and methodology; AM and PR – funding acquisition; AM – Project administration; AM and DB – Supervision; PR – Writing - original draft; P.R., A.T., R.P., C.S., DB and AM – Writing review and editing.
Data availability statementData are available upon reasonable request to the corresponding author.



![Intensity level of community-based physical activities (senior exercise classes [n = 12], gym [n = 10], and pool exercises classes [n = 8]) in people with COPD. Bar graphs represent the sum of the intensity results, i.e., sum of the number of participants categorized within each intensity level (light, moderate and vigorous), according to the four intensity criteria (METs, maximal heart rate percentage predicted [mean values] and dyspnoea and fatigue Borg scores). For each community-based physical activity modality, the total possible sum of intensity results was obtained by multiplying the number of participants by the number of intensity criteria used (senior exercise classes: 12×4 = 48; gym: 10×4 = 40; and pool exercise classes: 8 × 3 = 24). Due to technical problems, METs were missing in two participants of the senior exercise classes (46 intensity results) and in one participant integrating gym (39 intensity results). Within each coloured rectangle are represented the number of participants categorized according to that intensity criteria in that physical activity intensity level (e.g., within the 12 participants included in the senior exercise classes, according to the Borg dyspnoea criteria [light green], 10 fell within the moderate intensity level and 2 within the light intensity level). Graphs should be read as follows, e.g., in the pool exercise classes, within the 24 intensity results obtained, 18 (6 + 8 + 4) fell within the moderate intensity level, 4 (2 + 2) within the light intensity level and 2 within the vigorous intensity level. Legend: HRmax %predicted: maximum HR percentage predicted; METs – metabolic equivalent tasks. Intensity level of community-based physical activities (senior exercise classes [n = 12], gym [n = 10], and pool exercises classes [n = 8]) in people with COPD. Bar graphs represent the sum of the intensity results, i.e., sum of the number of participants categorized within each intensity level (light, moderate and vigorous), according to the four intensity criteria (METs, maximal heart rate percentage predicted [mean values] and dyspnoea and fatigue Borg scores). For each community-based physical activity modality, the total possible sum of intensity results was obtained by multiplying the number of participants by the number of intensity criteria used (senior exercise classes: 12×4 = 48; gym: 10×4 = 40; and pool exercise classes: 8 × 3 = 24). Due to technical problems, METs were missing in two participants of the senior exercise classes (46 intensity results) and in one participant integrating gym (39 intensity results). Within each coloured rectangle are represented the number of participants categorized according to that intensity criteria in that physical activity intensity level (e.g., within the 12 participants included in the senior exercise classes, according to the Borg dyspnoea criteria [light green], 10 fell within the moderate intensity level and 2 within the light intensity level). Graphs should be read as follows, e.g., in the pool exercise classes, within the 24 intensity results obtained, 18 (6 + 8 + 4) fell within the moderate intensity level, 4 (2 + 2) within the light intensity level and 2 within the vigorous intensity level. Legend: HRmax %predicted: maximum HR percentage predicted; METs – metabolic equivalent tasks.](https://static.elsevier.es/multimedia/25310437/0000003000000006/v1_202411040635/S253104372300199X/v1_202411040635/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9znTMwFdb/TnkS0koegILxs=)



