The introduction of endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) and endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) has been a major advance in the diagnosis and staging of lung cancer, as well as in the study of other mediastinal lesions.1 Although they are safe techniques, complications have occurred, including pneumothorax, hemorrhage, infection, mediastinitis and mediastinal abscess, with a 50% mortality rate with the last two.2 We present two cases of mediastinitis that we have experienced recently in our hospital following these endoscopic examinations.
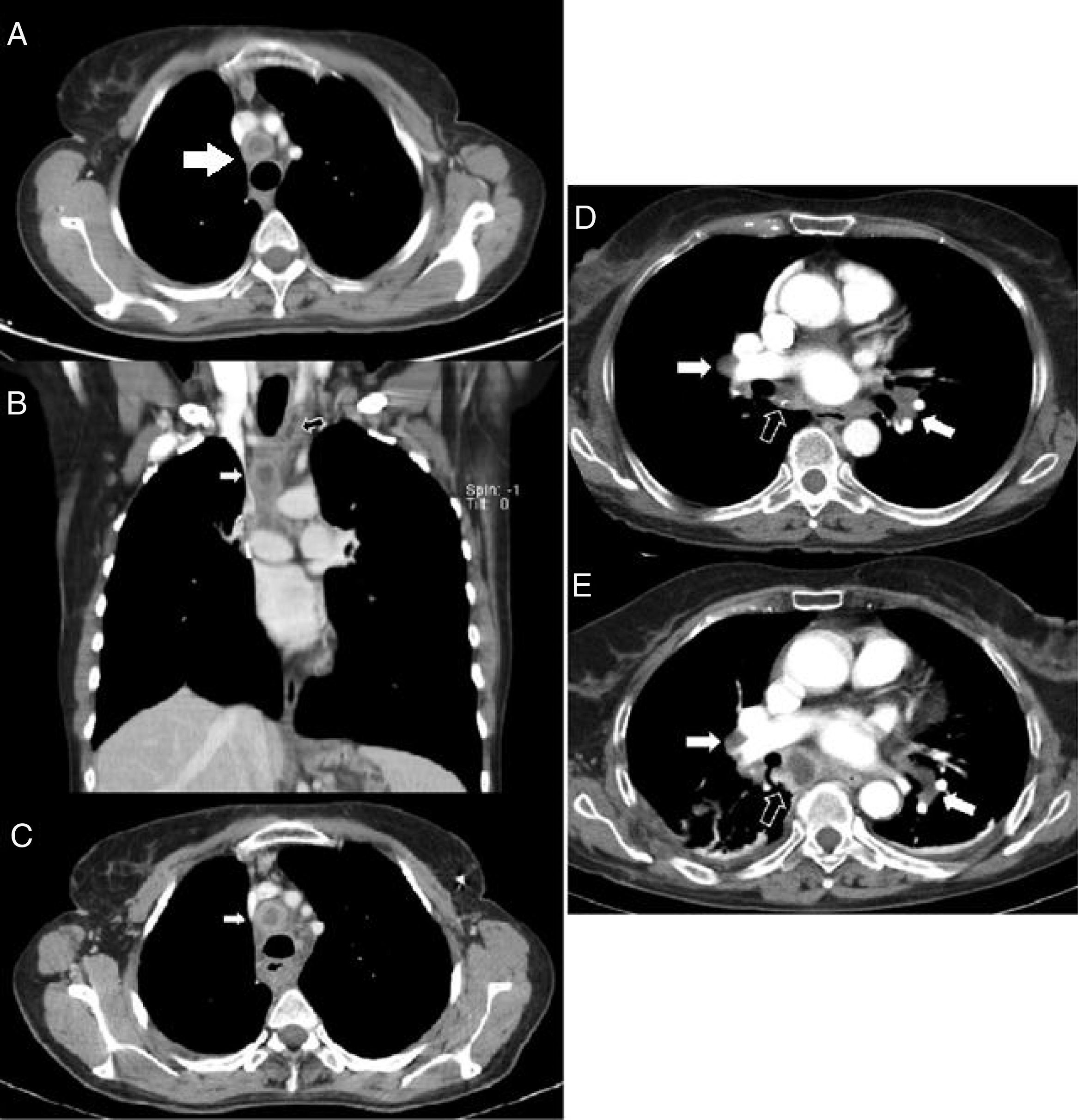
A 42-year-old woman diagnosed with a grade 3 breast infiltrating ductal carcinoma (stage cT2N+), was initially treated with neoadjuvant chemotherapy, left mastectomy, and monthly trastuzumab. Recurrence was confirmed through biopsy of a solitary pulmonary nodule. Later on, a chest CT revealed a well-delimited and necrotic pretracheal mediastinal adenopathy (2R) (Fig. 1A), which was biopsied by EBUS-TBNA under sedation (midazolam, 6mg; Olympus needle, 21-gauge) and a total of 4 passes, without complications. Malignancy was confirmed. After 48h, she started feeling general malaise, retrosternal pain radiating to the neck, odynophagia, dysphagia, fever, and erythematous, and pruriginous maculo-papular lesions in the trunk and upper limbs. In blood analysis, we noticed a significant presence of leukocytosis and elevation of C-reactive protein. Chest CT showed increased attenuation of mediastinal fat, well-defined wall collections in the left upper and lower paratracheal space (Fig. 1B and C). Treatment response with ceftriaxone and clindamycin was good and did not require surgical debridement. Blood cultures and punctured adenopathy were negative. The evolution was favorable and after 11 days she was discharged, continuing treatment at home.
(A) Computed tomography image with contrast showing a pretracheal retrocaval mediastinal adenopathy with well-delimited necrotic center (white arrow). (B) and (C) Computed tomography images with contrast in coronal and axial planes showing mediastinal collections at left paratracheal (black arrow) and necrotic 2R adenopathy (white arrows) with thick wall enhancing. (D) Computed contrast tomography image showing small hilar (white arrows) and subcarinal (black arrows) adenopathies with punctate calcifications. (E) Contrast computed tomography image several days after EBUS, showing subcarinal liquid collection with peripheral enhancement (arrows).
A 74-year-old woman was monitored in Pulmonology Clinic for presenting mediastinal lymphadenopathy (Fig. 1D). EUS-FNA (Cook needle, 22-gauge) was performed with a total of 4 passes (subcarinal adenopathy, 7), with no immediate complications. Tuberculosis was confirmed in anatomopathological samples. The next day she started having retrosternal pain not associated with any other symptomatology. After two weeks, she went to Emergency because of persistent pain and fever. As she was hemodynamically unstable she was admitted to the Intensive Care Unit. Blood tests revealed leukocytosis and hyperfibrinogenemia. The chest CT showed three well-defined liquid collections of adjacent fat (Fig. 1E). Right-assisted videothoracoscopic surgery drained the collections and a mediastinal lavage was performed. Cultures of the purulent material obtained during surgery were positive for Streptococcus spp, Pasteurella multocida and Peptostreptococcus. Antibiotic treatment was completed with ceftriaxone, vancomycin and clindamycin with positive effect. After a month of admission, she was discharged without further complications.
EBUS-TBNA and EUS-FNA are minimally invasive, cost-effective techniques for diagnosis and mediastinal staging of lung cancer.3 They have also been shown to be useful for the diagnosis of benign neoplastic disease and granulomatous diseases with mediastinal involvement.4 Although these are safe techniques, their rapid diffusion into daily clinical practice has led to the recording and publication of their adverse effects, some of them being serious. Hemoptysis, followed by infections, is the most frequent complication. However, the incidence of mediastinitis is still unknown. The hypothesis about the relationship between bronchoscopy and infections lies in the contamination of the endoscope's working channel through the nasopharyngeal region. The passage of the puncture needle through this channel causes the tissue to be contaminated and infected. Other risk factors are necrotic and cystic lesions due to their avascularity (anecdotal appearance with ultrasound) that allows the growth of bacteria without being recognized by the immune system, and, in the case of sarcoidosis, due to deterioration of the immune response in the sarcoid lymph nodes. None of these injuries should be punctured.
In order to prevent mediastinal infections, different measures have been proposed, such as the proper disinfection of the material, the careful performance of the procedure according to regulation recommendations,5 preferably carried out on intubated patients (avoiding oropharyngeal contamination, although this also has its drawbacks like deep sedation or general anesthesia, the need for an anesthesiologist in the bronchoscopy room and more prolonged procedures) and the use of prophylactic antibiotics (oral or intravenous). At present, there is a lack of evidence about when to recommend the use of prophylactic antibiotics and how to administer them,6 although some authors have considered their use in the case of cystic lymphadenopathy or necrotic areas in immunocompromised patients at high risk of developing local infections,7 or in patients with sarcoidosis. More studies are needed to investigate which situations may influence the development of infections and to see the role of prophylactic antibiotics in these cases.
In conclusion, although EBUS-TBNA and EUS-FNA are safe techniques for diagnosis and mediastinal staging, they are not exempt from complications, including mediastinitis. It is essential to follow scrupulously the recommendations of the regulations to avoid contamination of the endoscope's channel and its subsequent spread to lymphadenopathy through the needle puncture. More studies are needed to identify the role of prophylactic antibiotics in patients who are at increased risk of developing these infections.
Author's contributionTara Pereiro: Author. Conception and design. Final approval of the manuscript.
Antonio Golpe: Co-author. Final approval of the manuscript.
Anxo Martínez de Alegría: Co-author. Final approval of the manuscript.
Luis Valdés: Author. Conception and design. Final approval of the manuscript.
FundingThe authors declare the non-existence of external financing of this article.
Conflicts of interestThe authors have no conflicts of interest to declare.