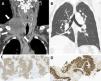
A 56-year-old white male presented with a voluminous right supraclavicular node with 2 months of evolution. He was a railroad worker, a heavy smoker and with no past medical history. The physical examination revealed a voluminous palpable, non-movable, right supraclavicular node. A cervical and thoracic CT scan was performed and revealed a voluminous heterogeneous right laterocervical mass, measuring 94 × 65 mm in greater diameter, involving the ipsilateral internal jugular vein and associated with multiple mediastinal and hilar nodes (Fig. 1 – A and B). He underwent an incisional biopsy of this right supraclavicular mass and pathology result was compatible with a large cell neuroendocrine carcinoma (LCNEC) of the lung. Immunohistochemistry was positive for neuroendocrine markers, including chromogranin A, synaptophysin (Fig. 1 - C), CD56 and Ki67, and for thyroid transcription factor-1 (TTF-1) (Fig. 1 - D). The Ki67 index was >90%. There was also evidence of right adrenal gland and multiple brain metastases. He underwent radiation therapy on the right supraclavicular mass and cranial. Following worsening of his general and neurological condition, the patient died and it was not possible to start his cytostatic treatment.
Cervical (A) CT scan revealed a voluminous heterogeneous right laterocervical mass, involving the ipsilateral internal jugular vein (white arrows). Thoracic (B) CT scan revealing multiple mediastinal and hilar nodes (white arrowheads) with no pulmonary findings. Immunohistochemistry from biopsy of the right supraclavicular mass whose pathology result was compatible with a large cell neuroendocrine carcinoma of the lung: positivity for neuroendocrine markers, including synaptophysin (C) and for thyroid transcription factor-1 (TTF-1) (D).
The authors report a patient with a LCNEC of the lung with an atypical presentation and no pulmonary findings on the CT scan and also with no respiratory complaints but where biopsy was fundamental to obtaining the correct histopathological diagnosis. The authors also highlight two specific and uncommon features present in these case: the majority of mediastinal LCNEC originate from the thymus1 and pulmonary LCNEC are less likely to present with advanced stage disease.2