Multifocal Micronodular Pneumocyte Hyperplasia (MMPH) corresponds to the proliferation of type II pneumocytes, which is almost exclusive to tuberous sclerosis complex (TSC) and/or lymphangioleiomyomatosis (LAM).1 The authors report on an uncommon case of MMPH in a patient with TSC, without LAM.
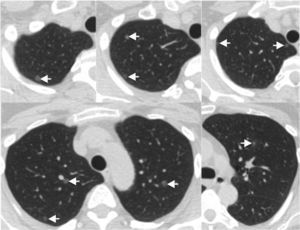
We present a case of a 48-year-old female, with previous history of seizures and TSC diagnosed 18 years earlier, based on the presence of skin lesions (facial angiofibromas) and cortical tubers on brain MR. Investigation of her family revealed that 6 relatives have the same condition. She is a non-smoker and has had no relevant occupational exposure. The patient presented asymptomatic, namely without respiratory complaints. The pulmonary function tests were normal: FEV1 2.91L (104% of predicted); FVC 3.6L (110% of predicted); DLCO 81%. Abdominal CT were performed to assess renal angiomyolipomas; the lower parts of the lungs showed pulmonary nodules that were followed up with a chest CT. The chest CT revealed multiple ground-glass nodules scattered through both lungs, the largest one was 8mm (Fig. 1). There were no cystic lesions suggestive of LAM. After 2 years of follow-up the nodules remained stable in size and number, compatible with a MMPH diagnosis.
Tuberous sclerosis complex is an autosomal dominant disease, which commonly affects various organs, typically the brain, skin, kidneys, heart and lungs. LAM is the most common pulmonary manifestation of TSC, with a reported prevalence 1–3% of the TSC patients, however it could be much higher (up to 35%) in women with TSC.2
MMPH, despite being considered rare, is the second most common cause of lung involvement by TSC. This disorder consists of multicentric, well-demarcated nodular proliferation of type II pneumocytes along alveolar septa, and has been reported in men and women with TSC (with or without LAM manifestation) and in women with sporadic LAM, with only 3 cases described without this association.3 Clinically, MMPH might be associated with cough, dyspnea and moderate or asymptomatic hypoxemia.2 Unlike LAM, treatment is generally not needed in MMPH, because it seems to be indolent and not progressive, moreover it has not been proven to have malignant potential.4 On HRCT MMPH is characterized by multiple solid or ground-glass nodules, ranging from 2 to 10mm, scattered through the lungs in a random distribution. The main radiological differential diagnosis includes atypical adenomatous hyperplasia, early Langerhans histiocytosis, hematogenous metastases and miliary tuberculosis. The differentiation between MMPH and these entities may be very difficult, however the history of TSC, the multiplicity and random distribution of the nodules, as well the stability of number and size of these lesions in the follow-up examinations, helps to provide the diagnosis MMPH.
To the best of our knowledge there are no established guidelines for management of MMPH in TSC. Taking into account the benign nature of this entity, we think that is reasonable to assume the diagnosis MMPH in this case, leaving histopathologic sampling as an option if there are suspicious lesions, nodule progression in dimension or number; or if the patient decides to follow this approach.4 However, a long-term follow-up is advised to document the stability the nodules to corroborate this diagnosis.
Conflict of interestsThe authors have no conflicts of interest to declare.