To quantify the impact of different air pollutants on respiratory health based on robust estimates based on international data and to summarise the evidence of associations between indoor exposure to those pollutants and respiratory morbidity in the Portuguese population.
ResultsSeveral systematic reviews and meta-analyses (MA) at the world level demonstrate the impact of indoor air quality on respiratory health, with indoor particulate matter and gasses exerting a significant effect on the airways. Volatile organic compounds (VOC) have been related to asthma and lung cancer. However, only meta-analyses on biomass use allowed documentation of long-term respiratory effects. While early publications concerning Portuguese-based populations mainly focused on indoor exposure to environmental tobacco smoke, later studies relocated the attention to relevant exposure environments, such as day care buildings, schools, residences and nursing homes. Looking at the pooled effects from the reviewed studies, high levels of carbon dioxide and particulate matter in Portuguese buildings were significantly associated with asthma and wheezing, with VOC and fungi showing a similar effect in some instances.
ConclusionsDespite the significant reduction of indoor air pollution effects after the 2008 indoor smoking prohibition in public buildings, studies show that several indoor air parameters are still significantly associated with respiratory health in Portugal. The country shares the worldwide necessity of standardisation of methods and contextual data to increase the reach of epidemiological studies on household air pollution, allowing a weighted evaluation of interventions and policies focused on reducing the associated respiratory morbidity.
Europeans spend a significant part of their time indoors.1 While inside a building, either at work, home, school or leisure spaces, occupants are exposed to microenvironments with particular air quality profiles that, after a short acute or long-term period of exposure, may determine exacerbation or development of, among other diseases, respiratory morbidity,2 such as irritation of lower and upper airways, acute and chronic respiratory disorders, including lung cancer, and lung function impairment.3 Mortality associated with these indoor air exposures is also relevant, as the World Health Organization (WHO) estimated in 2020 that 3.2 million deaths per year, including over 237000 deaths of children under the age of 5, were attributed to household air pollution alone.4 Most deaths occur in developing countries where around 2.4 billion people cook using open fires or inefficient stoves fueled by kerosene, biomass (wood, animal dung and crop waste) and coal, which generate harmful household air pollution.5
Indoor chemical air pollutants comprise nitrogen dioxide (NOx), carbon monoxide (CO), ozone (O3), sulfur dioxide (SO2) and volatile organic compounds (VOCs), as well as particulate matter (PM). In addition, indoor airborne microbiological agents include bacteria, viruses and endotoxins. Other indoor air quality parameters, such as temperature, relative humidity, and CO2, may also influence occupants’ susceptibility to the aforementioned air pollutants or directly impact their well-being,6,7 which is also influenced by the hosts’ characteristics.
Indoor air quality (IAQ) is a subject of particular concern to Portugal since it is one of the European countries most affected by energy poverty, a designation frequently associated with inadequate indoor air quality.8,9 Around 4% of Portuguese families are affected by severe housing deprivation conditions,10 and there seems to be a generalised absence of awareness among the population, which may lead to incorrect ventilation behaviours and excessive emission of hazardous pollutants.11 Although Portuguese legislation provides reference values regarding the indoor concentrations for most of these parameters,12 they are mainly based on WHO recommendations and are not adequately adapted to the Portuguese living conditions and occupants’ behaviours. For instance, natural ventilation is the rule in most buildings, and most of those equipped with HVAC systems cannot afford to use them.8 This situation strongly contrasts with other European countries with different climates, socioeconomic environments and physiognomic characteristics of their occupants.13
Hence, it is essential to understand how indoor air pollutants are associated with the respiratory health of populations to optimise legal regulations and national healthcare. This manuscript thus aims to: 1) quantify the impact of different air pollutants on respiratory health based on robust estimations; 2) summarise and disseminate studies concerning the Portuguese population, focused on the association between indoor air quality and respiratory health.
This article is the fourth in the Series on “Air pollution and health”14-16 and is closely linked to the companion paper on indoor pollution.17
MethodologyThe manuscript is structured into a general update and the Portuguese perspective: the former provides recent (from 2018 to 2022) quantitative estimates of the health impact due to indoor air quality at a global level based on robust data; the latter comprises a qualitative and quantitative summary of the findings obtained in international publications concerning the effects of IAQ on the respiratory health of the Portuguese population.
General updateThe general update on the health impact of indoor air quality in terms of chemical exposures at the world level was based on a PubMed Search using the words “indoor air” or “IAQ” and “respiratory” or “asthma*” or “COPD” or “pulmon*” not “outdoor/traffic” or “COVID-19” for the period 2018-2022. This yielded 755 papers. Limiting the search to reviews and meta-analyses produced 89 results, seven of which were meta-analyses (MA), providing robust estimations of effects.18-24 The results from these MA were retained for presentation in this paper.
The Portuguese perspectiveThe Portuguese perspective section was based on an online literature search in PubMed for studies published up to the 5th of August 2022 using the search terms “indoor air” or “IAQ” and “respiratory” or “asthma*” or “COPD” or “pulmon*” and “Portugal” or “Portuguese”.
A total of 77 articles were returned, one being excluded as a duplicate, eight for only being methodological or proceedings articles with no data output, two for being focused on COVID-19, three for not including any IAQ parameter, 27 for not measuring a respiratory outcome, 14 for not including a Portuguese population, two for considering only occupational exposures and two narrative reviews. One extra article meeting the inclusion criteria was identified through cross-referencing. Hence, 19 articles were thoroughly reviewed and summarised to express the Portuguese perspective.25-43
For the quantitative analysis, 13 of the 19 reviewed articles that reported the effect estimates for exposure to indoor air pollutants on the development or exacerbation of respiratory diseases were included. Based on the available data for respiratory outcomes, pooled estimates were calculated for asthma, wheezing and a combination of asthma symptoms, wheezing and asthma. Since the same population was used for multiple conditions (for instance, by having studied the association of numerous indoor air parameters with the same respiratory outcome), random-effect models were selected. Analysis of metadata was performed using the R “meta” and “metagen” packages to estimate pooled odds ratio and respective 95% confidence interval (OR and 95%-CI).44 Forest plots were constructed to illustrate the results.
ResultsGeneral updateFive systematic literature reviews and meta-analyses (MA) that fulfilled the selection criteria of robustness allowed us to re-examine existing research data about the association between indoor air pollutants and respiratory health. These varied according to the type of respiratory disease and air pollutant. The total number of included studies and respiratory patients in these MA is relevant. Furthermore, two systematic reviews reported on modifiers of air quality.
Robust and reliable effects (per 10 μg/m3) from a systematic review and MA including 101 studies were observed for SO2 with chronic obstructive pulmonary diseases (COPD) (pooled relative risks [RRs] 1.016, (95% confidence interval [CI] 1.012-1.021] and for NO2 with childhood asthma, preterm birth (a risk factor for asthma), lung cancer, and COPD (RRs 1.134 [1.084-1.186], 1.079 [1.007-1.157], 1.055 [1.010-1.101] and 1.016 [1.012-1.120], respectively).19 No robust effects of O3 and CO were observed for any of these respiratory diseases.
The MA of 35 studies with 73,122 participants indicated that exposure to indoor air pollution due to biomass smoke was strongly associated with COPD.22 Exposure to indoor air pollution due to solid biomass fuels significantly increased the risk of COPD (odds ratio [OR] 2.65 [CI 2.13-3.31]) and chronic bronchitis (2.89 [2.18-3.82]), compared with non-biomass fuels. The risk of COPD was higher in the African region (OR 3.19), compared with other areas (Asia (OR 2.88), South America (OR 2.15), Europe (OR 2.30) and North America (OR 2.14)).
Still, in the context of COPD, the summary estimates from 24 studies showed that biomass smoke exposure was associated with COPD in rural and urban women.20 There was more risk of COPD prevalence through clinical diagnosis than spirometry alone. Biomass-exposed individuals were 1.38 times more likely to be diagnosed with COPD than non-exposed (OR 1.38 [CI 1.28, 1.57]). Spirometry-diagnosed COPD studies failed to show a significant association (1.20 [ 0.99, 1.40]). Furthermore, the summary estimate of OR for chronic bronchitis (CB) was also significant (2.11 [1.70 to 2.52]).
Another recent systematic review and MA21 of 32 studies provided robust evidence for associations between VOCs and asthma as indicated by pooled RRs for asthma of 1.08 [CI 1.02-1.14], 1.02 [1.00-1.04], and 1.04 [1.02-1.06] per 1 μg/m3 increase of benzene, toluene, and p-dichlorobenzene, respectively. The pooled RR for low birth weight was 1.12 [1.05-1.19] per 1 μg/m3 increase of benzene.
Similarly, 13 papers included in a meta-analysis allowed us to calculate the pooled OR between formaldehyde (FA) exposure and asthma. Each 10 µg/m3 increase in FA exposure was significantly associated with a 10% increase in the risk of asthma in children (OR = 1.10 [CI 1.00-1.21]. FA exposure was also associated with an increased risk of asthma (1.81 [1.18-2.78]) in adults, when separating the high-exposure adult group (FA > 22.5 µg/m3) from the rest of the population.
Additional data collected in systematic reviews also exist on the description of the modifiers of air quality. Forty-nine studies described indoor PM2.5 concentrations generated from various familiar household sources in real-life home settings in high-income countries (HICs). These included wood/solid fuel burning appliances, cooking, candles, incense, cleaning and humidifiers. The reported concentrations varied widely between sources and within groups of the same source. The burning of solid fuels was found to generate the highest indoor PM2.5 concentrations. On occasion, other sources were also reported to be responsible for high PM2.5 concentrations; however, this was only in a few select examples. This review also highlights the many inconsistencies in how data are collected and reported.23
A recent review describing the parameters that affect IAQ in residential dwellings is also of great interest, such as building location, layout, ventilation, finishing materials, occupant activities, and occupant demography.18 From 180 peer-reviewed articles, published from 01/2013 to 09/2021, it resulted that, when considering classical pollutants such as particulate matter (PM) or volatile organic compounds (VOCs), the building parameters can have a significant impact on IAQ and detailed information of these parameters needs to be reported in each study.
The Portuguese perspectiveA total of 19 publications studying the associations between IAQ and respiratory diseases in Portugal were included and reviewed. The review has been structured first to describe studies on environmental tobacco smoke (ETS), a source of indoor air pollution that has been losing relevance since the implementation of smoke-free laws, followed by a summary of studies assessing IAQ sectioned by the different building settings that characterise lifetime indoor exposure.
Of the 19 publications, four were focused on indoor exposure to ETS,27-30 two studied day care settings,25,26 eight assessed the indoor environments in schools,36-43 three were concentrated on residential buildings,31-33 while the remaining two articles were based on nursing homes.34,35
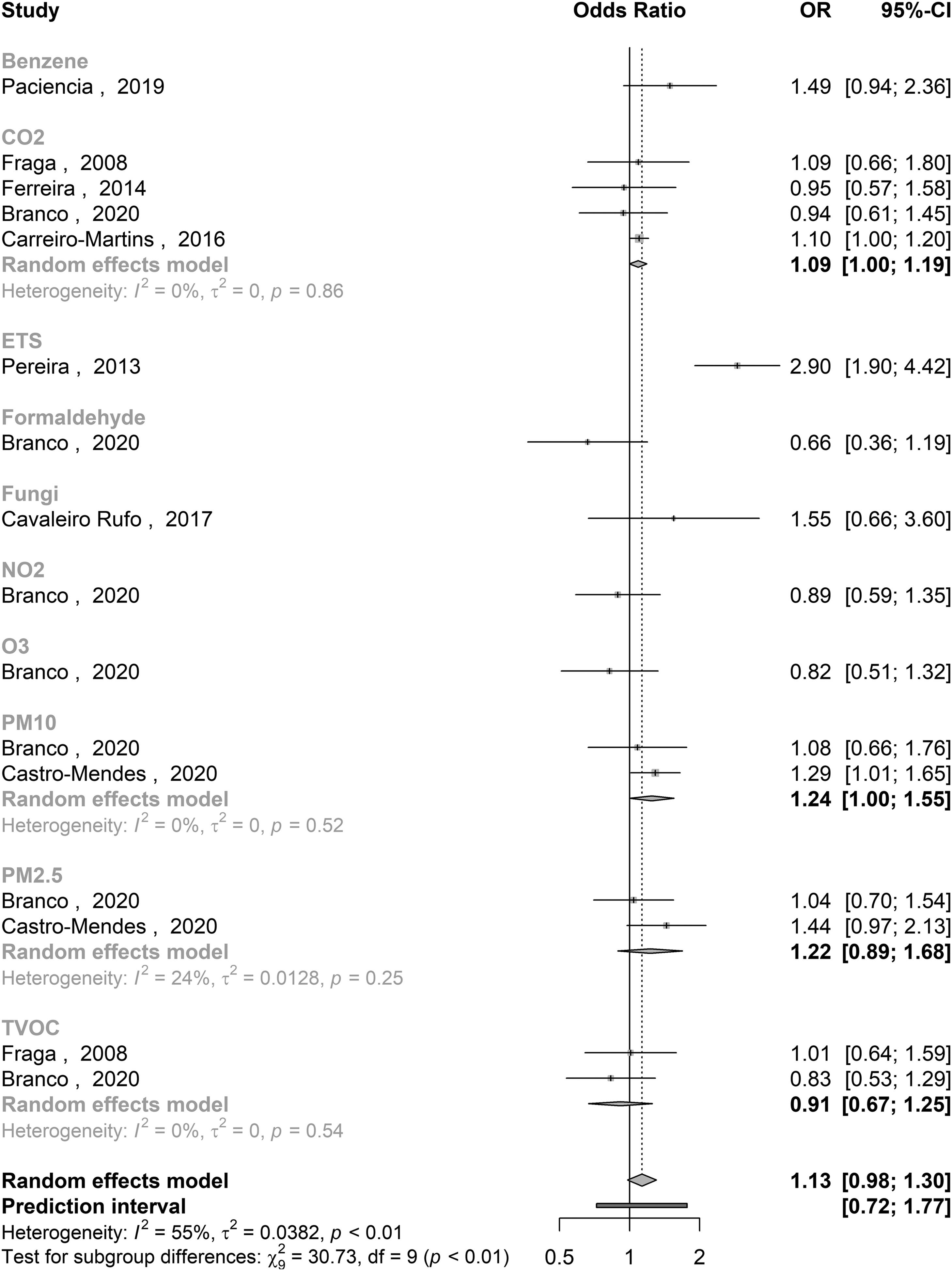
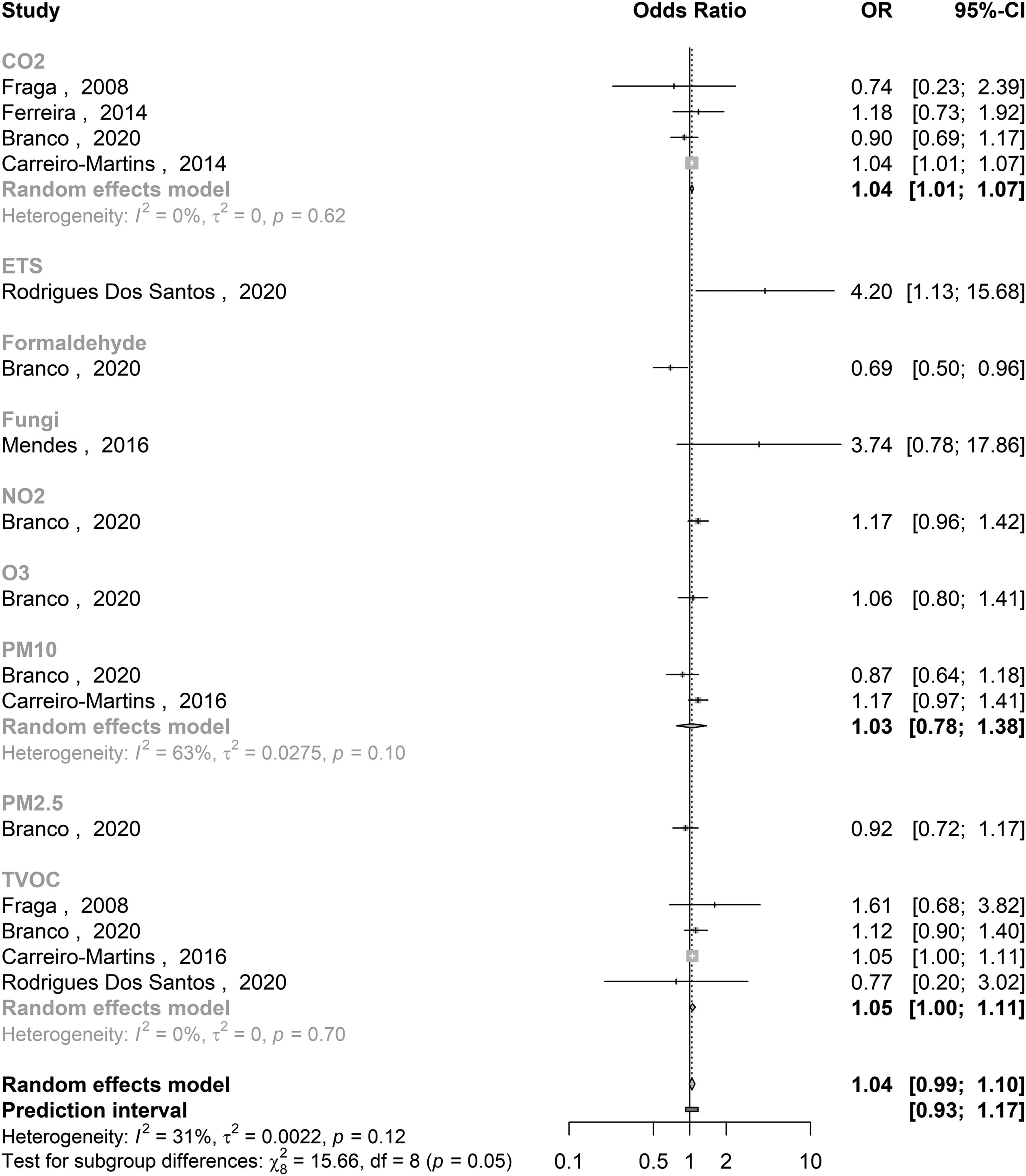
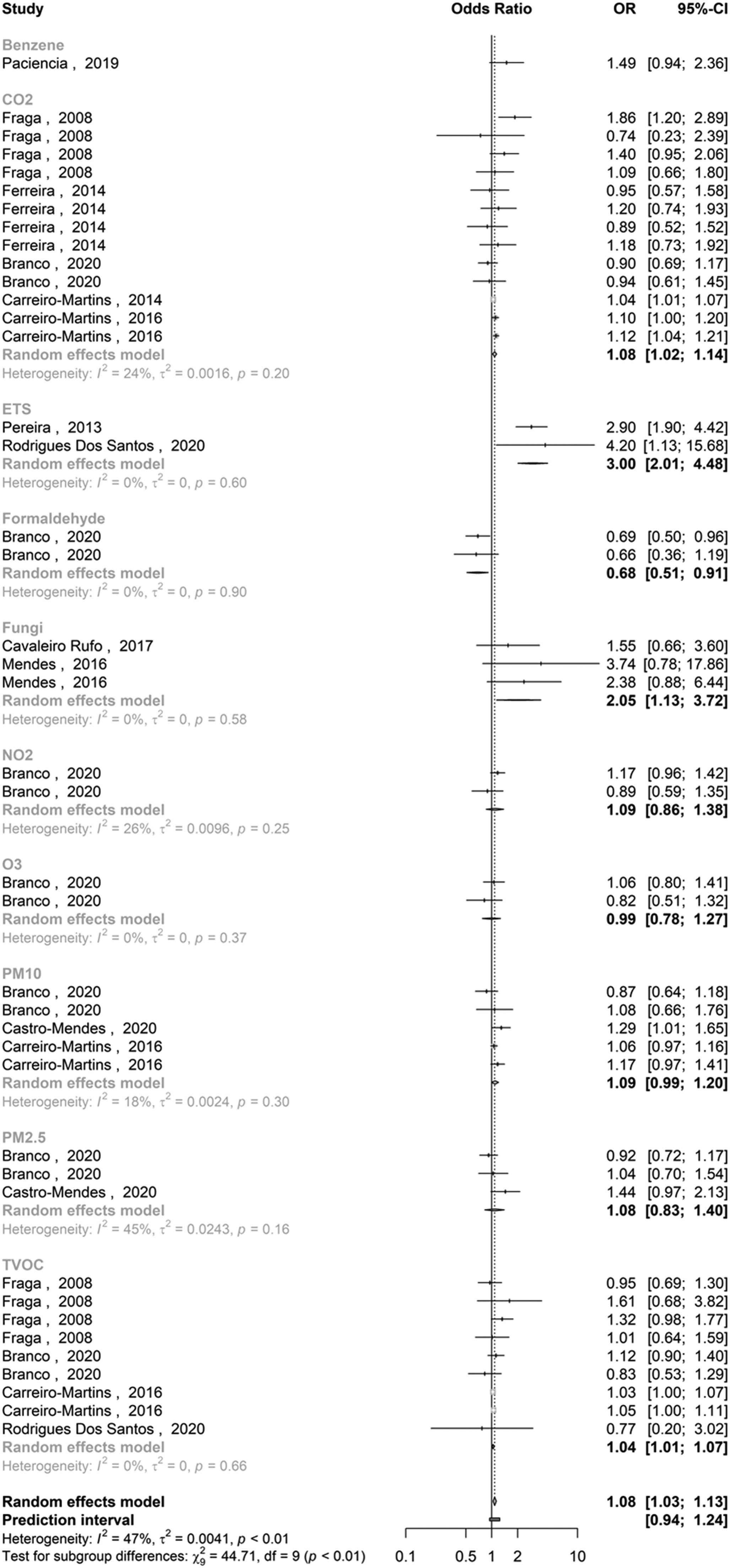
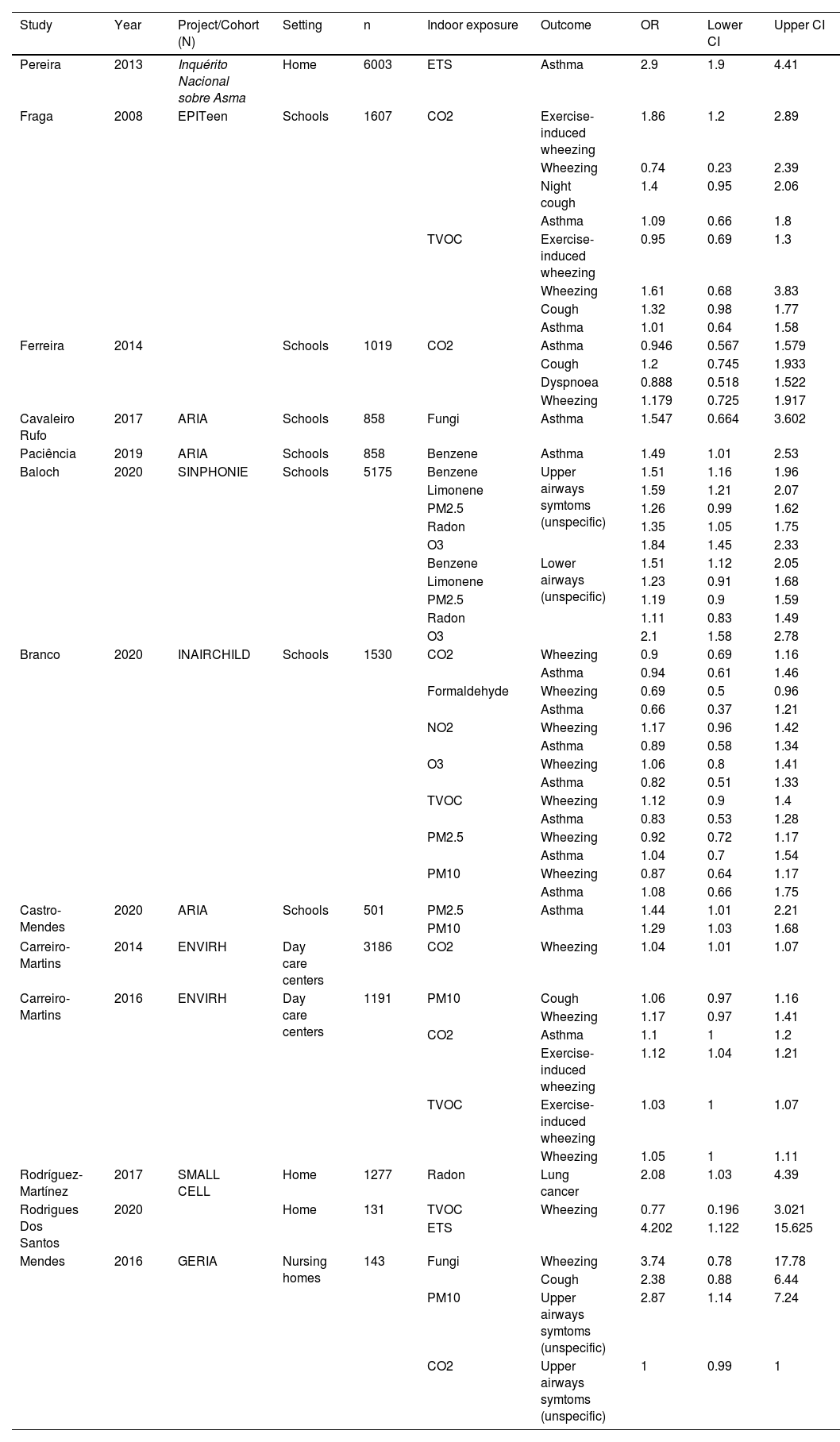
Quantitative analysisA total of 14 of the 19 publications met the criteria for meta-analysis (Table 1). With the available data, pooled effects were possible to estimate for asthma (Fig. 1) and wheezing outcomes (Fig. 2), as well as a combination of asthma and asthma-related symptoms, including wheezing and exercise-induced wheezing, cough and night cough, and dyspnoea (Fig. 3). Heterogeneity between studies seems moderate for all measured outcomes when accounting for the different parameter subsets, with the association between PM10 and wheezing being the only subgroup resulting in an I2 > 50%.
Summary of effect estimates retrieved from the reviewed studies. All outcomes (and corresponding studies) where the pooling of effect estimates was possible were included in the meta-analysis.
The pooled estimate (and 95% CI) for the effect of indoor air quality on asthma was 1.13 [0.98 : 1.30], with significant associations found for CO2 (1.09 [1.00 to 1.19], based on 4 studies), ETS (2.90 [1.90 to 4.42], single study) and PM10 (1.24 [1.00 to 1.55], 2 studies). Regarding wheezing, the pooled effect estimate was 1.04 [0.99 to 1.10), with significant associations found for CO2 (1.04 [1.01 to 1.07], 4 studies), ETS (4.20 [1.13 to 15.68], single study), formaldehyde (0.69 [0.50 to 0.96], single study) and TVOC (1.05 [1.00 to 1.11], 4 studies). Finally, the pooled effect estimates showed a significant association between IAQ parameters and asthma or asthma-related symptoms (1.08 [1.03 to 1.13]), with significant contributions from CO2 (1.08 [1.02 to 1.14], 13 inputs from 4 studies), ETS (3.00 [2.01 to 4.48], 2 studies), fungi (2.05 [1.13 to 3.72], 3 inputs from 2 studies) and TVOC (1.04 [1.01 to 1.07], 9 inputs from 4 studies). On the other hand, the only study performed in Portugal that explored the associations between indoor formaldehyde concentrations and respiratory health surprisingly reported a significant protective effect (0.68 [0.51 to 0.91], 2 inputs from a single study).
Environmental tobacco smokeFour reviewed studies focused on ETS, which is recognised as one of, if not the primary source of IAQ pollutants with highly documented evidence of causing respiratory morbidity. This has been reinforced by one of the reviewed studies showing that female individuals with asthma were more likely to be exposed to ETS when compared with those without the disease (OR [95% CI] = 2.90 [1.90 to 4.41]).30 It used data collected in 2010 from the Inquérito Nacional sobre Asma (The Portuguese National Asthma Survey), a cross-sectional study conducted through telephone interviews based on the GA2LEN questionnaire,45 targeting a randomised sample of individuals living in Portugal.46
Interestingly, a different study found converse results when focusing exclusively on children, showing no significant differences in secondhand exposure to ETS in indoor environments between asthmatic and non-asthmatic children.27 This survey also started in 2010 and was conducted by administering a self-reported questionnaire to 4th grade students attending schools in nine regions of Portugal.
The two remaining studies were centred on the effects of the smoke-free law that prohibited smoking indoors in public settings. The first was published in 2009 and refers to the Spanish smoke-free law, implemented in 2006, roughly two years before the law being applied in Portugal.28 It consisted of a longitudinal study that followed Spanish hospitality workers for 12 months after implementation of the regulation mentioned above. However, the article still provides a relevant perspective since it used Portuguese workers as controls in a timeframe when the law was still to be implemented in the country. Results demonstrated that, 12 months after smoking was banned, hospitality workers in Spain showed a significant decrease in the prevalence of respiratory symptoms. Although the prevalence also decreased in Portuguese workers, results were not statistically significant.28
In 2013, a study monitored IAQ in 10 Portuguese restaurants pre- and post-smoke ban (2 years since law implementation), as well as changes in respiratory symptoms and comfort parameters reported by 28 individuals working in those restaurants.29 Results showed that banning indoor smoke in these restaurants significantly reduced PM concentrations, total VOC (TVOC), benzene and CO. In addition, workers experienced fewer irritative symptoms after the ban, but there was no significant change in dyspnea.
Day care centresForty five day care centres from Lisbon and Porto, the two largest cities in Portugal, were included in a study aiming to evaluate the associations between indoor CO2 concentrations and symptomatology in preschool children.26 Results showed that CO2 was significantly associated with a higher prevalence of wheezing in children (1.04 [1.01 to 1.07]). Authors could also inversely correlate indoor CO2 in daycare centres with good ventilation practices, such as opening the windows.26 This result emphasises the need for instructing school and day care staff on ventilation behaviours to maintain adequate IAQ.
In a second phase of the same study, part of the ENVIRH project, the research group performed a thorough IAQ in 19 of the 45 day care centres with the worst ventilation practices.25 Authors found CO2 to be significantly associated with a diagnosis of asthma (1.10 [1.00 to 1.20]), while TVOC and concentrations of Der p1 in dust were associated with wheezing in the previous 12 months (1.06 [1.01 to 1.11] and 1.06 [0.99 to 1.12], respectively).
SchoolsThe first study to measure the associations between IAQ and respiratory health in adolescents in Portugal was published in 2008 and was part of the EPITeen project.41 Capitalizing on the previously validated Portuguese version of the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire, and after measuring temperature, relative humidity, CO2 and TVOC in 9 middle schools (7th, 8th and 9th grade, mean age 14.0) in the city of Porto, authors found significant associations between high levels of CO2 in classrooms and exercise-induced wheeze (1.86 [1.20 to 2.89]), hence corroborating the previously mentioned results of the ENVIRH project, in younger children.26 On the other hand, there were no significant associations between TVOC and respiratory symptoms.41
In another study, CO2 levels were assessed in 81 classrooms in 51 primary schools in Coimbra.40 Again, CO2 was above the reference level (1625 ppm for naturally ventilated buildings, according to Portuguese law) in most classrooms during Autumn and Winter, and was significantly correlated with lack of concentration (p = 0.002). No associations between respiratory health and CO2 were reported.
The first studies reporting the clinical outcomes of the Portuguese ARIA project were progressively published in 2017.38,42,43 The project aimed to study the associations between IAQ at schools in Porto and the development of allergic diseases and asthma in children. The project was distinguished for merging a complete evaluation of indoor air parameters in 71 classrooms from 20 primary schools with a comprehensive clinical evaluation of 858 children attending those classrooms, including skin-prick tests, spirometry with bronchodilation, exhaled nitric oxide (eNO), pupillometry, exhaled breath condensate (EBC) collection and anthropometric measurements. The children's legal guardians were also asked to fill out an ISAAC-based self-reported questionnaire. By analysing data from the ARIA project, significant associations were identified between high fungal diversity in classrooms and a lower risk of allergic sensitisation in children (0.60 [0.40 to 0.92]).38 However, no associations between microbial diversity and asthma were found.
Specific VOC were also measured in the ARIA project, with researchers being able to significantly associate a pattern of VOC – characterised mainly by high levels of toluene, o-xylene, m/p-xylene, benzene, ethylbenzene and styrene – with respiratory symptoms and asthma in children, particularly those with the obese asthma phenotype (1.43 [1.01 to 1.98]).42,47
Another publication on the same study population showed that children exposed to higher concentrations of particulate matter (both PM2.5 and PM10) were at a significantly higher risk of developing asthma, but this association was mediated by dietary practices (interaction effect = 1.44 [1.01 to 2.21] and 1.29 [1.03 to 1.68], for PM2.5 and PM10, respectively).39 In other words, children with a pro-inflammatory diet – according to the dietary inflammatory index – were less protected from the effects of PM2.5 and PM10 as asthma determinants, when compared with those under an anti-inflammatory diet.
Temperature, relative humidity and PM2.5 were also associated with a decrease in EBC pH; another team study showed.43 As a more acidic EBC has been associated with asthma.,48 these IAQ parameters may eventually contribute to a particular mechanism in its pathophysiology.
In 2020, the most recent study comprising data from the European project SINPONIE was published.36 This project aimed to assess the IAQ and built environment in 115 European schools, including Portuguese institutions, and study possible associations with symptomatology in 7089 attending children.49 After dichotomizing the concentrations of pollutants by their median, results showed that classrooms with higher concentrations of PM2.5, benzene, limonene, ozone and radon in classrooms were associated with increased odds for upper and lower airways symptoms. A significantly higher risk of lower and upper airways symptoms was also observed for the classrooms within the highest tier of VOC concentrations.
The final study in this section is part of the INAIRCHILD project,50 which followed a similar strategy as the ARIA project, but also included pre-scholar infants (3 to 5 years old). Results showed that inhalable doses of NO2 were significantly and positively associated with current wheezing (1.27 [1.02 to 1.59]), and PM2.5 and O3 exposure was associated with reduced FEV1 in primary school children (1.90 [1.11 to 3.25] and 2.38 [1.23, 4.63], respectively), but there was no identifiable relationship between inhalable doses of any indoor air pollutant and asthma.37
The residential environmentA 2020 study evaluated associations between IAQ and wheezing in 131 families with newborns (0 to 36 months) from the Arco Ribeirinho region, south of Lisbon, across the Tejo river.31 Building characterisation was conducted, and the children's bedrooms were monitored for TVOC. Results showed no associations between indoor TVOC and wheezing in children (0.77 [0.20 to 3.02]). Unfortunately, no specific volatiles were measured during this study.
The only other identified study focusing on residential IAQ was part of the SMALL CELL project, which included one Portuguese hospital (Centro Hospitalar do Porto).33 Patients with small cell lung cancer were recruited, and 63 had their residences monitored for radon concentration. Authors found that radon concentrations in stage IV patients were significantly higher in individuals diagnosed at later ages (p = 0.032), suggestive of the long-term effect of radon exposure demonstrated in previous studies.51 These results were complemented in a later publication from the same group, where authors showed that individuals with concentrations higher than 147 bq/m3 were at a significantly higher risk of developing small cell lung cancer (2.08 [1.03 to 4.39]).32
Nursing homesIn old-age, people are also highly susceptible to indoor air pollutants.52 A significant part of this population spends approximately 90% of their time in nursing homes, which reflects a pronounced opportunity for long-term exposure to indoor air pollutants. This is particularly important to the Portuguese perspective, since 19% of the population is aged over 65 years old. 53,54
A study which evaluated the influence of IAQ on the respiratory health of 668 residents from 21 long-term nursing homes showed PM10 to be significantly associated with allergic rhinitis (2.87 [1.14 to 7.24]) reported through questionnaire interview.35 However, no significant associations were observed for asthma-related symptoms, such as wheezing or coughing.
A later study with a similar objective was conducted in 33 nursing homes from Lisbon and 20 from Porto.34 In this study, a clinical evaluation of the participants was performed, including lung function measurement, EBC analysis and nitrite level quantification. Results showed that each 100 mg/m3 increment of TVOC was associated with a 5% average increase in the odds of respiratory infection in the previous three months (1.05 [1.00 to 1.09]). It was also shown that PM2.5 concentrations were inversely associated with EBC pH values (β [95% CI] = -0.04 [-0.06 to -0.01]), thus supporting the observations in the previously discussed study by Rama et al.43 In addition, total bacteria concentrations were significantly associated with an increase in FEV1/FVC (β [95% CI] = 0.22 [0.08 to 0.37]) and a decrease in FVC (β [95% CI] = -0.53 [-0.87 to -0.20]), when adjusted to respiratory disease.34 Nevertheless, it is necessary to states that each pollutant was fitted into models adjusted for different confounders or in combination with other covariates, with only significant effect estimates being shown in completely separated models. For this reason, caution is advised when interpreting these results.
DiscussionGeneral updateEvidence is increasing on the impact of indoor air quality on respiratory health at a world level based on systematic reviews and meta-analyses (MA), including several respiratory patients, which confirm previous data. They demonstrate that indoor particulate matter and gases significantly affect the respiratory system. VOCs have been related to asthma and lung cancer. However, most existing data are based on ad hoc assessments and thus relate to short-term effects. Only meta-analyses on biomass use have data that allow documenting the existence of long-term respiratory effects overall in women. Meta-analyses also indicate that indoor air pollution is not only a problem in developing countries.
Research gaps and suggestions for future studies together with the recommendation of where measurements should be done, are also provided. Studies show that the variable methods of measurement and reporting make comparison and interpretation of data difficult. There is a need for standardisation of methods and agreed contextual data to make household air pollutants data more useful in epidemiological studies and aid comparison of the impact of different interventions and policies.
The Portuguese perspectiveAs depicted in the reviewed studies, the Portuguese perspective concerning the association between indoor air quality and respiratory health is in line with the previous observations. Besides the link between radon and lung cancer, asthma or asthma-associated symptoms were the respiratory manifestations most commonly associated with indoor air parameters in the Portuguese population, with indoor tobacco smoking as the main offender, followed by fungi, CO2 and VOC. The main exception was formaldehyde, a compound highly associated with asthma according to the general perspective, but showing a protective effect in the single Portuguese study that assessed the effect of this pollutant on respiratory health.
The aforementioned ETS studies have demonstrated the impact of indoor smoking, and results showed how the smoke-free law for public buildings was associated with improving respiratory symptoms.28,29 Interestingly, most articles identified through the systematic search focused on studying the associations between respiratory health and the IAQ in settings where smoking was already not permitted even before the smoke-free law: daycare centres, schools and nursing homes. The first is of relevant importance as epidemiologists believe that the most determinant window of exposure to air pollutants occurs in the perinatal period.55 Therefore, indoor air quality in daycare centres and nurseries for infants should be of particular concern. Of the 19 reviewed studies, only two publications from the ENVIRH project contained data from the earliest exposure in a public setting.25,26 Later studies looked into air quality in schools, targeting older children who, although not as susceptible, spend a larger period of their life in those buildings.
For instance, the results from the SINPHONIE project support the previously existing evidence of respiratory symptomatology determined by toxic volatiles and fine particles at school.36 However, that particular study showed concerning evidence that radon exposure may be associated with upper airway symptoms in children. Radon is widely known to cause lung cancer upon long-term exposure; it is the first cause of incidence worldwide after tobacco smoke.56 In any case, little information existed regarding associations between upper airway symptoms and radon before this study. The fact that the median radon in the SINPHONIE schools was 113.8 bq/m3, considerably lower than the 300 bq/m3 used as a safety limit in most European countries, may suggest a fundamental need for further research on the health effects of radon.36 This would be particularly relevant in Portugal, as most of the country's topography involves granitic areas.57
The remaining reviewed studies, such as those resulting from the ARIA and INAIRCHILD projects, indicate that school environments may play a determinant role in modelling children's health.37-39,42,43 Children and infants spend a significant part of their time in these settings, which highlights the need for more consistent monitoring of IAQ at schools. However, the home environment is even more critical when considering the longest time of exposure to indoor air parameters, as not only children, but also adults spend a significant amount of their time at home. Unfortunately, due to the economic constraints associated with field work, the number of published Portuguese studies on residential IAQ is relatively small. Building characterisation and local climate are almost unique to each country, complicating the extrapolation of international studies results and justifying the need for more studies to uncover the national perspective on IAQ status in residential buildings.
Finally, this review covered studies examining the associations between respiratory health and IAQ in nursing homes. In most cases, these buildings are frequently the last environment that humans will be exposed to during their life course. The other final location of relevant indoor exposure is hospitals. According to a recently published systematic review looking at IAQ in healthcare units,58 this is a significant concern for occupant exposure, with hospitals frequently determining the respiratory health of elderly and younger occupants. However, as supported by the previous review, and despite some multi-approach protocols having been disclosed,59 no studies in Portugal focused on that perspective.
ConclusionsWorldwide, indoor air pollution affects respiratory health in all age groups, and several studies show such a link. Since the vast majority of the population spends more than 80% of their time indoors, air quality significantly impacts each individual's overall exposure to air pollution. In Portugal, although it has possible to substantially reduce the effects of indoor air pollution by prohibiting indoor smoking in public buildings in 2008, studies show that there are still several indoor air parameters significantly associated with respiratory morbidity in the country, including fungi, CO2 and VOC concentrations.
Globally, there is a need for standardisation of methods and agreed contextual data to make household air pollutants data more useful in epidemiological studies and aid comparison of the impact of different interventions and policies.