A 70-year-old woman with a 3-year history of progressive voice hoarseness was diagnosed with primary localized subglottic amyloidosis. Her medical history consisted of treated osteoporosis, hypothyroidism, and arterial hypertension, and a history of smoking six packs of cigarettes per year. The patient was referred to our department for bronchoscopic evaluation in the setting of worsened hoarseness.
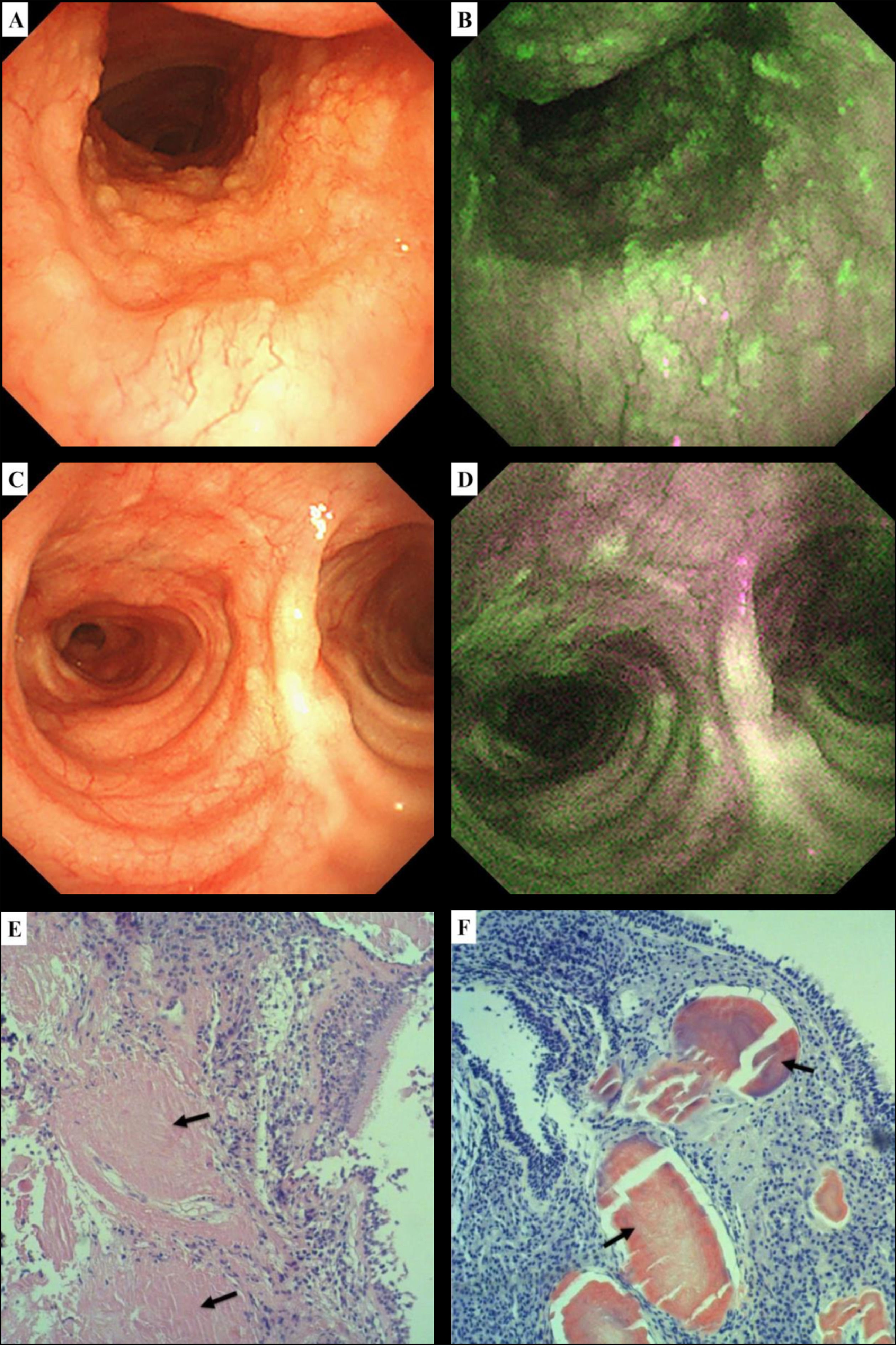
White light bronchoscopy (WLB) revealed nodular mucosa irregularities along the anterior tracheal wall extending from 3 cm below the vocal cords to the main carina (Fig. 1A). Upon switching to autofluorescence imaging bronchoscopy (BF-F260, Olympus Optical Co., Tokyo, Japan), green spots surrounded by diffuse magenta amyloid plaques were observed (Fig. 1B). A flat pathological magenta lesion on the posterior tracheal wall near the main carina was made visible by the autofluorescence light but was not visible using WLB (Fig. 1C and 1D). Abundant deposits of amyloid within the submucosal tissue were present in the five biopsies taken from the proximal anterior tracheal wall to the main carina (Fig. 1E and 1F).
White light bronchoscopy (WLB) showing nodular mucosa irregularities along the anterior tracheal wall up to the carina (A); upon switching to autofluorescence imaging bronchoscopy, green spots interweaved with magenta areas are visible (B). Normal-appearing main carina on WLB (C); using autofluorescence imaging bronchoscopy, a flat pathological magenta lesion is now visible near the posterior tracheal wall (D). Tracheal biopsy showing abundant amorphous amyloid deposits within the submucosal tissue on standard haematoxylin-eosin staining (E, black arrows). Congo red staining demonstrates the characteristic orange-red appearance of amyloid deposits (F, black arrows).
Localized tracheobronchial amyloidosis (TBA) is a very uncommon disease, with only a few hundred cases ever reported. TBA is characterized by extracellular amyloid infiltration throughout the proximal, mid, and lower airways.1 The endoscopic features of TBA are variable and include intraluminal nodules, luminal stenosis, bronchial wall thickening or rigidity, brittle and easily bleeding mucosa, mucosal unevenness, hyperemia, edema, or paleness.2 The use of autofluorescence imaging to look for amyloid deposition has been described in retinal imaging but has only been investigated for airway imaging in one case report.3
In our case, switching to autofluorescence endoscopy enabled us to observe the extent of tracheal infiltration by amyloid deposits and guided the choice of biopsy sites when we found that the conventional WLB view was not accurate enough. This technique may, therefore, be of interest for the assessment of suspected cases of TBA.
Patient's consentInformed consent was obtained for publication
FundingThe present manuscript did not have any source of support.
Author contributionConception and design: VI, MG, MB, VN - Acquisition of the data: MG, RDW, VN -
Drafting of the manuscript: VI - Critical revision of the manuscript: MB, VN, RDW, MG