Investment in respiratory disease research (RD) in primary care in Portugal is needed to assess the size of the problem and to develop appropriate clinical strategies to deal with it. The research agenda presented in 2013 in the National Health Plan and National Health Program Priorities1 lists a set of research needs in Primary Care. A Delphi study was published in 2016 in which consensus on national research priorities in respiratory diseases in primary care was achieved.2 However, there is little systematic knowledge of published research on respiratory diseases in primary care in Portugal.
We conducted a study to identify and characterise the studies on respiratory diseases carried out in Primary Care in Portugal over a decade. We assessed the issues addressed, the methodologies used, the scope and dimensions of the studies and the impact of research.
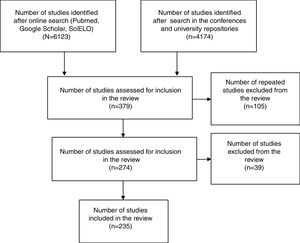
Between October and December 2015 we searched the Medline, Google Scholar, SciELO databases, the Index of Portuguese Medical Journals, the ‘grey literature’ for proceedings of family medicine scientific meetings held between 2010 and 2015, and university repositories of theses and publications. We used the National Library of Medicine MeSH terms ‘asthma’ ‘COPD’ ‘respiratorydiseases’ ‘respiratory’ ‘pneumonia’, ‘respiratoryinfections’ ‘sinusitis’, ‘rhinitis’ and ‘primary care’ and ‘Portugal’. We included studies published between 2005 and 2015, in Portuguese or English, with at least one Portuguese author from Primary Care, or studies whose participants were Portuguese and recruited from Primary Care (Fig. 1).
A total of 235 studies were analysed, of which 67 were studies published at a national or international level and 168 were studies presented at conferences. The complete list of studies identified is available from the authors.
We found 35 studies (52%) published in national journals, 20 (30%) in international journals, and 12 (18%) academic theses (ten master's degrees, one post-graduate and one doctorate), which were unpublished.
While 90% of all publications in international journals were cited at least once, only 40% of the national publications were cited. Only one of 12 theses was cited.
The most common methods used were cross sectional studies and literature reviews, both at a national level and international level. The other types of study methods were similarly distributed. At national conferences, reviews were more common (n=66) than cross-sectional studies (n=43) or case reports (n=33).
Asthma, allergic rhinitis, smoking, and COPD were the topics most often studied. (Table 1) Studies of asthma and allergic rhinitis produced 25 publications including 15 cross-sectional studies, 3 review articles, 2 validation studies, 1 retrospective study, 2 prospective studies, 1 report and 1 quasi-experimental study. COPD was the subject of 13 publications, including 7 cross-sectional studies, 3 reviews, one validation study, one experimental study and one quasi-experimental study. Smoking was studied in 13 publications. There were 4 studies of influenza, 4 on immunisation, and two on lung cancer.
Publications by subject and method in primary care respiratory disease research in Portugal, 2005–2015.
| Asthma and allergic rhinitis | Chronic obstructive pulmonary disease | Smoking | Influenza | Other respiratory infections | Immunisation | Lung cancer | |
|---|---|---|---|---|---|---|---|
| Retrospective | 1 | 1 | 1 | 1 | |||
| Cross sectional | 15 | 7 | 10 | 4 | 1 | 2 | |
| Prospective | 2 | ||||||
| Quasi-experimental | 1 | 1 | |||||
| Review | 3 | 3 | 2 | 2 | 1 | ||
| Validation | 3 | 1 | 1 | ||||
| Case report | 1 | 1 | |||||
| Technical report | 1 | ||||||
| Total | 25 | 12 | 13 | 4 | 5 | 4 | 2 |
Most published studies of respiratory research from primary care in Portugal are observational, using questionnaires or conducted by consulting clinical records. Despite their biases, they are useful in planning health care, because they help determine the prevalence of different risk factors in the population.
One experimental study3 and one quasi-experimental study4 were found among the 63 studies identified. There are fewer experimental studies in Primary Care because of the difficulties in controlling variables related to the phenomenon under study.
Few longitudinal or cohort studies were identified, although a characteristic of Primary Care is continuous follow-up of patients throughout their lives. Investment in this type of study may provide data on the evolution of RD in Portugal.
Asthma was the subject most often studied. Studies focused on prevalence, characterisation of patients, quality of life, and control of the disease. Some studies suggest that there is under-diagnosis of asthma in the Portuguese population. Improvements in diagnostic methods are required along with dissemination of diagnostic criteria among health professionals so that effective treatment can be implemented to control the disease and to improve quality of life. Simple tools like the CARAT questionnaire can assess control of allergic rhinitis and asthma. Further research in primary care may demonstrate its efficacy and effectiveness.
Smoking was addressed in 13 publications. Despite the implementation of anti-smoking laws, campaigns to prevent smoking, and the reduction in smoking that has occurred over the last decades, Portugal still has a high consumption of tobacco. The data obtained in recent research suggest the need to strengthen the anti-smoking law. There is a need as well for greater effectiveness in preventive measures, particularly among adolescents and young women. Education and prevention of smoking among medical students and other health professionals are required to enhance their efforts in smoking cessation among their patients.
Prevalence studies of COPD indicate probable under-diagnosis in clinical practice. Quality of life among COPD patients was also studied. Anxiety and depression are prevalent in these patients, regardless of the stage of COPD. Attention to mental health can promote psychological improvement among these patients.
It is hoped that this study will contribute to improvement in clinical practice. The map of studies published in the last ten years can contribute to the development of new research questions and methodological designs appropriate for Portugal.
FundingFinancial support for this work was provided by FEDER funds through the Operational Programme Competitiveness Factors—COMPETE and National Funds through FCT—Foundation for Science and Technology under the project POCI-01-0145-FEDER-007038, and by the project NORTE-01-0145-FEDER-000013, supported by Norte Portugal Regional Operational Programme (NORTE 2020), under the PORTUGAL 2020 Partnership Agreement, through the European Regional Development Fund (ERDF).
Author contributionsPMT designed the study, contributed to the data collection, performed the data analysis and wrote parts of the methods, results and discussion. BM designed the study, collected the data, contributed to the interpreted results and drafted the manuscript. LA contributed to study design and reviewed the manuscript. JY contributed to the study design and to writing and reviewing the final report. JCS conceived the idea for the study, contributed to the study design, contributed to the interpretation of results and reviewed the manuscript. All authors read and approved the final version of the manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thank the secretariat of the Associação Portuguesa de Medicina Geral e Familiar for access to proceedings of scientific meetings.
- Home
- All contents
- About the journal
- Metrics
- Open access