Cavernous hemangiomas of the mediastinum (CHM) are widely recognized as a rare congenital vascular-related tumor and are pathologically formed from variable-sized masses by dilated cavernous sinuses.1 They have an incidence rate of less than 0.5 % of all diagnosed mediastinal neoplasms.2 There are no previous reports of a CHM case with a concurrent primary lung carcinoma.
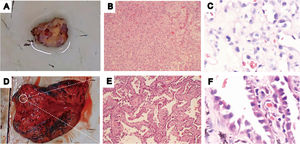
Here, we reported an unusual CHM with an associated primary lung carcinoma and a unilateral pleural effusion. A 59-year-old female, presented to our outpatient clinic with complaints of progressive cough. Chest-enhanced computed tomography (CT) showed a ground-glass nodule in the right upper lobe, as well as a heterogeneous high-density mass in the posterior mediastinum and a small right pleural effusion. One month later, the patient was admitted with mild wheezing. Chest magnetic resonance imaging (MRI) revealed a posterior mediastinal mass with low signal on T1WI, high signal on T2WI, and significantly high diffusion-weighted magnetic resonance imaging (DWI) signal. The previously identified right-sided pleural effusion increased at the time of admission. The patient underwent a right upper lobectomy and resection of the posterior mediastinal mass. Postoperative pathology diagnosed lung adenocarcinoma in the apical segment of the right lung (Fig. 1. D-F), while the size of posterior mediastinal mass was 3 cm × 2.2 cm × 1.5 cm, with a grey-brown surface and an encapsulated spongy dark red solid component (Fig. 1. A). Light microscopic examination of the posterior mediastinal mass demonstrated numerous ectatic vascular sinusoids filled with red blood cells and lined with endothelium. These vascular sinusoids were heterogeneously distributed throughout the spongy tissue. In addition, peripheral lymphoid hyperplasia was observed (Fig. 1. B-C). Immunohistochemistry revealed CD34 (+), CD31 (+), S100 (-), SMA (+), and Ki67 (+ > 1%). A final diagnosis of CHM with concurrent lung adenocarcinoma T1cN0M0, stage IA, was made. The patient was discharged seven days postoperatively, with no evidence of recurrence at a 22-month follow-up visit.
Macroscopic photograph demonstrating (A) a soft irregular mass consisting of a grey-brown surface and an encapsulated spongy solid with an abundance of blood vessels (D), and a white nodule in the apical segment of the right lung; (B) Medium-powered microscopic view revealing a tumor composed of ectatic vascular sinusoids and lymphoid aggregates. Blood clots can also be seen in dilated vascular lumens (Hematoxylin and eosin stain, 100 x); (C) High-powered microscopic view revealing endothelial cells lining red blood cell-containing vascular lumens. The blood vessels are rich and the lumens are variable in size (Hematoxylin and Eosin stain, 400 x); (E) Medium-powered microscopic view showing a large population of heterogeneous tumor cells arranged in nested/papillary patterns, consistent with an invasive adenocarcinoma (Hematoxylin and Eosin stain, 100 x); (F) High-powered microscopic view revealing mostly adherent adenocarcinoma tumor cells (Hematoxylin and eosin stain, 400 x).
In conclusion, CHM should be taken into consideration if a patient presents with a mediastinal lesion which shows angioma-like enhancement on contrast-enhanced CT scan, or high signal on T2WI and DWI. CHMs may complicate with unilateral pleural effusions. The presence of coexisting intrapulmonary lesions, particularly lung cancers, needs to be investigated in these patients.
Ethics approvalThe study was conducted according to the Declaration of Helsinki and Good Clinical Practice. The study was approved by Tianjin Chest Hospital Ethics Committee.
Ethical considerationsWritten informed consent was obtained from the patient for publication of the article.
Consent for publicationNot applicable
Availability of data and materialsAll data generated or analyzed during the study are included in the published article.
FundingThis study was supported by Tianjin Medical and Health Science and Technique Project, China (KJ20224), Tianjin Key Medical Discipline (Specialty) Construction Project, China (TJYXZDXK-049A), and Tianjin Chest Hospital Fund, China (2018XKZ32).
Authors’ contributionsL.Y., J.L., and J.W. participated in the design of the study. J.L., and J.W. analyzed imaging data. L.Y. wrote the manuscript. All authors read and approved the final manuscript.
Not applicable.