Maximum inspiratory (Pimax) and expiratory (Pemax) mouth pressures are commonly used to detect respiratory muscle weakness resorting to predictive equations established for healthy people. There are several predictive equations, but they are widespread in the literature. This study aimed to review the existent predictive equations of maximum inspiratory (Pimax) and expiratory (Pemax) mouth pressures for adults. Additionally, we aimed to identify which ones were generated based on international standards.
MethodsA systematic review of predictive equations of Pimax and Pemax for healthy adults was conducted. A comprehensive search was performed of Cochrane Library, EBSCO, PubMed, Scopus and Web of Science to identify studies that presented at least one equation for Pimax or Pemax developed for healthy adults. The quality of studies was assessed by two reviewers with the Quality Assessment of Diagnostic Accuracy Studies (Quadas-2).
ResultsRisk of bias was high in 8 of the 20 studies included. Forty-two Pimax and 34 Pemax equations were found, mostly using the variables age (n=39), weight (n=20) and height (n=8). These equations explained 3 to 96% of the Pimax/Pemax variance. They were developed with individuals from 11 countries (Portugal not included). Twelve Pimax and eight Pemax equations complied with international standards.
ConclusionsThis review gathered the predictive equations that have been developed for both Pimax and Pemax, however most were generated from unstandardized procedures. Future studies should explore the suitability of these equations for populations for which specific ones are not available, such as the Portuguese population, and develop new equations if necessary.
Respiratory muscle weakness is an important clinical problem as it contributes to higher levels of dyspnoea14 and limits exercise capacity,15 impairing patients’ daily functioning and health-related quality of life.16 Respiratory muscle weakness is known to be diminished in 20–30% of patients with advanced chronic obstructive pulmonary disease (COPD),17 30–50% of patients with chronic heart failure18 and is frequently undetected in patients with neuromuscular diseases.19 Hence, more attention to this clinical parameter is needed and respiratory muscle strength should be routinely assessed in clinical practice.
Maximum respiratory mouth pressures are commonly used to assess respiratory muscle strength. But, despite existent international standards on measurement procedures,20 there is no consensus on which cut-offs to use to identify respiratory muscle weakness.13,20 Currently, absolute values of maximum inspiratory mouth pressure (Pimax) below −60cmH2O in men and −40cmH2O in women13 are widely used for detecting inspiratory muscle weakness. However, these pressures are influenced by several personal characteristics (e.g., age, height) and therefore, a more suitable interpretation of respiratory muscle strength is commonly performed, using predictive equations of Pimax and maximum expiratory mouth pressure (Pemax).21,22 These equations are available, but they are widespread in the literature. Although one systematic review has been conducted on this topic,23 it is from 7 years ago, and more predictive equations have been developed since.24,25 Furthermore, equations for Pemax have not been reviewed yet.23 This is a serious gap in the literature. Expiratory muscle weakness is also important to detect, as it can increase residual volume,20 and thus worsen the impaired breathing pattern in individuals with respiratory diseases, namely patients with COPD and hyperinflation.
Therefore, this study aimed to review the existent predictive equations of Pimax and Pemax for adults. Additionally, we aimed to identify which ones were generated based on international standards.
This information can be helpful to identify future suitable equations and clinically relevant respiratory muscle weakness in the Portuguese population.
Materials and methodsThis is a systematic review of the literature, reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.26 The protocol was registered in the international prospective register of systematic reviews (PROSPERO) (ID: CRD42018102854).
Search strategyAfter ensuring that there was no similar systematic review on PROSPERO or the Cochrane Library, a systematic search by title, abstract and keywords was conducted in the Cochrane Library, EBSCO, PubMed, Scopus and Web of Science in September 2018. Additional searches were performed in weekly automatic updates retrieved from the databases until December 2019. References of each included study were hand searched for potentially eligible studies. Appendix A (supplementary material) reports the full search strategy.
Study selectionAfter completion of databases search, all duplicates were removed. Then, one author screened each article for the scope of the review by their title, abstract and keywords. In parallel, an independent researcher screened 10% of all abstracts for eligibility to be included in the study. Full text of the articles was assessed, and papers excluded according to the eligibility criteria. Studies were included if: (1) included healthy adults (≥18 years), (2) developed at least one predictive equation for either Pimax or Pemax (mouth pressures), and (3) were written in English, French, Portuguese or Spanish. Studies were excluded if they were qualitative studies, research protocols, thesis/dissertations, abstracts, letters to the editor, news, case studies, book chapters, guidelines, position papers and unpublished work.
In cases of uncertainty, the decision to include/exclude the article was debated between the two reviewers and a third member was consulted to reach consensus.
Data extractionData were extracted to a predesigned structured table with author's name, year and country, participant characteristics (sample size, number of women and men, age and body mass index (BMI)), smoking status, equipment and protocol used to assess Pimax and Pemax, established predictive equation(s), lower limits of normality (LLN), standard error of estimate (SEE) and coefficient of determination (R2). The table was built in an excel file format to facilitate calculations when needed and then transformed and simplified to a word format.
A second table was built to aid visualization of the equations found, their explanation coefficients and which ones complied with the American Thoracic Society/European Respiratory Society standards (Pimax measured at residual volume, Pemax measured near total lung capacity, use of a flanged mouthpiece, use of noseclip not mandatory, holding pressure for ≥1.5s but not much longer, avoid use of aneroid manometers, patients supports cheeks during maneuver, 3 maneuvers with less than 20% variability).20
The accuracy of the extracted data was verified by two reviewers and confirmed by all authors. All corresponding authors of the included studies were contacted by e-mail in case of missing data.
Quality assessmentTwo reviewers independently assessed the quality of the included studies with the Quality Assessment of Diagnostic Accuracy Studies (Quadas-2).27 This scale has two dimensions (risk of bias and applicability concerns) and four domains (patient selection, index test, reference standard and flow and timing) that are scored with unclear risk, low risk, or high risk.27 Consistency of the quality assessment performed by the two reviewers was explored with the inter-rater agreement analysis using Cohen's kappa through SPSS statistics (IBM, version 25.0) and interpreted as <0: poor agreement; 0.00–0.20: slight agreement; 0.21–0.40: fair agreement; 0.41–0.60: moderate agreement; 0.61–0.80: substantial agreement; 0.81–1.00: almost perfect agreement.28
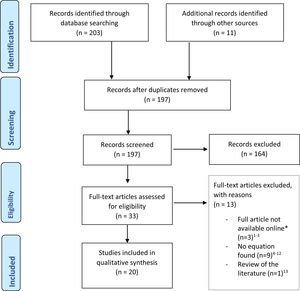
ResultsStudy selectionThe databases search identified 203 records. Eleven additional records were identified through hand searches of references of published articles and systematic reviews on the topic. After removing duplicates, 197 studies were screened. Of these, 164 studies were excluded by title, abstract or keywords, as they did not comply with the inclusion/exclusion criteria. Of the remaining 33 studies, 13 were excluded due to: unavailability of full-text (n=3),1–3 no equations for Pimax or Pemax being developed (n=9),4–12 and being a review of the literature (n=1).13 Twenty studies were included.24,25,29–46 A PRISMA flow diagram can be found in Fig. 1.
Quality assessmentA detailed view of the quality assessment is presented in Table B.1 (Appendix B). Overall, the quality of studies was good. Risk of bias was high in eight studies,24,30,34,35,39,41,43,45 mainly due to inclusion of participants by convenience, and in three studies the eligibility criteria was not clear.29,31,37 Risk of bias in the index test was high in one study.41 Concerns with applicability were unclear for patient selection and index test in eleven studies.24,29–31,34,36–38,41,45,46 Only three studies showed unclear risk for applicability concerns regarding the reference standard.31,32,43 Quality assessment of the studies revealed substantial agreement between the two reviewers (kappa=0.74, 95% CI 0.59–0.86).
Study characteristicsA detailed description of the studies can be found in Table 1. The 20 studies included a total of 9643 healthy individuals (5146 women, 4497 men). Most studies included young and older adults with ages between 10 and 90 years old (n=16),24,25,29–31,34–40,43–47 one study had only young adults (18–34 years old)41 and three studies had only middle-aged and older adults (45–85 years old).32,33,42 Seventeen studies reported the BMI, which ranged from 18 to 41.7kg/m2.24,25,30,32–36,38–46 Twelve studies excluded smokers.24,25,32–35,37,42–46 Seven included smokers and reported no differences in maximum respiratory pressures between smokers and non-smokers,29–31,36,38–40 and one study did not report this characteristic.41
Characteristics of the included studies (n=20).
| Author (year) | Country | N (sex, n) Age (range) BMI, mean | Smoking status | Equipment used | Protocol | Equation | LLN, cmH2O/kPA | SEE, cmH2O/kPA | R2, % |
|---|---|---|---|---|---|---|---|---|---|
| Black and Hyatt (1969)29 | United States of America | n=120n (women)=60n (men)=6020–70yBMI: NR | Smokers included. (number NR) | Two diaphragm gauges mounted on a metal bar connected to a pressure tap in the distal end of the cylinder by rigid plastic tubing; one gauge recorded negative pressure and the other recorded positive pressure. The gauges were calibrated with a pressure transducer | Position: sittingNose clip: yesHandling: The subject held the metal cylinder in his hand and pressed the mouthpiece tightly against his lips during the measurement;Pimax measurement: near RVPemax measurement: near TLCUnit: cmH2OHolding: ≥1sNumber of repetitions: ≥2Value used: higher | Pimax=104−(0.51×age)Pemax=170−(0.53×age)Pimax=143−(0.55×age)Pemax=268−(1.03×age) | NRNRNRNR | NRNRNRNR | NRNRNRNR |
| Wilson et al. (1984)30 | United Kingdom | n=135n (women)=87n (men)=4818–70yBMI:23.1kg/m223.3kg/m2 | Included smokers (number NR) | Gauges manufactured for the study and with the range −200 to +250cmH2O | Position: sittingNose clip: noHandling: NRPimax measurement: at RVPemax measurement: at TLCUnit: cmH2OHolding: ≥1sNumber of repetitions: ≥3 with 2 identical readings and 1min intervalValue used: NR | Pimax=−43+(0.71×Heightcm)Pemax=3.5+(0.55×Heightcm)Pimax=142−(1.03×age)Pemax=180−(0.91×age) | NRNRNRNR | NRNRNRNR | 552114 |
| Bruschi et al. (1992)31 | Italy | n=749n (women)=423n (men)=32618–70yBMI: NR | n=326 non-smokersn=299 smokers/former smokers | A differential pressure transducer (Honeywell, Freeport) with a pressure range of ±300cmH2O connected to an amplifier (Gould Instruments, Ballanvilliers, France) | Position: sittingNose clip: yesHandling: the subjects held the cheeks with their hands during the manoeuvers.Pimax measurement: near RV and FRCPemax measurement: near TLC and FRCUnit: cmH2OHolding: NRNumber of repetitions: ≥5Value used: highest | PimaxRV=4.02−(0.26×sex)−(0.004×age)+(0.47×BSA)PimaxFRC=3.89−(0.22×sex)−(0.004×age)+(0.52×BSA)PemaxTLC=4.48−(0.18×sex)−(0.0004×age)−(0.003×sex×age)+(0.25×BSA)PemaxFRC=4.54−(0.35×sex)−(0.003×age)+(0.24×BSA)Sex: male=0; female=1 | NRNRNRNR | 0.330.340.210.23 | 27254646 |
| Enright et al. (1994)32 | United States of America | n=2871Pimax=1602Pemax=292Pimax=1269Pemax=24467–78yBMI:26.5kg/m226.6kg/m2 | All non-smokers | MRP-PC system (Scientific and Medical Instrument Co., Doylestown, PA).Mechanical gauge reading ±150cmH2O | Position: sitting with exception of severely obese people.Nose clip: yesHandling: NR.Pimax measurement: near RVPemax measurement: near TLCUnit: cmH2OHolding: 2sNumber of repetitions: 3–5Value used: highest value not exceeding the secondhighest value by 10% | Pimax=(0.133 Wtlbs)−(0.805 Age)+96Pemax=(0.344 Wtlbs)−(2.12 Age)+219Pimax=(0.131 Wtlbs)−(1.27 Age)+153Pemax=(0.250 Wtlbs)−(2.95 Age)+347 | −32−52−41−71 | 21.5033.3025.4042.50 | 8181015 |
| Enright et al. (1995)33 | United States of America | n=288n (women)=176n (men)=11265–85yBMI:26.0kg/m226.4kg/m2 | All non-smokers | A mechanical and electronic pressure gauge (MRP1, ±250cmH2O, model 83KC-37, Marshalltown, Iowa) | Position: sittingNose clip: yesHandling: NR.Pimax measurement: near RVPemax measurement: near TLCUnit: cmH2OHolding: 2sNumber of repetitions: 5Value used: highest not exceeding the secondhighest value by 10% | Pimax=118−(0.9×age)+(0.10×Wtlbs)Pemax=179−(1.68×age)+(0.36×Wtlbs)Pimax=149−age+(0.10×Wtlbs)Pemax=278−(2.27×age+0.28×Wtlbs) | −38−75−42−52 | NRNRNRNR | 823512 |
| Johan et al. (1997)34 | China, Malaysia and India | China=221n=221n (women)=90n (men)=131Malaysian=111n (women)=42n (men)=69Indian=120n (women)=43n (men)=7720–80yBMI:China21.8kg/m223.0kg/m2Malaysia24.1kg/m223.9kg/m2India23.2kg/m224.3kg/m2 | All non-smokers or smoked <400 cigarettes in their lifetime | Ashcroft pressure gauges (Ashcroft, USA) with a flanged mouthpiece. | Position: sittingNose clip: yesHandling: NR.Pimax measurement: near RVPemax measurement: near TLCUnit: cmH2OHolding: ≥1sNumber of repetitions: ≥3Value used: highest value | China:Pimax=68.80−(0.49×age)−(0.05×Heightcm)+(0.22×Wtkg)Pemax=112.14−(0.59×age)−(0.11×Heightcm)−(0.07×Wtkg)Pimax=37.24−(0.67×age)+(0.15×Heightcm)+(0.85×Wtkg)Pemax=−106.17−(0.52×age)+(1.05×Heightcm)+(1.03×Wtkg)Malaysia:Pimax=52.48+(0.18×age)−(0.09×Heightcm)+(0.12×Wtkg)Pemax=181.87−(0.16×age)−(0.90×Heightcm)−(0.43×Wtkg)Pimax=151.32−(0.33×age)−(0.55×Heightcm)+(0.38×Wtkg)Pemax=109.82+(0.05×age)−(0.22×Heightcm)+(0.30×Wtkg)India:Pimax=54.65−(0.48×age)−(0.01×Heightcm)+(0.24×Wtkg)Pemax=130.36−(0.49×age)−(0.40×Heightcm)+(0.17×Wtkg)Pimax=112.47−(0.31×age)−(0.31×Heightcm)+(0.51×Wtkg)Pemax=−13.66−(0.62×age)+(0.79×Heightcm)+(0.06×Wtkg) | NRNRNRNRNRNRNRNRNRNRNRNR | NRNRNRNRNRNRNRNRNRNRNRNR | 262941421424221534251933 |
| Morales et al. (1997)35 | Spain | n=264n (women)=135n (men)=12918–83yBMI:26.3kg/m226.6kg/m2 | All non-smokers | T tube connected to a transductor (Gouid Statham, P23 ID) connected to an amplifier (Electronics for Medicine, Simultrace Recorder VR-6, V-2203) with a 50–300mmHg | Position: sittingNose clip: yesHandling: Handling: the subjects held the cheeks with their hands during the manoeuversPimax measurement: at RVPemax measurement: near TLCUnit: cmH2OHolding: 2–3sNumber of repetitions: <10Value used: highest value of 5 repetitions with 5% variability | Pimax=(−0.64×age)+125.18Pemax=(−0.57×age)+(0.65×Wtkg)+116.23Pimax=(−1.03×age)+(0.59×Wtkg)+133.07Pemax=(−1.31×age)+263.12 | NRNRNRNR | 23.227.729.342.6 | 19133022 |
| Harik-khan et al. (1998)36 | United States of America | n=267n (women)=128n (men)=13920–90yBMI:23.9kg/m225.8kg/m2 | 23% former smokers35% former smokers9% occasional smokers13% occasional smokers7% current smokers4% current smokers | Solid-state pressure transducer (S&M Instruments Co., Doylestown, PA) interfaced with a computer | Position: NRNose clip: NRHandling: NR.Pimax measurement: near RVUnit: cmH2OHolding: 2sNumber of repetitions: 3–5Value used: one that showed a 2s plateau of inspiratoryeffort with 10% variability | Pimax=171−(0.694×age)+(0.861×Wtkg)−(0.743×Heightcm)Pimax=126−(1.028×age)+(0.343×Wtkg) | −32−37 | 18.522.4 | 3142 |
| Neder et al. (1999)37 | Brazil | n=100n (women)=50n (men)=5020–80yBMI: NR | All non-smokers | Manual shutter apparatus with the maximal pressures measured using a manometer, aneroid-type gauge (±300cmH2O) (Imebrás, São Paulo, SP, Brazil) | Position: sittingNose clip: yesHandling: the subjects held the cheeks with one hand during the maneuversPimax measurement: at RVPemax measurement: near TLCUnit: cmH2OHolding: ≥1sNumber of repetitions: 3–5 repetitions with up to 10% variability and 1min rest between repetitionsValue used: highest value unless it was obtained from the last effort | Pimax=(−0.49×age)+110.4Pemax=(−0.61×age)+115.6Pimax=(−0.80×age)+155.3Pemax=(−0.81×age)+165.3 | NRNRNRNR | 9.111.217.315.6 | 47484848 |
| Hautmann et al. (2000)38 | Germany | n=504n (women)=256n (men)=24818–82yBMI:23.9kg/m225.8kg/m2 | 87.7% never smokedMean 17 pack-years for current/former smokers | Pressure gauge as an integral part of the pneumotachograph – piezzo-element (Type SX01, Sensym Corp, Milpitas, California, U.S.A.) was calibrated by the manufacturer | Position: sittingNose clip: yesHandling: NR.Pimax measurement: near RVUnit: kPAHolding: 2sNumber of repetitions: ≥7 with 20–90s of rest between repetitionsValue used: highest value maintained for ≥1s, with two consecutive measurementsFailing to improve the preceding highest value. | Pimax=(−0.024×age)+8.55Pimax=(0.158×BMI)−(0.051×age)+8.22 | 0.590.60 | NRNR | 39 |
| Wohlgemuth et al. (2003)39 | Netherlands | n=252n (women)=126n (men)=12618–70yBMI:26.2kg/m225.1kg/m2 | n=64 smokers/former smokers | Morgan manometer (type Pmax) containing a small leak (internal diameter 2mm, 2cm length) connected to a facemask | Position: sittingNose clip: Yes for mouthpieceHandling: Researcher held the facemaskPimax measurement: at RVPemax measurement: at TLCUnit: kPAHolding: 1sNumber of repetitions: ≥3 with maximum 5% variabilityValue used: highest | Pimax=7.224−(0.0406×age)+(0.032×Wtkg)+(3.745×sex)−(0.041×sex×age)Pemax=9.887−(0.0556×age)+(0.035×Wtkg)+(5.224×sex)−(0.049×sex×age)sex: males=1 females=0 | NRNR | 1.582.23 | 5150 |
| Windisch et al. (2004)40 | Germany | n=533n (women)=304n (men)=22910–90yBMI:23.9kg/m224.2kg/m2 | n=317 current smokersn (women)=84 former smokersn (men)=128 never smokers | Transportable apparatus connected to a computersystem (ZAN 100; ZAN1, Oberthulba, Germany) | Position: sittingNose clip: YesHandling: NRPimax measurement: at RV and FRCUnit: kPAHolding: 1sNumber of repetitions: ≥7 and 30–120s intervalValue used: highest | Pimax=y+(−0.08×age)+(0.04×Wtkg)+(0.11x BMI)aPimax=y+(−0.04×age)+(0.06×Wtkg)+(0.24×BMI)a | 0.9–5.80.9–5.8 | NRNR | 132 |
| Lausted et al. (2006)41 | United States of America | n=48n (women)=29n (men)=1918–34yBMI:22.5kg/m223.7kg/m2 | NR | Spirometry system (Collins™, Braintree, MA) | Position: NRNose clip: NRHandling: NR.Pimax measurement: at different volumes (10–90%VC)Pemax measurement: at different volumes (10–90%VC)Unit: cmH2OHolding: 2sNumber of repetitions: ≥3 with ≥1min of rest between repetitionsValue used: highest | Pimax=0.234×Ln (100%−%VC)−0.0828Pemax=0.1426×Ln (%VC)+0.3402 | NRNR | NRNR | 9696 |
| Sachs et al. (2009)42 | United States of America | n=1755n (women)=883n (men)=87245–84yBMI:18.5–35kg/m2 | Excluded current smokers, smoking history for the healthy subgroup NR | MRP-PC system (Scientific and Medical Instrument Co., Doylestown, PA).Calibration of the MRP transducer was checked each week against the mechanical gauge reading [−150–150cmH2O] | Position: sittingNose clip: yesHandling: the researcher pressed the cheeks of the participantPimax measurement: at RVUnit: cmH2OHolding: ≥1sNumber of repetitions: 5 with 1min rest between repetitionsValue used: nearest 5cm H2O value from the highest 2 within 10 cmH2OQuality confirmed by a 5% random quality-control sample of participants | Pimax=−388+(1.77×age)+(−0.014×age2)+(0.41×Wtlbs)+(−0.0041×age×Wtlbs)+(4.69×Heightcm)+(−0.014×Height2cm)Pimax=9.8+(−0.31×age)+(1.47×Wtlbs)+(−0.0026×Wt2lbs)+(−0.0059×age×Wtlbs) | −36−40 | NRNR | 2721 |
| Costa et al. (2010)43 | Brazil | n=120n (women)=60n (men)=6020–80yBMI: 18.0–29.5kg/m2 | All non-smokers | Calibrated aneroid vacuum manometer (GER-AR, São Paulo, Brazil, range of ±300cmH2O. | Position: sittingNose clip: yesHandling: NR.Pimax measurement: near RVPemax measurement: near TLCUnit: cmH2OHolding: ≥1sNumber of repetitions: ≥3Value used: highest value not exceeding the secondhighest value by 10% | Pimax=(−0.46×age)+74.25Pemax=(−0.68×age)+119.35Pimax=(−1.24×age)+232.37Pemax=(−1.26×age)+183.31 | −28.83−23.24−23.38−38.95 | 17.2017.7618.8824.22 | 24.835.160.748.9 |
| Simões et al. (2010)44 | Brazil | n=140n (women)=70n (men)=7020–89yBMI:24.6kg/m224.7kg/m2 | All non-smokers | Aneroid vacuum manometer (GER-AR, São Paulo, SP, Brazil) with an operational interval of ±300cmH2O was used | Position: sittingNose clip: yesHandling: NRPimax measurement: at RVPemax measurement: at TLCUnit: cmH2OHolding: ≥1sNumber of repetitions: ≥3 with ≤10% variabilityValue used: highest | Pimax=(−0.85×age)+80.7+(−0.3×Wtkg)Pemax=(−0.89×age)+125.1+(−0.18×Wtkg)Pimax=(−0.76×age)+125Pemax=(−0.83×age)+87.69 | −69−19.6−24.6−24.7 | 41.9511.9014.9715.0 | 84777284 |
| Gopalakrishna et al. (2011)45 | India | n=250n (women)=125n (men)=12520–70yBMI:23.17kg/m223.54kg/m2 | All non-smokers | Morgan Pmax monitor [P.K Morgan Ltd. ME8 7ED] | Position: sitting with exception of severely obese people.Nose clip: yesHandling: NR.Pimax measurement: near RVPemax measurement: near TLCUnit: cmH2OHolding: 2sNumber of repetitions: ≥3 with 1min rest between repetitionsValue used: highest not exceeding the second highest value by 10% | Pimax=45.98+(6.47×age)Pemax=74.85−(0.32×age)Pimax=83.36−(0.25×age)Pemax=133.36−(0.907×age) | NRNRNRNR | NRNRNRNR | 6241840 |
| Obando et al. (2012)46 | Colombia | n=308n (women)=154n (men)=15420–86yBMI: 24.2kg/m2 | All non-smokers | Pressure gauge (MICROMEDICAL RPM brand, Micro Medical Limited, PO Box 6, Rochester, Kent ME1 2AZ UK), with a range of 300cmH2O | Position: sittingNose clip: yesHandling: NR.Pimax measurement: near RV during 3–4sUnit: cmH2OHolding: 2sPemax: near TLCNumber of repetitions: 3Value used: highest | Pimax=78.237−(−0.446×age)+(22.430×sex)+(8.550×BMI Classification)Pemax=−97.424+(19.788×sex)+(0.528×Wtkg)+(0.911×Heightcm)Values for sex not provided | NRNR | 23.1629.60 | 2633 |
| Pessoa et al. (2014)24 | Brazil | n=134n (women)=74n (men)=6020–89yBMI:24.0kg/m225.0kg/m2 | Non-current smokers. Previous smoking history NR | A digital manometer (NEPEB-LabCare/UFMG) with pressure transducers with an operating range of 500cmH2O | Position: sittingNose clip: yesHandling: the researcher pressed the cheeks of the participantPimax measurement: at RVPemax measurement: near TLCUnit: cmH2OHolding: ≥1.5sNumber of repetitions: ≥5 with 1min rest between repetitionsValue used: highest value with three reproducible repetitions (one with variation less than or equal to 10% and the other with a variation of no more than 20% of higher value) | Pimax=63.27−(0.55×age)+(17.96×sex)+(0.58×Wtkg)Pemax=−61.41+(2.29×age) –(0.03×age2)+(33.72×sex)+(1.40×waistcm)Sex: males=1; females=0 | −43−54 | 26.332.8 | 3449 |
| Sanchez et al. (2018)25 | Brazil | n=353n (women)=229n (men)=12418–89yBMI:31.4±10.3kg/m2 | All non-smokers | Analogical manometer “Wika”, calibrated and graduated to 6300cmH2O | Position: sittingNose clip: yesHandling: NRPimax measurement: at RVPemax measurement: near TLCUnit: cmH2OHolding: ≥1sNumber of repetitions: 4 with 1min rest between repetitionsValue used: highest value with two reproducible repetitions and a variation of no more than 10% of higher value | Model 2:Pimax=–94.75+(0.816×age)−(1.822×BMI)Pemax=91.58−(0.556×age)+(0.798×BMI)Pimax=–108.16+(1.307×age)−(2.904×BMI)Pemax=98.36−(0.672×age)+(1.759×BMI)Model 3:Pimax=–95.54+(0.748×age)−(0.688×Wtkg)Pemax=87.20−(0.506×age)+(0.350×Wtkg)Pimax=–110.07+(1.208×age)−(0.942×Wtkg)Pemax=98.84−(0.610×age)+(0.576×Wtkg) | NRNRNRNRNRNRNRNR | 63.936.563.936.563.836.163.836.1 | 21.328.421.328.421.729.921.729.9 |
Legend: BMI: body mass index; BSA: body surface area; FRC: functional residual capacity; LLN: lower limit of normality; Ln: natural logarithm; Pemax: maximum expiratory pressure; Pimax: maximum inspiratory pressure; NR: not reported; R2: coefficient of determination; RV: residual volume; SEE: standard error of estimation; TLC: total lung capacity; VC: vital capacity; Wt: weight.
Of the 20 studies, ten used digital manometers,24,36,37,39,40,42–46 eight used mechanical gauges,25,29–35 one used a gauge associated with a pneumotachograph,38 whilst in another the gauge was associated with a spirometry system.41 Assessment protocol varied across studies. The vast majority of studies performed measurements with the participants in a sitting position (n=18)24,25,29–35,37–40,42–46 and using a nose clip.24,25,29,31–35,37–40,42–46 Two studies did not report either the position or use of a nose clip.36,41 Only one study performed the measurement at different volumes for both Pimax and Pemax (percentage of vital capacity),41 whilst 19 studies measured Pimax at residual volume24,25,29–40,42–46 and 16 measured Pemax at total lung capacity.24,25,29,31–37,39,41,43–46,48 Half of the studies reported holding pressures for ≥1s,25,29,30,34,37,39,40,42–44 eight for 2s,32,33,35,36,38,41,45,46 one for ≥1.5s,24 and one study did not report the holding time31. Number of repetitions of the procedure varied between 2 and 10, with most studies (n=18) reporting at least 3 repetitions.24,30–46
A total of 76 predictive equations were found, 42 for Pimax and 34 for Pemax. Variables most frequently used in the equations were: age (Pimax n=22; Pemax n=17),24,25,29–40,42–46 weight (n=11; n=9),24,25,32–36,39,40,42,44,46 height (n=5; n=3)30,34,36,42,46 and sex (n=4; n=4).24,31,39,46 Most studies produced distinct equations for each sex (n=15),25,29,30,32–38,40,42–45 with only five studies reporting a single equation for both.24,31,39,41,46 BMI was used in five Pimax equations25,38,46 and in two Pemax equations,25 and waist circumference in one Pemax equation.24 Body surface area was also used in 2 Pimax and 2 Pemax equations.31 Only 9 studies reported LLN values,24,33,36,38,40,42–44 12 reported the SEE24,25,31,32,35–37,39,40,43,44,46 and almost all (n=19) the R2.24,25,30–46
Overall the proposed equations explained between 3 and 96% of the variance of Pimax/Pemax, with most studies (n=14) explaining less than 50%. Equations were developed with individuals from 11 countries, with the most representative continents being North America (n=6), Europe (n=6), South America (n=5) and Asia (n=4). No developed equations were found in Northern Asia, Africa or Oceania. A world map of the distribution of the existent predicted equations and respective range of R2 can be found in Fig. 2. Of the 42 Pimax and 34 Pemax equations, 12 and 8 respectively, were generated using procedures that globally complied with the international standards. Of the remaining 56 equations using procedures that have not followed the ATS/ERS guidelines, only 36 were developed before publication of the guidelines. Table 2 summarizes the predictive equations found for respiratory muscle strength.
List of available predictive equations for maximum inspiratory (Pimax) and expiratory (Pemax) pressures for healthy adults.
| Author (year) | Equation Pimax women | Equation Pimax men | Equation Pemax women | Equation Pemax men | R2 |
|---|---|---|---|---|---|
| Black and Hyatt (1969)29 | 104−(0.51×age) | 143−(0.55×age) | 170−(0.53×age) | 268−(1.03×age) | NR |
| Wilson et al. (1984)30 | −43+(0.71×Heightcm) | 142 –(1.03×age) | 3.5+(0.55×Heightcm) | 180−(0.91×age) | 5–21 |
| Bruschi et al. (1992)31 | 4.02−0.26−(0.004×age)+(0.47×BSA) (from RV)3.89−0.22−(0.004×age)+(0.52×BSA) (from FRC) | RV=4.02−(0.004×age)+(0.47×BSA) (from RV)3.89−(0.004×age)+(0.52×BSA) (from FRC) | 4.48−0.18−(0.0004×age)−(0.003×age)+(0.25×BSA) (from TLC)4.54−0.35−(0.003×age)+(0.24×BSA) (from FRC) | 4.48−(0.0004×age)−(0.25×BSA) (from TLC)4.54−(0.003×age)+(0.24×BSA) (from FRC) | 25–46 |
| Enright et al. (1994)32a | (0.133 Wtlbs)−(0.805 Age)+96 | (0.131 Wtlbs)−(1.27 Age)+153 | (0.344 Wtlbs)−(2.12 Age)+219 | (0.250 Wtlbs)−(2.95 Age)+347 | 8–18 |
| Enright et al. (1995)33a | 118−(0.9×age)+(0.10×Wtlbs) | 149−age+(0.10×Wtlbs) | 179−(1.68×age)+(0.36×Wtlbs) | 278−(2.27×age+0.28×Wtlbs) | 5–23 |
| Johan et al. (1997)34 | China:68.80−(0.49×age)−(0.05×Heightcm)+(0.22×Wtkg)Malaysia:52.48+(0.18×age)−(0.09×Heightcm)+(0.12×Wtkg)India:54.65−(0.48×age)−(0.01×Heightcm)+(0.24×Wtkg) | China:37.24−(0.67×age)+(0.15×Heightcm)+(0.85×Wtkg)Malaysia:151.32−(0.33×age)−(0.55×Heightcm)+(0.38×Wtkg)India:112.47−(0.31×age)−(0.31×Heightcm)+(0.51×Wtkg) | China:112.14−(0.59×age)−(0.11×Heightcm)−(0.07×Wtkg)Malaysia:181.87−(0.16×age)−(0.90×Heightcm)−(0.43×Wtkg)India:130.36−(0.49×age)−(0.40×Heightcm)+(0.17×Wtkg) | China:−106.17−(0.52×age)+(1.05×Heightcm)+(1.03×Wtkg)Malaysia:109.82+(0.05×age)−(0.22×Heightcm)+(0.30×Wtkg)India:−13.66−(0.62×age)+(0.79×Heightcm)+(0.06×Wtkg) | 14–42 |
| Morales et al. (1997)35 | (−0.64×age)+125.18 | (−1.03×age)+(0.59×Wtkg)+133.07 | (−0.57×age)+(0.65×Wtkg)+116.23 | (−1.31×age)+263.12 | 13–30 |
| Harik-khan et al. (1998)36 | 171−(0.694×age)+(0.861×Wtkg)−(0.743×Heightcm) | 126−(1.028×age)+(0.343×Wtkg) | 31–42 | ||
| Neder et al. (1999)37 | (−0.49×age)+110.4 | (−0.80×age)+155.3 | (−0.61×age)+115.6 | (−0.81×age)+165.3 | 47–48 |
| Hautmann et al. (2000)38a | (−0.024×age)+8.55 | (0.158×BMI)−(0.051×age)+8.22 | 3–9 | ||
| Wohlgemuth et al. (2003)39 | 7.224−(0.0406×age)+(0.032×Wtkg)+3.745 | 7.224−(0.0406×age)+(0.032×Wtkg)−(0.041×age) | 9.887−(0.0556×age)+(0.035×Wtkg)+5.224 | 9.887−(0.0556×age)+(0.035×Wtkg)−(0.049×age) | 50–51 |
| Windisch et al. (2004)40b | y+(−0.08×age)+(0.04×Wtkg)+(0.11x BMI)a | y+(−0.04×age)+(0.06×Wtkg)+(0.24×BMI)a | 2–13 | ||
| Lausted et al. (2006)41 | 0.234×Ln (100%−%VC)−0.0828 | 0.234×Ln (100%−%VC)−0.0828 | 0.1426×Ln (%VC)+0.3402 | 0.1426×Ln (%VC)+0.3402 | 96 |
| Sachs et al. (2009)42a | −388+(1.77×age)+(−0.014×age2)+(0.41×Wtlbs)+(−0.0041×age×Wtlbs)+(4.69×Heightcm)+(−0.014×Height2cm) | 9.8+(−0.31×age)+(1.47×Wtlbs)+(−0.0026×Wt2lbs)+(−0.0059×age×Wtlbs) | 21–27 | ||
| Costa et al. (2010)43 | (−0.46×age)+74.25 | (−1.24×age)+232.37 | (−0.68×age)+119.35 | (−1.26×age)+183.31 | 24.8–60.7 |
| Simões et al. (2010)44 | (−0.85×age)+80.7+(−0.3×Wtkg) | (−0.76×age)+125 | (−0.89×age)+125.1+(−0.18×Wtkg) | (−0.83×age)+87.69 | 72–84 |
| Gopalakrishna et al. (2011)45a | 45.98+(6.47×age) | 83.36−(0.25×age) | 74.85−(0.32×age) | 133.36−(0.907×age) | 6–40 |
| Obando et al. (2012)46 | 78.237−(−0.446×age)+(22.430×sex)+(8.550×BMI Classification)Values for sex not provided | 78.237−(−0.446×age)+(22.430×sex)+(8.550×BMI Classification)Values for sex not provided | −97.424+(19.788×sex)+(0.528×Wtkg)+(0.911×Heightcm)Values for sex not provided | −97.424+(19.788×sex)+(0.528×Wtkg)+(0.911×Heightcm)Values for sex not provided | 26–33 |
| Pessoa et al. (2014)24a | 63.27−(0.55×age)+(0.58×Wtkg) | 63.27−(0.55×age)+(17.96)+(0.58×Wtkg) | −61.41+(2.29×age)−(0.03×age2)+(1.40×waistcm) | −61.41+(2.29×age)−(0.03×age2)+33.72+(1.40×waistcm) | 34–49 |
| Sanchez et al. (2018)25 | Model 2:–94.75+(0.816×age)−(1.822×BMI)Model 3:–95.54+(0.748×age)−(0.688×Wtkg) | Model 2:−108.16+(1.307×age)−(2.904×BMI)Model 3:−110.07+(1.208×age)−(0.942×Wtkg) | Model 2:91.58−(0.556×age)+(0.798×BMI)Model 3:87.20−(0.506×age)+(0.350×Wtkg) | Model 2:98.36−(0.672×age)+(1.759×BMI)Model 3:98.84−(0.610×age)+(0.576×Wtkg) | 21.3–29.9 |
Legend:
Pimax: maximum inspiratory pressure; Pemax: maximum expiratory pressure; BSC: body surface area; %VC: percentage of vital capacity; Wtlb: weight in pounds; Wtkg weight in kilograms; BMI: body mass index; RV: residual volume; TLC: Total lung capacity; FRC: Functional residual capacity; Heightcm: Height in centimeters; NR: Not reported.
This study has shown that there are 42 Pimax and 34 Pemax predictive equations developed for eleven countries. From these equations, only 12 for Pimax and 8 for Pemax derived from procedures that complied globally with the international standards.
Although a previous systematic review on respiratory muscle strength was published in 2014,23 it only reviewed Pimax predictive equations. Therefore, the present systematic review brings novelty to the body of literature as it is not limited to updating the previous systematic review, but also reviews the Pemax equations and identifies which equations were generated following the ATS/ERS guidelines.
A substantial number of equations across distinct continents were found for respiratory muscle strength, however, there is no equation available for Northern Asia, Africa or Oceania. As reference values and predictive equations are population-specific, the suitability of the existent equations needs to be tested in populations for which specific ones are not available, such as the Portuguese population. This analysis may stress the need to develop specific equations for some populations. These are important steps to interpret with confidence the values of Pimax/Pemax and guide further assessments or interventions.
Most equations integrate easy to collect variables, with the most weighted variables in the models being age, weight and height. These variables are also frequently present in predictive equations for quadriceps muscle strength47 and exercise capacity tests,49 which makes them highly accepted variables to enter prediction models. Predictive equations showed a high variability of explanation, and most studies explained less than 50% of the variance in respiratory muscle strength. Only four studies,39,41,43,44 explained between 50% and 96% although the study presenting 96% of explanation had a difficult equation to apply in clinical practice, as it included vital capacity which is a more complex variable to obtain in many clinical settings.41 Poor explanation of the variance will affect the accuracy of the interpretation of results, implying that the equation might not be suitable. Although no recommendations exist for the use of specific predictive equations, studies developing new equations should balance the quality of the predictive equations, i.e., taking the explanation of the variability into account, with their utility in clinical practice, i.e., including variables that are easy-to-use. Thus, novel variables, also easy to collect with high weight in equations may produce more powerful equations with better explanation coefficients.
Furthermore, this systematic review has shown that almost half of the equations were developed through measurements with non-digital equipment and variable protocols, which impair comparisons across studies and interpretation of the predictive values. Indeed, many studies showed lack of compliance with the ATS/ERS standards,20 by using different number of repetitions, not using a nose clip, and holding breath during data collection with different durations. This heterogeneity in the methodological procedures was expected for older studies, but not for the ones published after the guidelines (2002). Although, the impact of choosing an equation based on the ATS/ERS standards instead of unstandardized ones to identify respiratory muscle weakness needs further investigation, the fact is that continuing to use different procedures limits the advance of knowledge in the field and should therefore be considered carefully and be well-justified.
This study has some limitations that need to be acknowledged. Although all predictive equations have been revised, the analysis of the articles did not consider the size and characteristics of the included samples. In fact, a considerable amount of studies (n=8) had a high level of bias, which might have affected the validity and reliability of the equations proposed. Moreover, most equations were not validated with an independent sample. All these aspects have hindered our ability to make recommendations about which equation(s) should be used in clinical practice.
This review gathered the current predictive equations available in the literature for Pimax and Pemax and identifies which ones have followed the ATS/ERS standards. Future work could explore the suitability of the different available equations for populations to whom specific ones are not available, such as the Portuguese population, and only develop new equations for both Pimax and Pemax, if necessary.
Financial supportThis work was funded by Programa Operacional de Competitividade e Internacionalização – POCI, through Fundo Europeu de Desenvolvimento Regional – FEDER (POCI-01-0145-FEDER-007628 and POCI-01-0145-FEDER-028806), Fundação para a Ciência e Tecnologia (PTDC/DTP-PIC/2284/2014 and PTDC/SAU-SER/28806/2017) and under the project UID/BIM/04501/2019.
This work was presented as a Poster Discussion at the European Respiratory Society International Congress 2019.