Lung cancer is the deadliest cancer worldwide. In Portugal, the disease remains the main cause of cancer death in males.
AimThis study aims to evaluate the demographic and clinical characteristics of lung cancer patients diagnosed and treated in northern Portugal hospitals from 2000 to 2010.
Patients and methodsTwelve hospitals in the north of Portugal contributed to this study. The demographic and clinic characteristics of the patients registered in each hospital from 2000 to 2010 and the patterns of their occurrence were analyzed.
ResultsDuring an 11-year period (2000–2010), 9767 lung cancer patients were registered in the participating hospitals. Comparing the number of the patients registered in the year 2000 to those registered during 2010, there was a significant increase in lung cancer cases. Females represent only 20% of the total registered lung cancer cases; however, during the study period, the number of female patients increased by 30%. A significant number of the patients, 3117 (48.6%), had poor performance status at presentation. The adenocarcinoma histology became more preponderant over the study period. Most of the patients were diagnosed as stages IIIB or IV: 7206 of 9267 (77.8%). Chemotherapy was the treatment of choice for 3529 (40.4%) patients, whereas surgical treatment was achieved in 1301 (14.9%) cases.
ConclusionA significant number of lung cancer patients have been diagnosed and treated in hospitals in northern Portugal, and the incidence of the disease among females has been increasing. The overwhelming majority of the tumors were diagnosed in advanced stage; nevertheless, surgical treatment was possible in 14.9% of the patients.
O cancro do pulmão é o cancro que mais mortalidade determina em todo mundo. Em Portugal a doença mantém-se a principal causa de morte por cancro no sexo masculino.
ObjetivoNeste estudo pretendeu-se avaliar as características demográficas e clínicas dos doentes com cancro do pulmão diagnosticados e tratados nos hospitais do norte de Portugal entre os anos 2000-2010.
Doentes e métodosDoze hospitais contribuíram para este estudo. Foram analisadas as características demográficas e clínicas dos doentes com cancro do pulmão registados em cada hospital, entre os anos 2000-2010, nos hospitais do norte de Portugal, bem como os padrões de ocorrência da doença.
ResultadosAo longo de um período de 11 anos (2000-2010), 9.767 doentes com cancro do pulmão foram registados nos hospitais participantes. Identificamos um importante aumento no número de doentes registados em relação aos registados em 2000. No sexo feminino observou-se uma elevação da ocorrência atingindo os 30%, o que é significativo, apesar do cancro do pulmão nas mulheres, em Portugal, ser muito menos frequente que nos homens e nesta série representar apenas 20% dos casos. Um número elevado de doentes, 3.117 (48,6%), tinha mau estado geral na altura que recorreram aos cuidados de saúde. O adenocarcinoma foi-se tornando a histologia mais preponderante ao longo do período de estudo. A maior parte dos doentes, 7.206 (77,8%), foi diagnosticada em estádios avançados (IIIB, IV) da doença. A quimioterapia foi o tratamento escolhido para 3.529 (40,4%) dos doentes, por outro lado, a cirurgia foi possível em 1.301 (14,9%) dos casos.
ConclusãoUm elevado número de doentes com cancro do pulmão é diagnosticado e tratado nos hospitais do norte de Portugal. A incidência no sexo feminino tem vindo a aumentar. A esmagadora maioria dos tumores foi diagnosticada em estádio avançado, tendo sido possível, apesar disso, tratar cirurgicamente 14,9% dos doentes.
Lung cancer is the deadliest cancer worldwide.1 In 2008, 1.61 million new cases were diagnosed and 1.38 million of deaths occurred,1 illustrating the aggressiveness of the disease.
In Portugal, lung cancer remains the main cause of cancer death in males.1 Over the past 50 years until the 1990s, lung cancer mortality had increased sharply; in recent years, however, it has slowed down among males.2 Female lung cancer patients represent only 20% of the total number of cases in Portugal, but a growing trend has been observed in the last few years.2,3
The importance of obtaining knowledge about lung cancer trends in the northern part of Portugal and the need to harmonize diagnostic and therapeutic strategies has always been recognized. These were the goals of a group of lung specialists in northern Portugal when they started a discussion forum specifically to deal with these matters. These chest physicians voluntarily worked together for more than a decade, discussing clinical cases with problematical or unusual features. Afterwards, they expanded their interests to recent technological and scientific developments and to the study of the epidemiology of the disease in the region where they work.
AimThe study aims to investigate the demographic and clinical characteristics of lung cancer patients diagnosed from 2000 to 2010 in hospitals in northern Portugal, as well as to identify and describe the patterns of lung cancer occurrence and the strategies for treatment during the same interval.
Patients and methodsTwelve hospitals contributed to this study (Centro Hospitalar Vila Nova de Gaia, Centro Hospitalar S. João, Instituto Português Oncologia-Porto, Centro Hospitalar Vila Real e Trás os Montes, Hospital S. Marcos (Escala Braga), Hospital Pedro Hispano, Centro Hospitalar Alto Minho, H. Guimarães, Centro Hospitalar entre Vouga Douro, H. Famalicão, H. Barcelos e H. Joaquim Urbano). Accrual of patients in each hospital followed the usual clinical conditions, that is, by self-reference (symptomatic people who seek medical attention at the Urgency or General Consultation units) or by referral from other hospitals or clinics to clarify symptoms, signs, or suspicious changes in diagnostic procedures often performed for another reason. When diagnosis and treatment had been done in different hospitals, for patient registration purposes, only the hospital responsible for the treatment was taken into consideration. The year of diagnosis, the hospital where patients were diagnosed/treated, sex, age, smoking habits, performance status (PS), histology/cytology, stage (TMN), the first treatment option, and the date of death were included in an anonymous database. In this study, all the characteristics listed in that database, except survival, were analyzed. The characteristics were transformed, as appropriate, into continuous or discrete variables before analysis. Using the variable PS, a new dichotomic variable was generated to classify the patients into two categories: those with no or a slight general condition compromise (PS 0 or 1, codified as “0”) and those with significant daily life limitation (PS 2 or more, codified as “1”). Because this is a multiyear study, we analyzed the trends of some variables and the interaction between them. We used as reference the data on lung cancer incidence and mortality published in international databases.2,3 Performance status determinants at presentation were estimated, computed with the use of STATA Statistical Data Analysis 9.04 and MIX 2.0 BiostatXL 2010.5
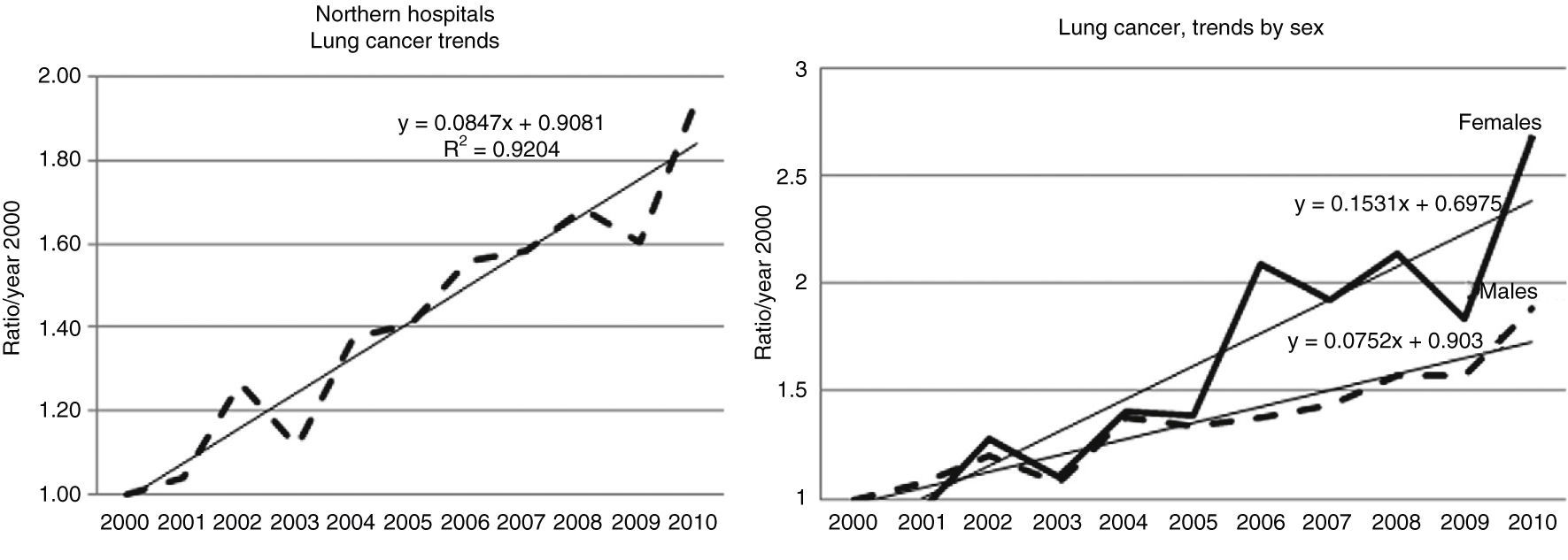
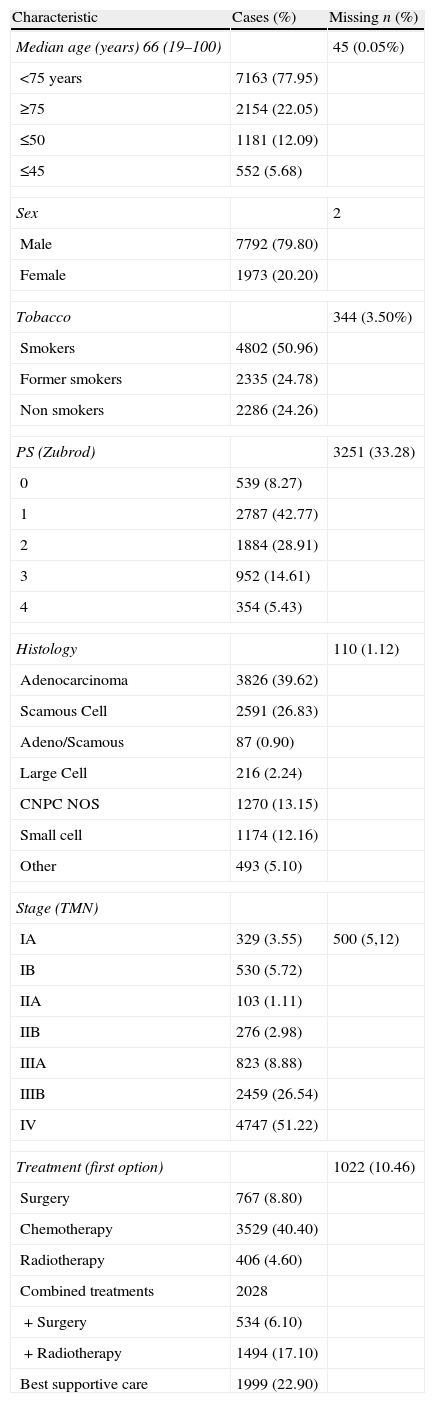
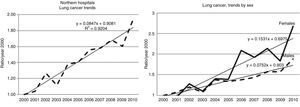
ResultsThroughout the study period, 9767 patients with lung cancer were registered (Table 1). There was an increase in the absolute number of cancer cases registered in all hospitals during the study (Fig. 1). The 634 lung cancer cases registered by the year 2000 correspond to the 1284 cases in 2010 (*Suppl. – Table 1).
Patient's data.
| Characteristic | Cases (%) | Missing n (%) |
| Median age (years) 66 (19–100) | 45 (0.05%) | |
| <75 years | 7163 (77.95) | |
| ≥75 | 2154 (22.05) | |
| ≤50 | 1181 (12.09) | |
| ≤45 | 552 (5.68) | |
| Sex | 2 | |
| Male | 7792 (79.80) | |
| Female | 1973 (20.20) | |
| Tobacco | 344 (3.50%) | |
| Smokers | 4802 (50.96) | |
| Former smokers | 2335 (24.78) | |
| Non smokers | 2286 (24.26) | |
| PS (Zubrod) | 3251 (33.28) | |
| 0 | 539 (8.27) | |
| 1 | 2787 (42.77) | |
| 2 | 1884 (28.91) | |
| 3 | 952 (14.61) | |
| 4 | 354 (5.43) | |
| Histology | 110 (1.12) | |
| Adenocarcinoma | 3826 (39.62) | |
| Scamous Cell | 2591 (26.83) | |
| Adeno/Scamous | 87 (0.90) | |
| Large Cell | 216 (2.24) | |
| CNPC NOS | 1270 (13.15) | |
| Small cell | 1174 (12.16) | |
| Other | 493 (5.10) | |
| Stage (TMN) | ||
| IA | 329 (3.55) | 500 (5,12) |
| IB | 530 (5.72) | |
| IIA | 103 (1.11) | |
| IIB | 276 (2.98) | |
| IIIA | 823 (8.88) | |
| IIIB | 2459 (26.54) | |
| IV | 4747 (51.22) | |
| Treatment (first option) | 1022 (10.46) | |
| Surgery | 767 (8.80) | |
| Chemotherapy | 3529 (40.40) | |
| Radiotherapy | 406 (4.60) | |
| Combined treatments | 2028 | |
| +Surgery | 534 (6.10) | |
| +Radiotherapy | 1494 (17.10) | |
| Best supportive care | 1999 (22.90) | |
From 2000 to 2010, the registered lung cancer patients consisted of 7792 (79.8%) males and 1973 (20.2%) females. Both showed a persistent increase throughout this 11-year period; however, among women, the growth pattern seems sharper (Fig. 1). The median age was 66 years (Table 1). Only 5% of the patients were aged 45 years or younger, and 22% of cases were 75 years or more (Table 1).
The smoking habits of lung cancer patients are gender-related. Whereas the smokers and ex-smokers with lung cancer are mostly males, the overwhelming majority of nonsmokers with lung cancer are women. The occurrence of lung cancer in nonsmokers remained stable, whereas a small increase was found among former smokers (Suppl. Fig. 2).
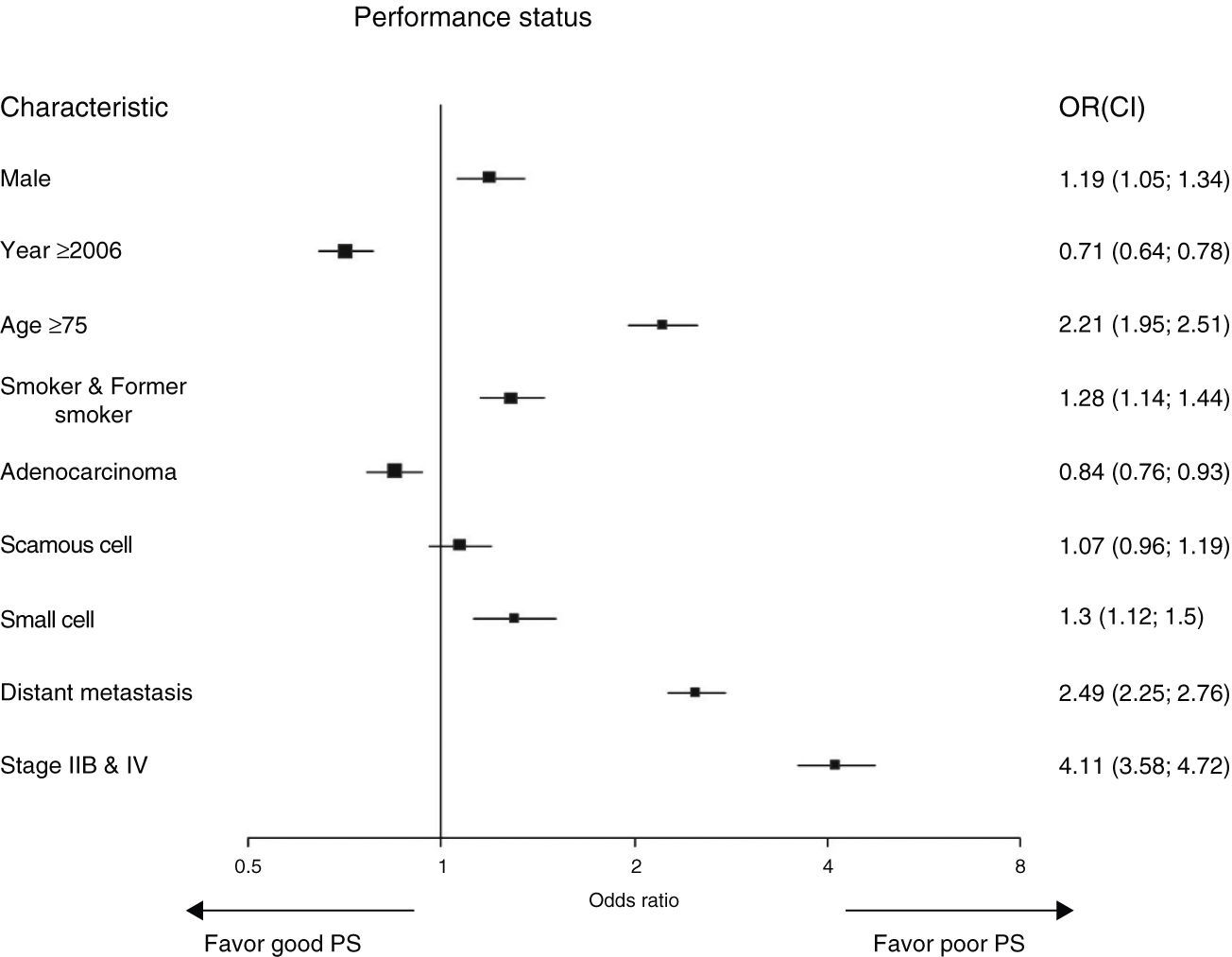
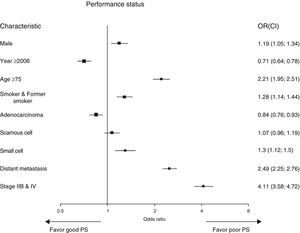
The performance status was evaluated in only 6395 patients (67.4%; Table 1). A large number of the patients, 3162 (48.5%), had significant general condition compromise: 1851 cases (28.9%) with PS 2 and 1257 (19.6%) with PS 3 and 4. We found (Fig. 2) a statistically significant interaction between PS and gender, year of diagnosis, age group, smoking habits, cytology/histology, extensive stage, and metastatic disease. The patients with poor PS tended to be males, older, smokers or former smokers, and small cell lung cancer cases with disseminated disease at presentation and whose diagnosis had been established at the beginning of the study period (Fig. 2).
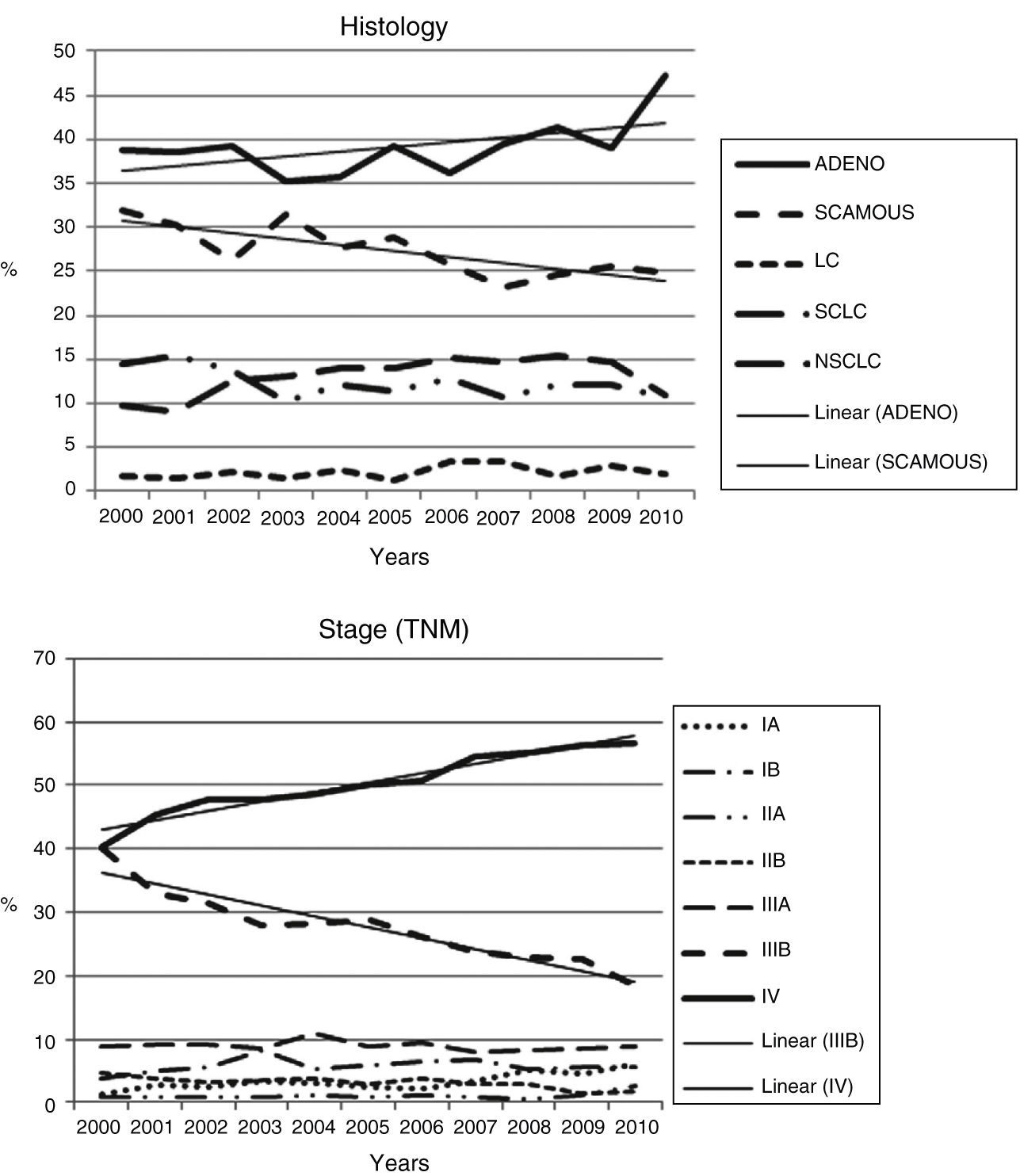
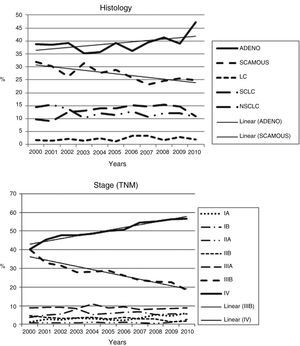
Cellular type adenocarcinoma became more dominant (Fig. 3) over the period of study, whereas squamous cell and small cell carcinomas decreased.
An overwhelming predominance of advanced cancers was observed in 6997 patients (77.7%): 2388 (25.2%) in stage IIIB and 4609 (48.6%) in stage IV. A gradual but clear reduction in stage IIIB cases and an increase in stage IV cases were observed throughout the study period (Fig. 3).
There has been an increase in application of multimodal treatment strategies for lung cancer. Almost one-fourth of the patients, 2028 (23.2%), were treated using a multimodal treatment strategy (Table 1).
For 1999 (22.9%) patients, the only possible initial treatment was the best supportive care. For a significant number of the patients, 3529 (40.4%), chemotherapy was the first treatment option. Surgery was chosen as a single treatment in 761 (8.8%) cases. A combined strategy as first-line therapy was the choice for 2028 (23.2%) patients, whereas radiotherapy as a single treatment was used in only 406 (4.6%) patients.
Compared to 2001, combined modalities including surgery, in 2010, accounted for double the number of the patients. This strategy had a huge influence on the proportion of patients treated with surgery, which increased from 8.8% to 14.9%.
DiscussionThis study was made possible by the persistence and willingness to improve of all the physicians in the lung cancer field working in hospitals in northern Portugal. In addition to meeting many of our expectations, the analysis we conducted also revealed certain findings that need discussion and, ultimately, require explanation.
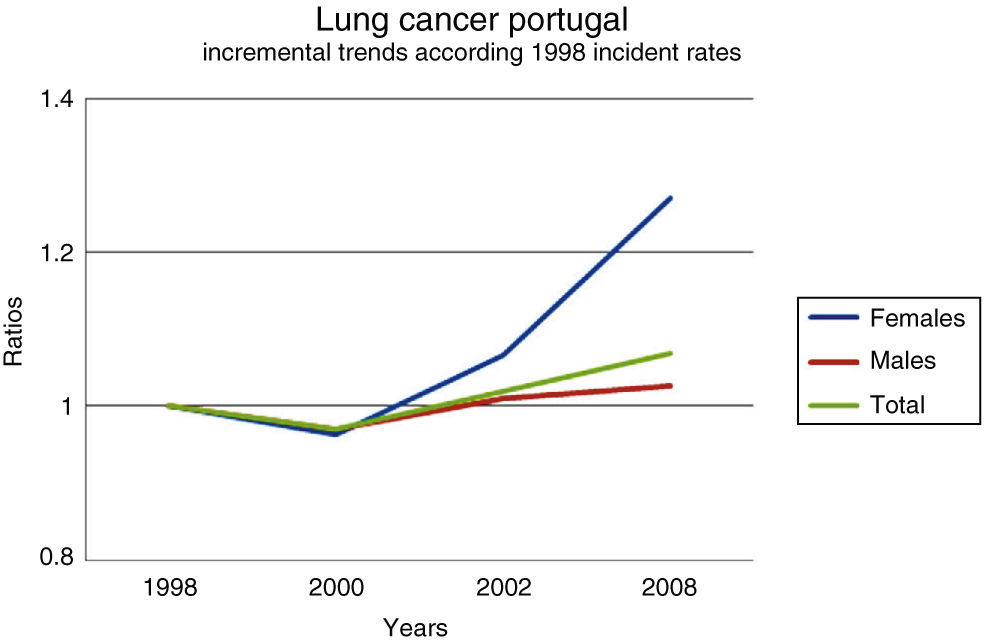
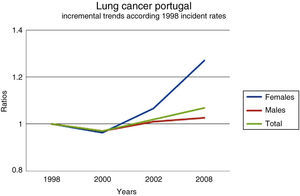
The first challenge is related to the huge increase in registered lung cancer cases, which doubled over the study period. This trend is not easy to explain, as looking at the incidence of lung cancer cases and the mortality rates in Portugal, for the same period,1,2,3,6,7 there is no valid reason for this increase (Fig. 4). Lung cancer incidence did increase somewhat but not enough to explain the figures registered in the hospitals studied.3,6,7
Lung cancer incidence in Portugal7 (from the OECD Health Data 2011).
This leaves either one or both of two possible explanations: registry failures and non-exhaustive patient referrals to the diagnostic and treatment centers, mainly at beginning of the study period. These explanations are hard to accept considering the characteristics and aggressiveness of the disease, which means we did not find a completely satisfactory explanation for the increase in lung cancer cases. Lung cancer primarily afflicts individuals over the age of 60 years. Young adults account for only 5% of cases (<45 years)6,7; however, among people 45–50 years old, the number of registered cases doubled (Table 1).
Another important issue is related to the pattern of occurrence of lung cancer among females, which showed a higher increase than expected. This occurrence was apparently not linked to smoking habits (*Suppl. Figs. 1 and 2). In Portugal, female lung cancer patients accounted for 20–25% of the total lung cancer cases in 2008.7 These figures are quite similar to the proportion of lung cancer diagnosed in females during the study, which was around 20%, a long way from the 34.5% lung cancer incidence in females in the “eurozone”.1,3
Smoking was the single most common cause of disease given by at least 80% of lung cancer patients. The proportion of lung cancer in nonsmokers was slightly more than 20%. Throughout the study period, it is worth noting that the proportion of lung cancers stabilized in nonsmokers, progressively decreased in smokers, and increased in former smokers. This pattern of occurrence7–10 could be related to changes in attitude within society regarding smoking and fear of the risk of lung cancer.
The performance status of the patients represents a decisive factor in the choice of treatment. Evaluation of the repercussion of the disease on PS shows that, although the majority of patients were in good physical condition at the time of diagnosis, 48.6% of them were severely limited. Unlike other malignancies, the rather large proportion of patients with poor PS is an unusual occurrence among lung cancer patients.11 In our study, the proportion of patients with good PS increased over the study period. In the past decade, better socioeconomic conditions could explain the better PS. During the decade in which the study was conducted, there was a significant change in how and where people lived. This could, at least in part, explain the better PS without any stage shift. This trend could be related to patients’ easy access to specialized lung cancer centers. However, this explanation is difficult to justify because it was not associated with a higher proportion of tumors diagnosed at early stages.12–14 The proportion of tumors that are potential candidates for surgical treatment remained stable, whereas locally advanced disease – stage IIIB – decreased in the same proportion as the increase in metastatic tumors. These changes between stages IIIB and IV seem to indicate the clear influence of a well-known phenomenon that explains stage migration: the “Will Rogers phenomenon”.15 The most probable explanation is the use of a new staging method that allows for more accurate classification.
The predominance of adenocarcinoma and the consequent reduction in squamous cell and small cell carcinomas are other important issues that occurred during the study period. These changes, although not yet completely clarified, seem to be related with changes in the type of tobacco the patients smoked9,10 and their possible consequences (changes in the particle dimensions and the lung areas affected). Moreover, new techniques of pathology evaluation and new classifications may have influenced our results.
Regardless of all these efforts, the reality remains that year after year, nearly 80% of the patients in the northern hospitals had extensive disease at diagnosis, so that they would not qualify them as candidates for potentially curative treatment. Given this situation, the treatment option for most of these patients was chemotherapy, and the only option for almost 2000 patients was the best supportive care. This is not a unique situation; unfortunately, it happens more or less worldwide and should be a stimulus for research into new strategies to avoid such a large number of patients being diagnosed at such a late stage of the disease. Screening for lung cancer could be the answer, but further evidence is needed. Surgery is still the best treatment option we have at present; however, only a small proportion of patients, 767 (8.8%), qualified as candidates without restrictions. Combinations of chemotherapy and/or radiotherapy before and after surgical interventions allowed for the recovery of potential curative treatment patients, who otherwise could not have benefitted from this strategy. Throughout the 11-year study period, this strategy allowed 534 (6.1%) patients to recover for surgical treatment, increasing the proportion of patients operated by 41% (6.1% of 14.9%) and, thus, the consequent expectation of better quality of life and survival. Additionally, the possibility of widespread use of target therapies (tyrosine kinase inhibitors), not only as second- and third-line treatments but as a first-line option for patients with extensive disease harboring active EGFR mutations and EML-ALK translocations, could influence the global life survival of lung cancer patients.
ConclusionThe lung cancer cases diagnosed and treated in hospitals in northern Portugal accounted for 1059 (32.2%) of the 3288 total cases registered in the country in 2008. Based on the same total incidence (3288), the proportion of lung cancer cases in the northern hospitals could be said to have increased to 39.5% (1284) in 2010.
The evolution of lung cancer among females is relevant and should be monitored. The high proportion of advanced lung cancer cases diagnosed each year is, unfortunately, a reality that entails huge economic and social costs. Given the socioeconomic burden of the disease and the resources involved in diagnosis, treatment, and palliative care, lung cancer should be included in the national respiratory health strategy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank all our colleagues at the Pneumologia Oncológica do Norte de Portugal for their excellent work and continuing efforts in recording patient data.
Please cite this article as: Hespanhol V, Parente B, Araújo A, Cunha J, Fernandes A, Figueiredo MM, et al. Cancro do pulmão no norte de Portugal: um estudo de base hospitalar. Rev Port Pneumol. 2013;19:245–251.