We conducted this prospective study to expand available information in relation to serum phosphate levels in treatment of acute asthma. A β-adrenergic agonist, salbutamol, was used for this purpose.
Material and methodsTwenty-six patients who met the inclusion criteria as; age over 16 years, asthma history, and an acute exacerbation were included. Serum blood urea nitrogen, creatinine, glucose were within normal limits in all the patients. None of the patients were on chronic theophylline therapy. Baseline serum phosphate and potassium levels were measured. Nebulized salbutamol (2.5mg) was used three times at every hour. After 60min, serum phosphate and potassium levels were measured.
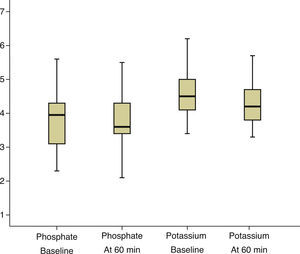
ResultsSerum phosphate levels decreased from 3.7±0.9mg/dL (baseline) to 3.6±0.9mg/dL at 60min. This decrease was not statistically significant (p=0.373). Serum potassium levels decreased significantly (p<0.001) from 4.6±0.7mmol/L (baseline) to 4.3±0.7mmol/L (60min).
ConclusionAdministration of nebulized salbutamol during the emergency treatment of acute exacerbation of asthma is not associated with a statistical decrease in serum phosphate. There was significant hypokalemia. This study indicates that a further study is needed to elucidate the clinical significance of nebulized salbutamol on serum phosphate.
Levámos a cabo este estudo prospetivo para ampliar a informação disponível relativamente aos níveis de fosfato sérico no tratamento de asma aguda. Foi utilizado um agonista β-adrenérgico, salbutamol, para este efeito.
Materiais e métodosForam incluídos 26 doentes que cumpriam os critérios de inclusão de: idade superior a 16 anos, história de asma, incluindo uma exacerbação aguda. A ureia do soro sanguíneo, creatinina e glucose estavam nos limites normais em todos os doentes. Nenhum dos doentes era submetido a terapia crónica de teofilina. Os níveis da base de referência de fosfato e potássio sérico foram medidos. O nebulizador de salbutamol (2,5mg) era usado 3 vezes por hora. Após 60 min, os níveis da base de referência de fosfato e potássio sérico eram medidos.
ResultadosOs níveis de fosfato sérico diminuíram de 3,7±0,9mg/dL (base de referência) para 3,6±0,9mg/dL aos 60 min. Esta redução não era estatisticamente significativa (p=0,373). Os níveis de potássio sérico diminuíram significativamente (p<0,001) de 4,6±0,7mmol/L (base de referência) para 4,3±0,7mmol/L aos 60 min.
ConclusãoA administração de salbutamol nebulizado durante o tratamento de urgência de uma exacerbação aguda de asma não está associada a uma diminuição estatística do fosfato sérico. Ocorreu uma hipocalemia significativa. Este estudo indica que é necessário um estudo adicional para esclarecer o significado clínico do salbutamol nebulizado no fosfato sérico.
Asphyxia is responsible for the majority of deaths in patients with acute asthmatic crisis, and the adverse effects of medical treatments are also important in terms of the deaths.1 Nebulized β-adrenergic agonists are the mainstay of treatment for acute exacerbation of asthma in the emergency setting.2 β-Adrenergic agonists (BAA) have side effects such as tremor, palpitations, tachycardia, and anxiety.3 There are several studies that demonstrate a statistically significant decrease in serum potassium and magnesium after BAA administration.4–7 In addition, there are also some studies regarding the BAA induced hypophosphatemia.8–11 In the current research, our aim is to investigate Serum Potassium and Phosphate Levels at the 60min after administration of Nebulized Salbutamol for Asthma.
Materials and methodsThis prospective study is conducted in patients with asthmatic attack in the emergency department. Patients were treated with a BAA-salbutamol – according to a study protocol that was approved by the local ethical committee. Informed consent was obtained from all the patients. Baseline data including age, sex, clinical history, and the medications used were recorded. All patients included in the study met the criteria as: age >16 years, a history of acute exacerbation of asthma (dyspnea, cough and, on examination, wheezing). Patients with respiratory failure, altered mental status, renal failure, diabetes mellitus, and cirrhosis were excluded. Patients using alcohol, diuretics, theophylline, aminophylline, antidiabetic, and antihypertensive drugs were also excluded. The samples had BAA at least four hours before the admission. The severity of the exacerbation determines the treatment modality. Indices of severity including particularly PEF, pulse rate, respiratory rate, and pulse oximetry, had to be monitored during treatment. The exacerbation severity was defined according to the Global Strategy for Asthma Management and Prevention 2011.12
All the patients were monitorized by continuous electrocardiograhy, and arterial oxygen saturation by pulse oximetry with a finger oximeter. The baseline peak expiratory flow rate was measured. An intraveneous (i.v.) line for repeated blood sampling was established and baseline laboratory assay which included serum phosphate, creatinine, blood urea nitrogen, glucose, potassium levels was performed. Patients were given initial nebulized treatment of salbutamol (2.5mg).
Nebulized salbutamol (2.5mg) was used three times during the first hour. After the third administration of salbutamol, serum phosphate and potassium levels were assessed.
None of the patient received magnesium, potassium, phosphate, corticosteroids, theophylline, and i.v. dextrose or saline during the study period.
The mean and standard deviation were calculated for baseline and subsequent measure of phosphate and potassium. Paired-t test was used for analyzing the changes in case of phosphate and potassium levels. p-Value <0.05 was considered statistically significant.
ResultsTwenty-six patients were enrolled during the study period. The mean patient age was 58.8±10.3 years (range 35–74 years), with 11 female and 15 male asthmatic patients. All the patients had moderate asthmatic attack. The protocol included the usage of oxygen if arterial oxygen saturation (Sao2) decreased to less than 92%. However, during the study, all patients had Sao2 values above 92%. There was no change in ECG monitorization related to hypokalemia in the patients. In the emergency department, all patients received three doses of nebulized salbutamol therapy (2.5mg, every 20min). Theophylline and corticosteroids were not administered in the emergency department during the study. Neither intraveneous dextrose nor saline solution was used during the study period.
There was an average duration of symptoms of 30±35h (range 2–55) before seeking medical attention. Mean baseline peak expiratory flow rate averaged 210±110L/min (range 100–320L/min).
Although serum phosphate levels decreased from a mean of 3.7±0.9mg/dL at baseline to 3.6±0.9mg/dL at 60min, no significant decrease was found (Fig. 1).
Serum potassium levels decreased significantly from 4.6±0.7 (baseline) to 4.3±0.7mmol/L (60min) (p<.001) (Fig. 1).
DiscussionThe aim of this study was to add more data to the information concerning the serum phosphate and potassium changes during intensive treatment of acute asthma with salbutamol.
In this study, salbutamol use was accompanied by a significant decrease in serum potassium levels. Our observation regarding BAA related hypokalemia is consistent with most of the previous studies.4–7 The principal action of BAA is to stimulate the BAA that are associated with the membrane-bound sodium-potassium ATPase. Activation of this enzyme results in a direct potassium influx into cells.
In this report, salbutamol was given according to the standard emergency medical protocols, and it was not accompanied by significant decrease in serum phosphate. Serum phosphate levels decreased from a mean of 3.7±0.9mg/dL at baseline to 3.6±0.9mg/dL at 60min. No significant correlation was found. This result is not consistent with previous studies.
There are some differences between our study and previous studies. Firstly, we administered only a BAA-salbutamol. We did not use i.v. fluids, theophylline, and corticosteroids which may have an effect on serum phosphate levels.
Secondly, our patients were not receiving theophylline, diuretics, antihypertensive, and antidiabetics before they arrived at the emergency department.
In one study BAA induced hypophosphatemia, but BAA and other bronchodilator drugs were used together.8
In a different study, BAA decreased serum phosphate, besides albuterol, other bronchodilator agents such as theophylline, atropin, corticosteroids, and i.v. fluids were administered.11
In another study, it is reported that hypophosphatemia induced by albuterol is due to the parenteral albuterol administration.13
In Massara et al's study, i.v. infusion of salbutamol caused hypophosphatemia.10
In the current study, we used only nebulized salbutamol. Other drugs that may affect serum phosphate levels such as theophylline, corticosteroids and IV fluids were not used. Therefore, this preliminary report indicates that a further study aimed at elucidating the clinical effect of nebulized salbutamol on serum phosphate is required.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.