To compare secondhand smoke exposure (SHSe) prevalence at home and inside the car between asthmatic and non-asthmatic Portuguese children.
Materials and methodsThis is a cross-sectional study that assessed children's SHSe in a representative sample of nine Portuguese cities. A validated self-reported questionnaire was administered to a random sample of 4th grade students during the school year of 2010/2011. The asthma prevalence was defined by the answers to three questions regarding asthma symptoms, medication and inhaler use. We performed chi-square tests and analysed frequencies, contingency tables, confidence intervals, and odd-ratios.
ResultsThe self-reported questionnaire was administered to 3187 students. Asthma prevalence was 14.8% (472 students). Results showed that 32.3% of non-asthmatic children and 32.4% of asthmatic children were exposed to secondhand smoke as at least one of their household members smoked at home. The prevalence of parental smoking, smoking among fathers and smoking among mothers at home was also similar in both groups (asthmatic and non-asthmatic children). SHSe inside the car was 18.6% among non-asthmatic children and 17.9% among asthmatic children.
ConclusionsAsthmatic and non-asthmatic children were equally exposed to secondhand smoke, because no significant differences were found between the two groups concerning the prevalence of SHSe at home and inside the car. These findings highlight the need to include SHSe brief advice in paediatric asthma management.
Worldwide, children's SHSe is a serious public health problem.1 Children living with smokers are more likely to become smokers themselves. Thus, reducing children exposure to secondhand smoke (SHS) must become a public health priority.1–3 Asthma is the most frequent chronic disease in childhood and its prevalence and morbidity has been increasing in most countries.4,5 Asthma diagnosis in younger children may be difficult, but at school age a more stable phenotype of asthma has already been developed.6 Since suggestive asthma symptoms in children are not asthma-specific, the use of anti-asthmatic therapy can be a complementary diagnostic criteria.7 SHSe is a common and avoidable risk factor for wheezing and asthma in children, increasing the incidence of these problems by at least 20%.8 SHSe is associated with asthma exacerbations and poor asthma control in children.7,9,10 Many children often do not have the personal power to complain or to protect themselves.11 Children are more frequently exposed at home and in the car, as a result of parents’ smoking behaviour or other household smoker.8 Parental smoking, and particularly maternal smoking, significantly increases the risk of asthma, especially in school-aged children. These behaviours worsen the severity of asthma symptoms and may impair lung growth and lung function.8–10 Preventing parental smoking and promoting smoke-free homes is crucial for asthma prevention and control.8,9 In the United States of America (USA), 39% of families reported at least one smoker at home.12 Prior studies have shown that the prevalence of smoking bans among asthmatic children living with a smoker was less than 50%.13 SHSe inside vehicles is relatively common, and particularly harmful due to its higher concentrations of smoke when compared to SHSe at home.13 Until now few studies have addressed asthmatic-children SHSe at home or inside the car.
The aim of this study was to estimate and compare SHSe prevalence at home and in the car among asthmatic and non-asthmatic Portuguese children.
Materials and methodsStudy designA cross-sectional study, based on a self-reported questionnaire, was administered to 4th grade students during the school year of 2010/2011. The schools included in this study were randomly selected from a list provided by the Office of Statistics and the Planning Department of the Portuguese Ministry of Education.
The study was approved by the Directorate of Innovation and Curriculum of the Ministry of Education and by the directors of the selected schools.
The questionnaire had been previously administered to a small pilot group of 4th grade students. We taught the teachers how to administer the questionnaire in the classroom. Nevertheless, most of the questionnaires were administered by our full-time researchers. Before the administration of the questionnaire, every participant was asked to deliver an informed consent form signed by their parents.
Population and sampleThe population consisted of 11,659 students from the 4th grade in the school year of 2010/2011. The theoretical sample size consisted of 4112 students assuming an expected SHSe prevalence of 35% with a 95% confidence interval (CI) and a precision of 1.5%. Before the implementation of smoking bans in Portuguese public places, a previous study in the Portuguese population (Braga) showed SHSe prevalence rates of 38%.14
We included randomly-selected 4th grade students from schools in Braga, Oporto and Viana do Castelo (North littoral of Portugal); Covilhã (Centre inland), Évora (South inland), Faro and Lisbon (South littoral), and the islands of Madeira (Funchal) and Azores (Angra do Heroísmo). We achieved a response rate of 77.5% (70↔90%) with a drop-out of 925 students. The reasons for the drop-out were: (1) parents did not sign the consent form; (2) students forgot to bring the signed consent form to school; (3) students missed school when the questionnaire was administered. Thus, the sample was representative of school-aged children from the 4th grade of nine Portuguese counties during the school year of 2010/2011 and included 3187 students.
InstrumentWe administered a self-report anonymous questionnaire, which has been developed and validated for this study. It was based on survey tools used in previous studies to evaluate second-hand smoke exposure (e.g. Precioso et al., 2010. Rev Port Pneumol. 2010;16:57–72)15 and a questionnaire developed for the “Child Exposure to Environmental Tobacco Smoke (CHETS) Scottish study”.16 Content validity was assessed through specialist revision and a pilot administration among a group of 4th grade children. The questionnaire was reviewed according to their feedback, and changes in the number and in the structure of questions were made. The final version of the questionnaire consists of 34 multiple choice questions and four open-ended questions to measure the following variables: (1) sociodemographic variables: age, sex, fathers’ and mothers’ education level and occupation; (2) parental/other relatives’ smoking [Does your father/mother/brother(s)/other(s) family member(s) smoke? Answer: no, sometimes, yes]; (3) Children's SHS exposure in the family car [Does your father/mother/brother(s)/other(s) smoke in the family car? Answer: always, sometimes and never]; (3) Children's exposure to SHS at home: Smoker family members (“does not smoke”, “yes, sometimes”, “yes, every day” or “I don’t know/I do not have any”), Family members and visitors’ permission to smoke at home (“does not smoke”, “yes, every day”, “1 yes, sometimes” and “does not smoke at home” or “I don’t know/I do not have any/does not live in my house”) and rules concerning smoking inside the house (“smoking is not allowed in any part of the house”; “smoking is allowed in some parts/rooms of the house”; “smoking is allowed in any parts/rooms of the house” and “smoking is allowed only on special occasions”). For asthma diagnosis, three eligibility conditions were considered: self-reported “doctor-diagnosis” of asthma, use of a specific asthma inhaler, and use of asthma medication.
Statistical analysisData were analysed using the Statistical Package for the Social Sciences (SPSS), 19.0 version for Windows. The variable education was dichotomized using a cut-off of 9 schooling years.
For statistical analysis, we performed Chi-square tests and analysed frequencies, contingency tables, confidence intervals, and odd-ratios. Two-sided tests of significance were based on the 0.05 level.
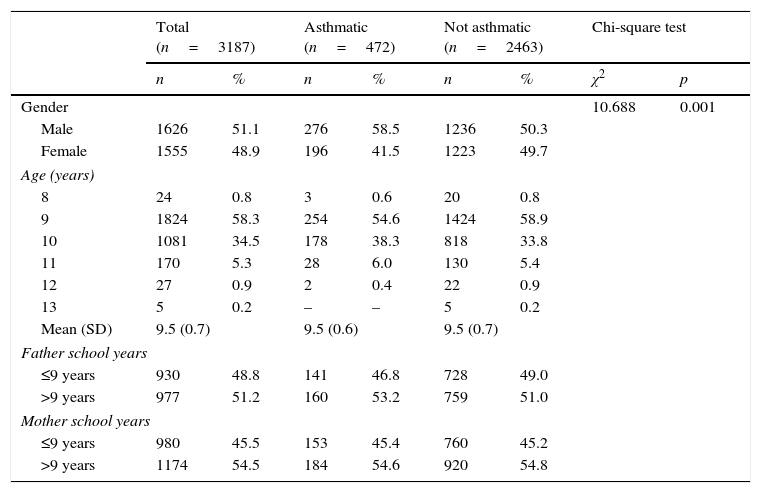
ResultsOut of the 3187 participants, 51.1% were male and the mean age for all the sample was 9.5±0.7 years, as shown in Table 1. The proportion of male children with asthma was significantly higher than the proportion of female children (p<.001). The prevalence of parental smoking was 52%; smoking prevalence among fathers was 43.7%; and smoking prevalence among mothers was 29.3%.
Descriptive statistics of children and parents socio-demographic characteristics.
| Total (n=3187) | Asthmatic (n=472) | Not asthmatic (n=2463) | Chi-square test | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | χ2 | p | |
| Gender | 10.688 | 0.001 | ||||||
| Male | 1626 | 51.1 | 276 | 58.5 | 1236 | 50.3 | ||
| Female | 1555 | 48.9 | 196 | 41.5 | 1223 | 49.7 | ||
| Age (years) | ||||||||
| 8 | 24 | 0.8 | 3 | 0.6 | 20 | 0.8 | ||
| 9 | 1824 | 58.3 | 254 | 54.6 | 1424 | 58.9 | ||
| 10 | 1081 | 34.5 | 178 | 38.3 | 818 | 33.8 | ||
| 11 | 170 | 5.3 | 28 | 6.0 | 130 | 5.4 | ||
| 12 | 27 | 0.9 | 2 | 0.4 | 22 | 0.9 | ||
| 13 | 5 | 0.2 | – | – | 5 | 0.2 | ||
| Mean (SD) | 9.5 (0.7) | 9.5 (0.6) | 9.5 (0.7) | |||||
| Father school years | ||||||||
| ≤9 years | 930 | 48.8 | 141 | 46.8 | 728 | 49.0 | ||
| >9 years | 977 | 51.2 | 160 | 53.2 | 759 | 51.0 | ||
| Mother school years | ||||||||
| ≤9 years | 980 | 45.5 | 153 | 45.4 | 760 | 45.2 | ||
| >9 years | 1174 | 54.5 | 184 | 54.6 | 920 | 54.8 | ||
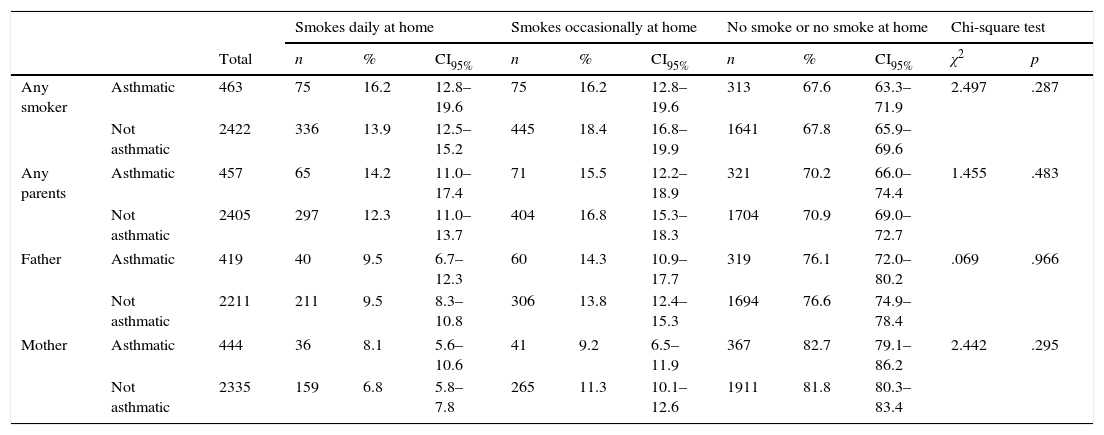
Of the 3187 children, 32.6% were exposed to SHS at home and 29.2% inside the car. Among smokers, 69.8% of mothers and 56.8% of fathers smoked at home. Mothers usually smoked in the kitchen (29.7%) and fathers tended to smoke near open windows or doors (28.1%). Table 2 shows that 32.3% of non-asthmatic children were exposed to SHS because at least one of their household members smoked at home (daily and occasionally); 29.1% had at least one parent who smoked at home (daily and occasionally); 23.3% had a father who smoked at home (daily and occasionally); and 18.1% had a mother who smoked at home (daily and occasionally).
Prevalence of secondhand smoke exposure at home in the asthmatic and not asthmatic children.
| Smokes daily at home | Smokes occasionally at home | No smoke or no smoke at home | Chi-square test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | n | % | CI95% | n | % | CI95% | n | % | CI95% | χ2 | p | ||
| Any smoker | Asthmatic | 463 | 75 | 16.2 | 12.8–19.6 | 75 | 16.2 | 12.8–19.6 | 313 | 67.6 | 63.3–71.9 | 2.497 | .287 |
| Not asthmatic | 2422 | 336 | 13.9 | 12.5–15.2 | 445 | 18.4 | 16.8–19.9 | 1641 | 67.8 | 65.9–69.6 | |||
| Any parents | Asthmatic | 457 | 65 | 14.2 | 11.0–17.4 | 71 | 15.5 | 12.2–18.9 | 321 | 70.2 | 66.0–74.4 | 1.455 | .483 |
| Not asthmatic | 2405 | 297 | 12.3 | 11.0–13.7 | 404 | 16.8 | 15.3–18.3 | 1704 | 70.9 | 69.0–72.7 | |||
| Father | Asthmatic | 419 | 40 | 9.5 | 6.7–12.3 | 60 | 14.3 | 10.9–17.7 | 319 | 76.1 | 72.0–80.2 | .069 | .966 |
| Not asthmatic | 2211 | 211 | 9.5 | 8.3–10.8 | 306 | 13.8 | 12.4–15.3 | 1694 | 76.6 | 74.9–78.4 | |||
| Mother | Asthmatic | 444 | 36 | 8.1 | 5.6–10.6 | 41 | 9.2 | 6.5–11.9 | 367 | 82.7 | 79.1–86.2 | 2.442 | .295 |
| Not asthmatic | 2335 | 159 | 6.8 | 5.8–7.8 | 265 | 11.3 | 10.1–12.6 | 1911 | 81.8 | 80.3–83.4 | |||
Note: CI, confidence interval; OR, odds ratio.
We found that 472 children had asthma, 58.5% of them males. Thus, asthma prevalence was 14.8%. Of the 472 children with asthma, 22.3% used asthma medication; 18.3% were diagnosed with asthma; and 14.8% used an asthma specific inhaler. Results showed that 32.4% children with asthma were exposed to SHS because at least one of their household members smoked (daily and occasionally); 29.7% had at least one parent who smoked at home (daily and occasionally); 23.8% had a father who smoked at home (daily and occasionally); and 17.3% had a mother who smoked at home (daily and occasionally). We did not observe any significant differences between non-asthmatic and asthmatic children's SHSe (Table 2).
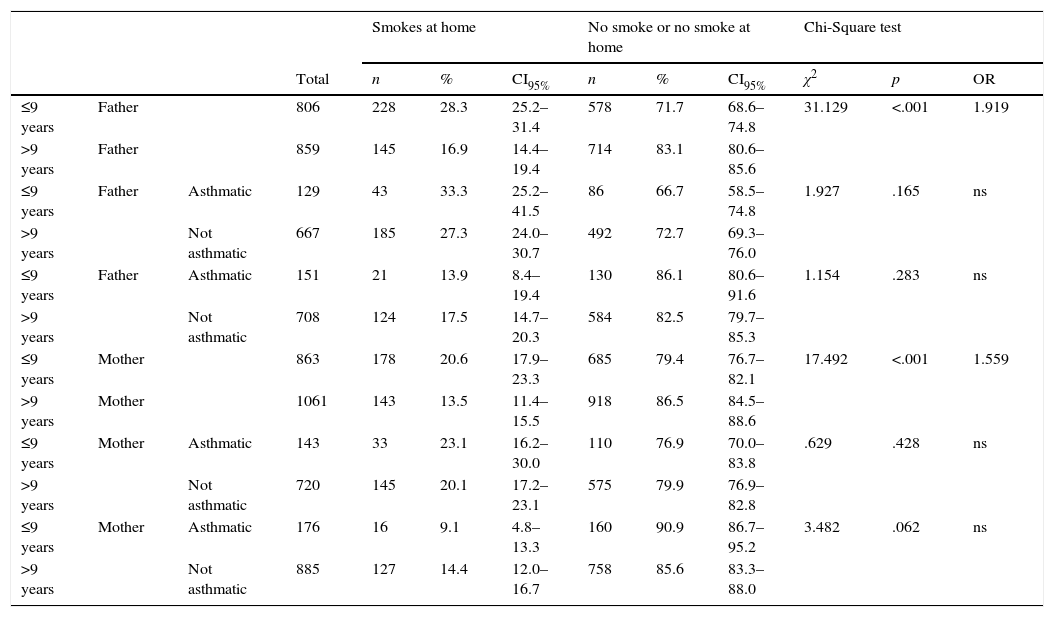
Smoking at home was more frequent in parents with a low education level (mothers p<.001; fathers p<.001), as shown in Table 3.
Parents’ school years and secondhand smoke risk exposure in the asthmatic and not asthmatic children.
| Smokes at home | No smoke or no smoke at home | Chi-Square test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | n | % | CI95% | n | % | CI95% | χ2 | p | OR | |||
| ≤9 years | Father | 806 | 228 | 28.3 | 25.2–31.4 | 578 | 71.7 | 68.6–74.8 | 31.129 | <.001 | 1.919 | |
| >9 years | Father | 859 | 145 | 16.9 | 14.4–19.4 | 714 | 83.1 | 80.6–85.6 | ||||
| ≤9 years | Father | Asthmatic | 129 | 43 | 33.3 | 25.2–41.5 | 86 | 66.7 | 58.5–74.8 | 1.927 | .165 | ns |
| >9 years | Not asthmatic | 667 | 185 | 27.3 | 24.0–30.7 | 492 | 72.7 | 69.3–76.0 | ||||
| ≤9 years | Father | Asthmatic | 151 | 21 | 13.9 | 8.4–19.4 | 130 | 86.1 | 80.6–91.6 | 1.154 | .283 | ns |
| >9 years | Not asthmatic | 708 | 124 | 17.5 | 14.7–20.3 | 584 | 82.5 | 79.7–85.3 | ||||
| ≤9 years | Mother | 863 | 178 | 20.6 | 17.9–23.3 | 685 | 79.4 | 76.7–82.1 | 17.492 | <.001 | 1.559 | |
| >9 years | Mother | 1061 | 143 | 13.5 | 11.4–15.5 | 918 | 86.5 | 84.5–88.6 | ||||
| ≤9 years | Mother | Asthmatic | 143 | 33 | 23.1 | 16.2–30.0 | 110 | 76.9 | 70.0–83.8 | .629 | .428 | ns |
| >9 years | Not asthmatic | 720 | 145 | 20.1 | 17.2–23.1 | 575 | 79.9 | 76.9–82.8 | ||||
| ≤9 years | Mother | Asthmatic | 176 | 16 | 9.1 | 4.8–13.3 | 160 | 90.9 | 86.7–95.2 | 3.482 | .062 | ns |
| >9 years | Not asthmatic | 885 | 127 | 14.4 | 12.0–16.7 | 758 | 85.6 | 83.3–88.0 | ||||
Note: CI, confidence interval; OR, odds ratio; ns, not significant.
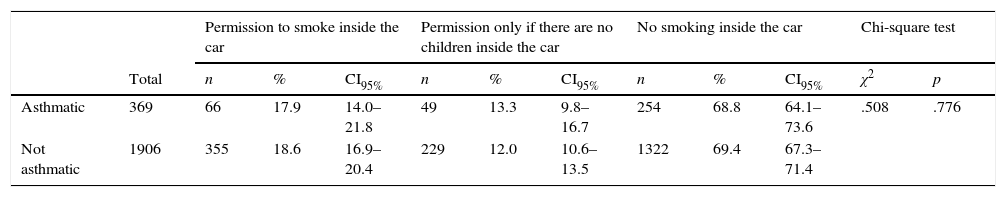
Table 4 shows that 18.6% of non-asthmatic children and 17.9% of asthmatic children were exposed to SHS inside the car. We did not observe any significant differences between non-asthmatic and asthmatic children's SHSe inside the car.
Prevalence of secondhand smoke exposure inside the car in asthmatic and not asthmatic children.
| Permission to smoke inside the car | Permission only if there are no children inside the car | No smoking inside the car | Chi-square test | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | n | % | CI95% | n | % | CI95% | n | % | CI95% | χ2 | p | |
| Asthmatic | 369 | 66 | 17.9 | 14.0–21.8 | 49 | 13.3 | 9.8–16.7 | 254 | 68.8 | 64.1–73.6 | .508 | .776 |
| Not asthmatic | 1906 | 355 | 18.6 | 16.9–20.4 | 229 | 12.0 | 10.6–13.5 | 1322 | 69.4 | 67.3–71.4 | ||
Note: CI, confidence interval.
The present study aimed to be the first questionnaire-based cross-sectional study to evaluate school-aged children SHSe in a representative sample of nine Portuguese cities. The results showed that one-third of Portuguese asthmatic children were exposed to SHS at home. Equal SHSe was found among non-asthmatic and asthmatic children at home and inside the family vehicle. These results are similar to the ones found in other countries: a third of asthmatic American children were exposed to SHS inside the car,13 but recently the number significantly decreased to one-fifth.17 Also in the USA, 39% of families reported at least one smoker at home.12
The asthma prevalence in this study was 14.8%. In the USA, asthma prevalence has been estimated as 14.4%.18 In Portugal, a previous study targeting children has reported 15.7% asthma prevalence.5 Asthma prevalence in this study was also similar to the prevalence found in the International Study of Asthma and Allergies in Childhood in Portugal.5 Asthma diagnosis in children at this age is frequent and accurate.6
Parents with a low education level smoked more at home and therefore their children were more exposed to SHS.
This study has some limitations that should be discussed. With all data being self-reported and taking into account the non-response rate (22.5%), SHSe underestimation must be considered. However, previous studies have stated that self-reported SHSe questionnaires tend to be valid.19 Also, although our response rate was high,20 we should consider non-response bias. One of the reasons for non-response was the fact that the inclusion of children in the study depended on a parents’ written consent. Although it is not possible to assess the pattern of non-response bias, because the characteristics of those who did not participate are not available, some literature have shown that non-respondents tend to differ from respondents in terms of several socio-demographic and economic variables that can be linked to lifestyles, attitudes and beliefs.21 We can hypothesise that there is a possibility that the non-respondents are less aware of the negative impact of the SHS exposure among children, which could mean that the real exposure is be higher than the values presented. Another limitation was asthma definition. Asthma diagnosis in younger children may be difficult, since suggestive asthma symptoms are not asthma-specific, thus the use of asthma inhaler can be a better diagnosis criteria.7 And, finally, we did not use objective bio-markers for evaluating children's exposure to SHS. The gold standard bio-marker for SHSe is cotinine measurement in plasma, urine or saliva. Past research had identified two questions that predicted high cotinine children measurements: (1) whether the primary caregiver smoked and (2) permission to smoke at children's home.21 These two questions were included in our questionnaire and there was a good correlation between exposure evaluated by questionnaires and children cotinine levels.22 Quantification of SHS should be a target in future research.
In 2008, Portugal implemented a partial smoking ban. This study showed that the ban is not being effective in protecting children from SHSe at home and inside the car. Only 100% smoke-free policies promote smoke-free homes. Comprehensive tobacco control policies such as raising tobacco taxes, 100% smoke-free policies, public health campaigns promoting cessation and smoke-free environments (including awareness of SHSe health hazards) should be implemented. Doctors, particularly paediatricians, should provide smoking cessation counselling to all parents who smoke and especially to those who have an asthmatic or a wheezing child.10 If cessation is not possible, they should promote a smoke-free home and a smoke-free car.
ConclusionThe current study provides relevant findings about the prevalence of children's SHSe in Portugal. It can be concluded that asthmatic and non-asthmatic children are equally exposed to SHS at home and inside the car. These findings highlight the need to prevent parental smoking and to promote 100% smoke-free environments, including smoke-free homes and cars. Brief but effective SHSe advice should be included in paediatric asthma management and control.
Authors’ contributionJosé Precioso, Henedina Antunes, Catarina Samorinha, Elisardo Becoña, Sofia Belo-Ravara, Paulo Vitória conceived this study and supervised all aspects of its implementation. Ana-Carolina Araújo and Sofia Belo-Ravara collected the data and collaborated in the analysis. José Precioso and José Cunha Machado designed and carried out statistical analysis. Vânia Rocha revised the manuscript critically, helped to write its final version and contributed to the interpretation of data for the work. Henedina Antunes wrote the first draft of the manuscript. All authors gave a substantial contribution to the interpretation of data, critical discussion and revision of the manuscript, and approved its final version.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors declare no conflict of interest.
This study was supported through FEDER from the Operational Programme Factors of Competitiveness – COMPETE and through national funding from the Foundation for Science and Technology – FCT (Portuguese Ministry of Education and Science) (FCOMP-01-0124-FEDER-009117). The authors also thank the “Sociedade Portuguesa de Pediatria” by the prize attributed to the communication on this topic in the National Conference of Pediatrics, in October 2012.