Pulmonary tumour thrombotic microangiopathy (PTTM) is a very rare cancer-related pulmonary complication, histologically characterised by fibrocellular subintimal proliferation of small pulmonary arteries and arterioles in patients with metastatic carcinoma and associated with the development of thrombotic microangiopathy (TMA), respiratory failure and cor pulmonale,1 and it is a known cause of severe pulmonary hypertension.2 TMA is a disorder characterised by thrombocytopenia, microangiopathic haemolytic anaemia with negative Coombs test, and variable degrees of organ dysfunction.1
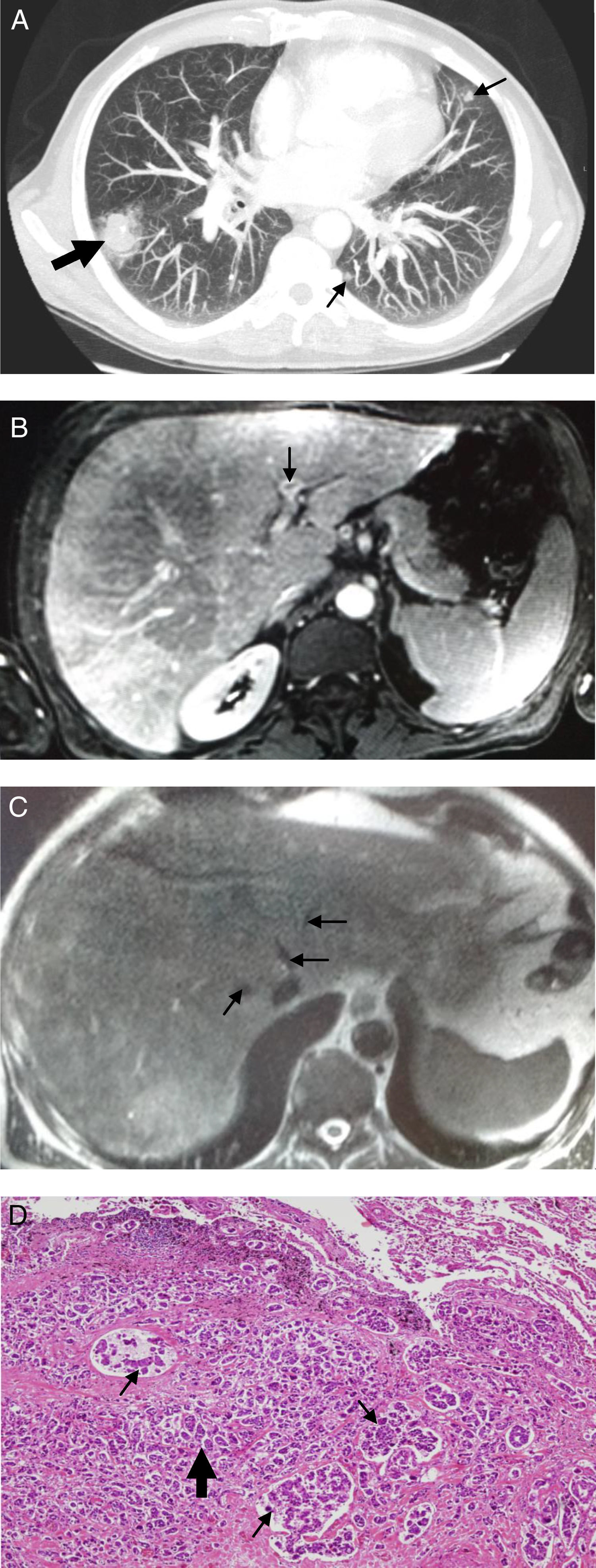
We present the case of a 60-year-old male who had been diagnosed four years previously with carcinoma of larynx treated with surgery and radiotherapy, without evidence of relapse, and who was admitted for dyspnoea, orthopnea, dysphonia and haemoptoic sputum with two weeks of evolution. The physical examination showed the patient to be tachypneic, with a yellowish or icteric hue of the skin and signs of right-sided heart failure. The following were the most relevant complementary examinations. Blood test: platelets 99×103μL−1; total bilirubin 3.4mg/dL (as opposed to direct bilirubin, 2mg/dL); GOT 241UI/L; GPT 73UI/L; GGT 787UI/L; alkaline phosphatase 802UI/L; ferritin 1457ng/mL and N-terminal brain natriuretic propeptide 2155pg/mL. Peripheral blood smear: 7% of schistocytes with negative direct Coombs test, PaO2 49.8mmHg. Radiology and chest computed tomography (CT) angiography showed a pulmonary nodule with ground glass halo and a small calcification and several peripheral ground glass nodular lesions, and hepatomegaly with faint, hypodense, ill-defined, subcentimetre hepatic nodules. There was no evidence of defects in repletion at the level of the pulmonary trunk, principal, lobar and segmental arteries (Fig. 1A). Abdominal echography: hepatomegaly was suggestive of chronic hepatopathy and splenomegaly. Echocardiography: right-sided chamber dilatation with septal displacement, tricuspid insufficiency and severe pulmonary hypertension with preserved left ventricular ejection fraction. Right heart catheterisation: pulmonary arterial pressure 87/22/40mmHg; pulmonary capillary wedge pressure 5mmHg; cardiac output 7.7l/min; cardiac index 3.94l/min/m2; pulmonary vascular resistance 363dyn/sec/cm5. Positron emission tomography: increased uptake at a pulmonary, mediastinal, hepatic and bone level, suggestive of malignancy. Hepatic magnetic resonance with contrast: thrombosis of the left branch of the portal vein, suprahepatic veins threadlike but permeable (Fig. 1B and C).
(A) Projection of maximum intensity in the computed tomography of the thorax. It shows a pulmonary nodule with ground glass halo and a small calcification (thick arrow) and several peripheral ground glass nodular lesions (thin arrows). (B) Thrombosis of the left portal vein on magnetic resonance imaging of the liver (sequence T1 with Gadolinium), (C) Narrow, but permeable, suprahepatic veins on magnetic resonance imaging of the liver (FSE T2WI sequence), (D) Micropapillary pattern lung adenocarcinoma (thick arrow) with marked vascular invasion (thin arrows). HE4× (haematoxylin eosin).
These data pointed to atypical thrombotic microangiopathy probably secondary to a neoplastic process of pulmonary origin which advanced with pulmonary hypertension. On subsequent days, the patient's clinical deterioration intensified and he presented with anasarca, increased dyspnoea, signs of hepatic encephalopathy, increased anaemia (which required transfusion of red blood cells and fresh-frozen plasma) and severe liver damage. The patient died some days later. The necropsy showed the existence of adenocarcinoma in the right lung, with massive pulmonary vascular embolisation which affected both lungs, mediastinal lymph nodes, heart, both suprarenal (adrenal) glands and liver, with hypertrophy and dilatation of the right cardiac cavities, subendocardial ischaemia, congestive hepatosplenomegaly, bilateral pleural effusion and ascites (Fig. 1D). The cause of death was multiorgan failure related to PTTM.
Diagnosis of PTTM during life is extremely rare.3 Adenocarcinoma of the stomach is the condition most frequently associated with PTTM (52.4% of all described cases), followed by those of the lung (14.3%), breast (9.6%), and a few rarely-reported tumour sites.1 Disease course tends to be rapidly progressive and may cause pulmonary hypertension, right ventricular pressure-overload and cor pulmonale,4 or organ dysfunction. In many cases, the presence of TMA is the predominant finding in the clinical scenario and differential diagnosis with thrombotic thrombocytopenic purpura must be made5 to avoid initiation of ineffective therapeutic measures, such as plasmapheresis, which would delay diagnosis and might, even, favour microthrombotic formation.2,6 Diagnosis during life of this disease has only been achieved in 10 patients on the basis of: transbronchial biopsy (5 cases); video-assisted thoracic surgery (2); CT-guided lung biopsy (1); and pulmonary microvascular cytology using a wedged pulmonary catheter (2).7
If diagnosis can be established during life, it should be followed by starting early treatment. Of the only four patients to survive beyond the initial acute phase, one was treated with warfarin, dexamethasone, acetylsalicylic acid and chemotherapy based on fluoropyrimidine (gastric adenocarcinoma).7 While the other three patients showed improvement in their pulmonary hypertension after administration of Imatinib, all died due to disease progression.3 Imatinib is an inhibitor of the vascular endothelial growth factor receptor implicated in the pathogenesis of PTTM, which is used in this disease because it has been shown capable of reducing such blood receptor levels.
In brief, in cases of severe, rapidly progressive pulmonary hypertension, differential diagnosis should include PTTM secondary to a neoplasm, particularly if accompanied by haematological alterations that suggest TMA. Although our case was one of pulmonary adenocarcinoma, the most frequent clinical profile is that where the tumours are gastric in origin. In the course of patient's clinical disease, early diagnosis is crucial to enable treatment to be initiated as quickly as possible, since, failing this, prognosis is generally fatal.
Authors’ contributionsRA, MET and LV were responsible for the conception and design of the study, and wrote and edited the manuscript. JMAD contributed to the drafting and revision of the manuscript. All authors read and approved the final manuscript.
FundingThis work was performed without funding.
Conflicts of interestThe authors have no conflicts of interest to declare.