Pneumocystis pneumonia (PCP) is caused by the fungus Pneumocystis jirovecii, and its incidence has been on the rise in immunosuppressed patients without HIV.
We performed a cross sectional study in patients with PCP and assessed demographic, clinical presentation and outcome measures such as mechanical ventilation and mortality differences between HIV and non-HIV patients.
The two groups were statistically significantly different, with the HIV group being younger (45.5 years vs 55.9 years, p-value 0.001) and mostly composed of male patients (69% vs 31%, p-value <0.001). Also, the HIV patients had higher percentage of respiratory complaints (90% vs 68%, p-value 0.02) and lactate dehydrogenase elevation (73% vs 40%, p-value 0.001). In contrast, non-HIV patients had worse outcomes with higher incidence of invasive mechanical ventilation (23% vs 46%, p-value 0.005) and in-hospital mortality (13% vs 37%, p-value 0.002).
These results reflect the literature and should raise awareness to a potentially fatal medical situation of increasing incidence.
Pneumocystis pneumonia (PCP) is a respiratory invasive infection caused by Pneumocystis jirovecii, an ubiquitous fungus.1 It is transmitted by air and mostly infects immunocompromised patients.1 PCP is characterized by respiratory complaints of cough, dyspnea, but also tachycardia, low grade fever and hypoxemia.1,2 Analytically, elevated levels of lactate dehydrogenase (LDH) are very suggestive, and in terms of radiographic findings there is a broad range from diffuse infiltrate to nodules, cysts and pneumothorax.1,2 Diagnosis is made by detection by RT-PCR of the fungus in bronchoalveolar lavage (BAL) material.2 Treatment is usually with trimethoprim/sulfamethoxazole (TMP/SMX), but other options are available.2,3 When there is important hypoxemia (PaO2≤70mmHg), adjuvant corticosteroids may be added.2,3
Immunosuppression other than HIV can be drug related, due to lymph and myeloproliferative disorders, solid tumors, autoimmune diseases, solid organ and hematologic transplant, primary immunodeficiency and severe malnutrition.4 It has been shown that these patients are at increasing risk for PCP, and usually the clinical presentation is abrupt with fast evolution to respiratory failure and higher mortality (30–60% versus 10–20% in HIV patients).2,4 Treatment is the same, but despite prophylaxis being well established for HIV patients (with lower doses to TMP/SMX), there is still no consensus for other immunosuppressed patients.3,4
The main goal is to assess the differences between HIV and non-HIV patients with PCP.
MethodsCross sectional retrospective study by chart review of patients with pneumocystis pneumonia admitted to a single tertiary-care center between 2011 and 2016.
Permission was obtained to review data retrospectively on the basis of medical record review from the Centro Hospitalar Universitário de Lisboa Central Institutional Review Board.
Eligible patients were 18 years or older and identified using an ICD-9 code for pneumocystis pneumonia.
The electronic medical record for each eligible patient was reviewed to obtain demographic data, length of stay, HIV infection and its status, and risk factors for PCP. PCP was characterized by clinical (respiratory complaints any, fever – axillary temperature over 37.5°C), analytical (hypoxemia in blood gas analysis with PaO2<80mmHg, leucocytes values higher than 11×109/L and below 4.5×109/L, lactate dehydrogenase (LDH) >220U/L and C-reactive protein (CRP) >5mg/mL), and radiological features (any of the PCP radiological presentations was considered), defined as dichotomous variables (presence/absence), as well as definitive versus probable diagnosis. Outcomes were in-hospital mortality, corticotherapy use and need for either invasive or non-invasive mechanical ventilation.
Data was analyzed with mean and standard deviation (SD) if normally distributed and with median and Interquartile range (IQR), if non-normally distributed. Student t-test was performed for continuous variables, and chi square test for dichotomous variables. Multivariate logistic regression was done to account for confounding. To avoid model overfitting, the rule of ten was observed. A p value of <0.05 was considered to be significant. Analysis was conducted in Stata (StataCorp. Stata statistical software: release 14. College Station, TX: StataCorp LP).
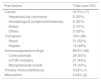
ResultsA total of 129 patients were included – 75 with HIV diagnosis and 54 with immunosuppression other than HIV (Table 1). Between these 2 groups there was a significant difference in demographic data mainly age (45.5 years vs 55.9 years, p-value 0.001) and gender (preponderance of male sex – 69% vs 31%, p-value <0.001). There was no difference between HIV and non-HIV in length of stay (overall mean 28.3 days ± 20.8).
Demographic characteristics of both HIV and non-HIV groups: total of 129 patients (75 with HIV diagnosis and 54 with immunosuppression other than HIV). There was a significant difference in age (45.5 years vs 55.9 years, p-value 0.001) and gender (preponderance of male sex – 69% vs 31%, p-value <0.001).
| Demographics | HIV | Non-HIV | Total | p-Value |
|---|---|---|---|---|
| Age | 45.5 (11.5) | 55.9 (13.7) | 49.8 (13.4) | 0.001 |
| Gender (male) | 69.1% (56) | 30.9% (25) | 62.8% (81) | <0.001 |
| Length of stay | 27.8 (22.6) | 29.1 (18.2) | 28.3 (20.8) | 0.7 |
| Total | 75 | 54 | 129 |
Regarding the HIV group, only 12.5% (7) had virological suppression and none had immunological response. CD4 cell count mean was 57 (0–458), with 92% (59) below 200 cells.
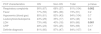
Causes of immunodepression in the non-HIV group were mainly due to drug related immunosuppression (89%) and transplant (74%) (Table 2).
Risk factors for immunosuppression in non-HIV patients: the most frequent was drug related immunosuppression (89%) and transplant (74%), followed by cancer (32%), malnutrition (0.04%) and primary immunodeficiency (0.02%). The most common cancers were hepatocellular carcinoma and hematological (30% each), transplants were about half renal and hepatic. The most used immunosuppressive drugs were corticosteroids (50%) mTOR inhibitors (44%) and mycophenolate mofetil (33%).
| Risk factors | Total (non-HIV) |
|---|---|
| Cancer | 31.5% (17) |
| Hepatocellular carcinoma | 5 (30%) |
| Hematological (lymphoma/leukemia) | 5 (30%) |
| Breast | 2 (10%) |
| Others | 5 (30%) |
| Transplant | 74% (40) |
| Renal | 21 (52%) |
| Hepatic | 19 (48%) |
| Immunosuppressive drugs | 88.9% (48) |
| Corticosteroids | 24 (50%) |
| mTOR inhibitors | 21 (44%) |
| Mycophenolate mofetil | 16 (33%) |
| Primary immunodeficiency | 0.02% (1) |
| Malnutrition | 0.04% (2) |
Clinically there was a statistically significant difference between HIV and non-HIV patients in relation to respiratory complaints (90% vs 68%, p-value 0.02). This difference was still observed after adjusting for potential confounders (p-value 0.04), yielding a 2.2 odds ratio (OR), which means a 2.2 times higher risk in HIV patients. There was also a difference between groups in LDH elevation at diagnosis (73% vs 40%, p-value 0.001), which was still observed after adjusting for confounding, with a 1.7 times higher risk in HIV patients. There was no statistically significant difference between groups in the presence of fever, hypoxemia, white blood count abnormalities and C-reactive protein (Table 3). Definite diagnosis defined by RT-PCR isolation of P. jirovecii in bronchoalveolar lavage (BAL) material was similar in both groups (81% vs 73%, p-value 0.4).
Clinical characteristics of pneumocystosis pneumonia: statistically significant difference between HIV and non-HIV patients in relation to respiratory complaints (90% vs 68%, p-value 0.02) and lactate dehydrogenase (LDH) elevation at diagnosis (73% vs 40%, p-value 0.001). There was no statistically significant difference between groups in the presence of fever, hypoxemia, white blood count abnormalities and C-reactive protein. Definite diagnosis was similar in both groups (81% vs 73%, p-value=0.4).
| PCP characteristics | HIV | Non-HIV | Total | p-Value |
|---|---|---|---|---|
| Respiratory complaints | 90% (67) | 68% (37) | 81% (104) | 0.002 |
| Fever | 77% (55) | 68% (36) | 73% (91) | 0.2 |
| Hypoxemia (blood gas) | 85% (61) | 83% (43) | 84% (104) | 0.7 |
| Leukocytosis/leukopenia | 43% (29) | 35% (17) | 40% (46) | 0.4 |
| LDH | 73% (48) | 40% (18) | 60% (66) | 0.001 |
| CRP | 48% (23) | 53% (25) | 59% (69) | 0.17 |
| Definite diagnosis | 81% (60) | 87% (47) | 84% (107) | 0.4 |
In terms of outcome measures, statistically significant differences were only observed in need for invasive mechanical ventilation (23% vs 46%, p-value 0.005) and in-hospital mortality (13% vs 37%, p-value 0.002). Both these outcomes were still statistically significant following adjustment for confounders (p-values of 0.015 and 0.037 respectively), resulting in a 0.6 and 0.5 times risk for invasive mechanical ventilation and mortality for HIV patients. There was no statistically significant difference in the need for corticotherapy or non-invasive mechanical ventilation (Table 4).
Outcomes differences between HIV and non-HIV: statistically significant differences observed for need for invasive mechanical ventilation (23% vs 46%, p-value 0.005) and in-hospital mortality (13% vs 37%, p-value 0.002). There was no statistically significant difference in the need for corticotherapy or non-invasive mechanical ventilation.
| Outcomes | HIV | Non-HIV | Total | p-Value |
|---|---|---|---|---|
| Corticotherapy | 73% (55) | 73% (37) | 73% (92) | 0.9 |
| Non-invasive mechanical ventilation | 3% (2) | 7% (4) | 5% (6) | 0.2 |
| Invasive mechanical ventilation | 23% (17) | 46% (25) | 33% (42) | 0.005 |
| In-admission mortality | 13% (10) | 37% (20) | 23% (30) | 0.002 |
The results show that the populations suffering from HIV and non-HIV immunosuppression are different in terms of demographics, with HIV patients mostly being younger and of the male gender, which might be related to HIV epidemiology.
The main causes for immunosuppression in our cohort are drug related immunosuppression and transplant, which are obviously related, but also include autoimmune patients undergoing biological immunosuppression. This largely correlates to our hospital setting as a reference center for both solid organ transplant and autoimmune disease patients.
Clinically, HIV patients were more exuberant with higher likelihood of experiencing respiratory complaints and of having a higher LDH level, very relevant for the diagnosis. On the contrary, non-HIV patients were mostly likely to have worse outcomes such as the need for invasive mechanical ventilation and in-hospital mortality. Interestingly, these bad outcomes were not related to accuracy of diagnosis or demographic variables that were so different between the two groups.
The results suggest that the clinical presentation in non-HIV patients is more subtle, but with worse consequences than in HIV patients. This fits in with the published data. It remains to be answered if these two findings are related, and so if the higher mortality and need for invasive mechanical ventilation are a result of a later diagnosis due to an elusive clinical presentation. Therefore, it would be interesting to compare time to diagnosis in the two settings.
This work has some confounders, mainly, that the non-HIV group was not very representative, being composed mostly of patients with solid organ transplants. It would be interesting to include a broader range of causes for immunosuppression.
Conflicts of interestThe paper authors have no present or potential conflict of interests.
The project had no funding.