Interstitial lung diseases (ILD) encompass a heterogeneous group of lung diseases with more than 300 subtypes, with the most common being sarcoidosis, idiopathic pulmonary fibrosis (IPF), hypersensitivity pneumonitis, connective tissue disease-associated ILD, pneumoconiosis and drug-induced ILD.1 Although these subtypes present different aetiology and prognosis,1 all share common clinical features such as disabling symptoms and impaired functional capacity, which accelerate disease progression and mortality risk.2 Assessing functional capacity, a highly meaningful health-domain for the daily life of people with ILD, is therefore crucial. The 6-minute walk test (6MWT) has been the most widely used test to assess it and to predict survival in ILD,3 however its applicability across settings (e.g., patients’ homes) is limited. Alternative tests such as the 1-minute sit-to-stand test (1-minSTS)4 and the Chester step test (CST)5 have emerged. Both are simple and low-cost field tests which require minimal physical space to assess functional capacity, however, the CST also enables exercise prescription.5,6 The CST has shown to be valid and reliable in people with ILD,7 however its suitability for use as a first-line screening tool is still unknown. Thus, we explored the discriminative ability of the CST in distinguishing people with ILD with/without functional capacity impairment and low/higher chance of survival.
A cross-sectional study was conducted with ethical approval from three ethic committees [Administração Regional de Saúde do Centro (Ref. 16/2020), Centro Hospitalar do Baixo Vouga (N/ref.15-04-2019; 15-05-2019) and UICISA:E (P/N°P619-10/2019; P620-10/2019)]. Data protection followed the European regulation (EU 2016/679). Adult individuals diagnosed with ILD and clinically stable for 1 month prior the study were included. Individuals with other lung diseases and/or a clinical condition that may limit their participation in data collection were excluded. Informed consent was obtained from each participant prior to data collection.
Sociodemographic, anthropometric and clinical data (lung function, ILD subtype, comorbidities and medication) were collected with a questionnaire and medical records. Participants were classified according ILD-GAP model.8 Additionally, dyspnoea was assessed with modified British Medical Research Council–dyspnoea scale, physical activity with Brief-Physical Activity Assessment Tool and functional capacity with the CST, the 6MWT and the 1-minSTS test. The CST is a 5-stage incremental step test lasting for a maximum of 10 min, where participants step according to a timed metronome.5,7 More steps indicate better functional capacity.5,7 Further details on monitoring and criteria to interrupt the CST can be found in supplementary material 1. The 6MWT and the 1-minSTS were performed as recommended.4,9
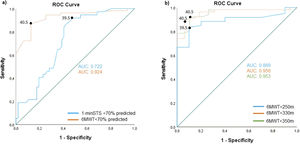
A receiver operating characteristics (ROC) curve analysis was performed. We determined the thresholds for the CST to identify: i) functional impairment, based on cut-offs of the 70% predicted of the 6MWT and the 1-minSTS;10 and, ii) higher chance of survival, based on published mortality-associated ILD cut-offs of the 6MWT (250 m, 330 m and 350 m).3,11 The optimal cut-off points were identified by the highest Youden index [the point where the sensitivity (SN) and specificity (SP) were simultaneously maximized]. The area under the curve (AUC) and the SN, SP and accuracy were also calculated. The AUC was interpreted as: <0.5-no discrimination, 0.5–0.69-poor discrimination, 0.7–0.79-acceptable discrimination, 0.8–0.89-excellent discrimination, ≥0.9-outstanding discrimination. People with ILD below or above the cut-off point of the CST or with/without comorbidities or amongst ILD subtypes were compared using independent t-test/Mann-Whitney U/chi-square tests. The impact of SpO2 levels during the performance of the CST on the prognosis was computed using a linear mixed model. The level of significance was set at 0.05.
Ninety-four people with ILD (64±13 years, DLCO=51±21% predicted) were included (Supplementary material 2 and Table 1). During the CST performance, a significant decrease in SpO2 (−3.5 ± 3.8%, p<0.001) was observed similarly between ILD severity (p>0.05) (Supplementary material 3). Number of steps in the CST was not influenced by comorbidities or ILD subtype (p>0.05) (Supplementary material 4 and 5).
Sample characterisation (n = 94) and comparison of people below (n = 40) and above (n = 54) the cut-off point (41 steps).
Values are presented as frequencies (percentages), mean±standard deviation or median [IQR].
Legend: 1-minSTS, 1-minute Sit-To-Stand test; 6MWT, 6-minute walk test; BMI, body mass index; BPAAT, Brief Physical Activity Assessment Tool; CHP, Chronic Hypersensitivity Pneumonitis; CST, Chester step test; CTD-ILD, Connective Tissue Disease-associated ILD; DLCO, Diffusing Capacity for Carbon Monoxide; FEV1, Forced Expiratory Volume in 1 second; FVC, Forced Vital Capacity; GORD, gastro-oesophageal reflux disease; ILD, Interstitial Lung Disease; ILD-GAP model, Interstitial Lung Disease-Gender, Age and Physiology model; IPF, Idiopathic Pulmonary Fibrosis; LTOT, long-term oxygen therapy; mMRC, modified Medical British Research Council; OSA, obstructive sleep apnoea.
Cut-offs of 41 and 40 steps in the CST were determined to differentiate participants with and without functional impairment using 6MWT<70% predicted and 1-minSTS<70% predicted, respectively. The 6MWT<70% predicted cut-off demonstrated better discriminative ability (AUC=0.92 [0.86–0.99]; SN=87%, SP=88%) compared to the 1-minSTS<70% predicted cut-off (AUC=0.72 [0.62–0.82]; SN=87%, SP=58%) (Fig. 1 and Supplementary material 6).
Receiver operating characteristics (ROC) curve to identify: a) functional impairment, based on the cut-offs of the 6MWT<70% predicted and 1-minSTS<70% predicted; and, b) chance of survival (cut-offs of 6MWT<250 m, <330 m and <350 m) in the Chester step test in people with interstitial lung disease. Legend: 1-minSTSpp, 1-minute sit-to-stand test, percentage predicted; 6MWT, 6-minute walk test; 6MWTpp, 6-minute walk test percentage predicted; AUC, area under the curve.
Except for the 6MWT<250 m cut-off, the other two cut-offs of the 6MWT identified a cut-off of 41 steps in the CST, to potentially reflect higher chance of survival in people with ILD. The cut-offs of the 6MWT<330 m and <350 m showed best discriminative ability, with an outstanding discrimination (AUC=0.96; 0.91–1 and AUC=0.95; 0.90–1) and higher balanced SN and SP (89%/94% and 92%/90%, respectively) compared with the cut-off of 6MWT<250 m (AUC=0.89; 0.81–0.97; SN=83%, SP=90%) (Fig. 1 and Supplementary material 6).
People below the cut-off of 41 steps in the CST were older, predominantly diagnosed with IPF, (p<0.001), at severe disease stages (according ILD-GAP model) and had worse lung function (p<0.05), dyspnoea (p<0.001) and functional capacity in all measures (CST, 1-minSTS and 6MWT; p<0.001) than those above the cut-off (Table 1).
A cut-off of 41 steps in the CST can effectively identify functional capacity impairment and chance of survival in ILD. This is the first study analysing the CST ability to detect health-related impairments. These findings have significant clinical implications, offering a meaningful and person-centred test,12 representative of daily activities (stair climbing) and which can be conducted in any setting, even in limited-spaces. Using our 41 steps cut-off, health professionals may now personalise interventions to enhance functional capacity in ILD.
FundingThis project was funded by Programa Operacional de Competitividade e Internacionalização – POCI, through Fundo Europeu de Desenvolvimento Regional - FEDER (POCI-01-0145-FEDER- 007628), by Fundação para a Ciência e a Tecnologia (PhD grant SFRH/BD/148741/2019 and COVID/BD/153477/2023) and under the project UIDB/04501/2020.