Portugal is one of the countries with the highest number of visits to the emergency department (ED), 31% classified as “non-urgent” or “avoidable.” The objectives of our study were to evaluate the size and characteristics of patients with pulmonary disease who overuse the ED, and identify factors associated with mortality.
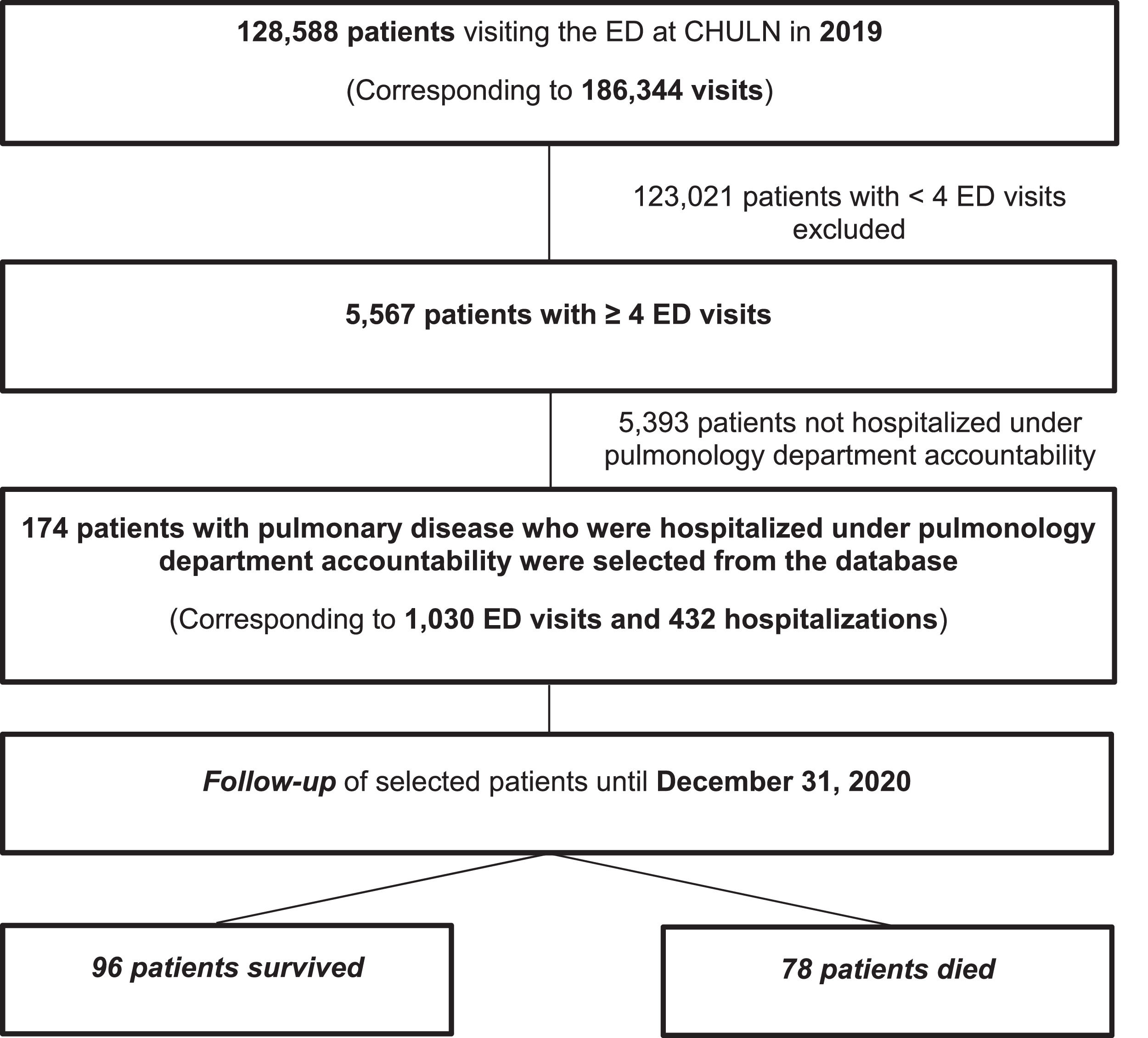
Materials and methodsA retrospective cohort study was conducted, based on the medical records of ED frequent users (ED-FU) with pulmonary disease who attended a university hospital center in the northern inner city of Lisbon from January 1 to December 31, 2019. To evaluate mortality, a follow-up until December 31, 2020 was performed.
ResultsOver 5,567 (4.3%) patients were identified as ED-FU and 174 (0.14%) had pulmonary disease as the main clinical condition, accounting for 1,030 ED visits. 77.2% of ED visits were categorized as “urgent/very urgent.” A high mean age (67.8 years), male gender, social and economic vulnerability, high burden of chronic disease and comorbidities, with a high degree of dependency, characterized the profile of these patients. A high proportion (33.9%) of patients did not have a family physician assigned and this was the most important factor associated with mortality (p<0.001; OR: 24.394; CI 95%: 6.777–87.805). Advanced cancer disease and autonomy deficit were other clinical factors that most determined the prognosis.
ConclusionsPulmonary ED-FU are a small group of ED-FU who constitute an aged and heterogeneous group with a high burden of chronic disease and disability. The lack of an assigned family physician was the most important factor associated with mortality, as well as advanced cancer disease and autonomy deficit.
The overuse of emergency departments (EDs) is a global problem, raising questions of whether many of these visits could be avoided. Visits to emergency services by Portuguese citizens show very similar values over time. In 2010, there were 6411,000 ED visits, and in 2019 over 6426,000 visits.1 This scenario places Portugal as the country in the Organization for Economic Co-operation and Development (OECD) with the highest number of ED visits (over 70 visits/100 vs. an OECD mean of 31/100 population in 2011).2 Further, according to national statistics, 31% of patients admitted to the ED in Portugal are “non-urgent,” “avoidable” or “inappropriate.”2 Reducing visits of avoidable ED frequent users (ED-FU) and the number of preventable hospital visits is a priority, as they use considerable resources and are disruptive to the health system.3 In Portugal, Hospital EDs are the only place in the National Health Service (NHS) where individuals have access to a full range of services at any time, regardless of their ability to pay or the severity of their condition. Providing ambulatory health care, such as primary health care (PHC), can prevent the use of the ED through clinical measures such as preventive treatment, early diagnosis of chronic disease exacerbation and adjustment of pharmacological therapy.2–5
ED-FU, defined as having four or more visits per year, poses a challenge to emergency services as they contribute to a disproportionate number of visits.3 Several factors associated with avoidable ED-FU visits have been described in the literature and are grouped into individual-centered factors, such as sociodemographic features or disease severity, and factors associated with the health system, such as PHC resources or the proximity of the patient’s home to the ED.3 Moreover, an important question is whether ED-FU may be inflicting poor service on themselves by choosing emergency care over seeking consistent care from their own family physician. Understanding the causes related to avoidable ED-FU visits, and identifying which ones are potentially modifiable, will allow the planning and implementation of health care strategies.
ED visits due to pulmonary disease are among the most common reasons for hospitalization in developed countries.3 In Portugal, respiratory hospitalizations are one of the main reasons for visiting EDs and represent the fifth leading cause of hospitalization.6
The objective of our study was to evaluate the size and characteristics of patients with pulmonary disease as their main clinical condition overusing the ED in a university hospital in Lisbon, during the year 2019, with regard to individual-centered factors and health care-associated characteristics. A secondary objective was to identify factors associated with mortality during a follow-up since the first ED visit until December 31, 2020.
MethodsStudy design and settingThe authors chose 2019, a non-pandemic typical year concerning ED utilization, to conduct the retrospective cohort study. The investigation was based on the electronic medical records analysis of individuals who attended the ED of Centro Hospitalar Universitário Lisboa Norte (CHULN) – Hospital de Santa Maria, in Lisbon, Portugal, from January 1, 2019, to December 31, 2019 (Fig. 1). In addition to the hospital records analysis, other national health platforms were used through their links to the hospital electronic platform. To evaluate the mortality of pulmonary ED-FU, a follow-up of the patients’ electronic data was conducted until December 31, 2020.
Study populationThe study population consisted of adult individuals with pulmonary disease and criteria of ED-FU, meaning a total number of yearly visits ≥ 4, including respiratory or non-respiratory ED visits.3 Frequent users (FU) were identified from a query of the computerized hospital management system. The inclusion criteria for pulmonary disease FU were hospitalizations in which lung disease was the main clinical problem. The query to identify this group was the code corresponding to being hospitalized under pulmonology department accountability and at least one pulmonary appointment. The exclusion criteria included all patients who were not under the responsibility of our pulmonology department. Patients were excluded if respiratory disease was not their main clinical condition.
Study protocolPatients were characterized based on individual-centered factors and health care-associated characteristics. Individual-centered factors included demographic, socioeconomic status and clinical features, obtained from the electronic clinical file (ALERT and Hospital GLINTT platforms). Disability, financial insufficiency, chronically ill patients with special medication according to national criteria, pensioners with pensions at or below the national minimum wage, solidarity supplement for the elderly and family physician assignment were obtained by special codes using the National User Registry (RNU). The comorbidity burden was evaluated with Charlson Comorbidity Index (CCI).7–9 Frailty status was evaluated with Clinical Frailty Scale (CFS).10,11 The characteristics of patients who died during follow-up (2019–2020) were analyzed and compared with the survivors within this period. Health care-associated characteristics included both information about the assignment of a family physician to each patient and the characterization of ED visits according to the Manchester triage classification.12 The STROBE Statement was used to report the results.
The research was conducted according to the principles of the World Medical Association Declaration of Helsinki and was approved by CHULN Ethics Committee (No. 176/22).
Data analysisPatients’ characteristics were obtained from the electronic record and included in an anonymized database. SPSS Statistics software version 23.0 (IBM, Armonk, NY) was used. Data is presented in frequencies for categorical variables, mean ± standard deviation (SD) for continuous variables with a normal distribution and median (interquartile range (IQR) = Q3-Q1) for data with non-normal distribution. The Chi-Square statistic or Fisher's exact test were performed to measure the association of categorical or dichotomous variables, respectively. Depending on whether the sample distribution was normal or not, the Pearson or Spearman correlation was used for continuous variables. Comparison between groups with normal distribution was performed using Student's t-test and non-parametric tests (Mann-Whitney) when a non-normal distribution was present. To identify factors associated with mortality, a binary logistic regression was used. All variables whose bivariate analysis (Odds Ratio, OR) revealed statistical interest were included in a multifactorial analysis. A logistic regression model was created to predict mortality in the period from the first ED visit until the end of follow-up. The Kaplan-Meier curve was used to conduct survival analysis. The follow-up time was defined as the first ED visit in 2019 until December 31, 2020 or death.
ResultsDuring 2019, 128,588 adult individuals visited the ED, accounting for 186,344 ED visits. Over 5567 (4.3%) patients were identified as FU, and 174 (0.14%) as ED-FU with pulmonary disease as the main clinical condition, who accounted for 1030 ED visits. These patients had a median (IQR) of 5(3) ED visits, ranging between 4 and 41. Sixty-five patients were admitted to the ED more than 5 times. One patient had 40 visits reporting respiratory symptoms.
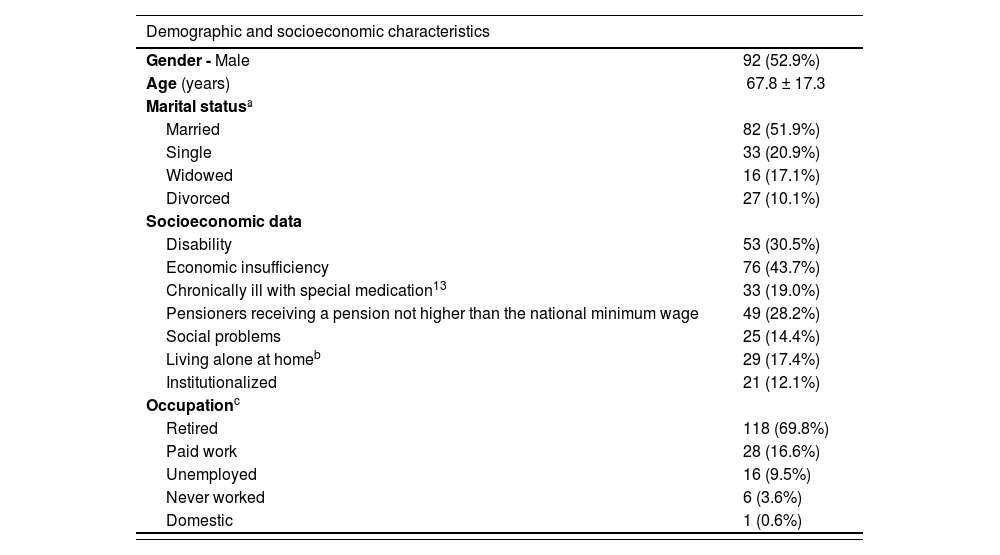
Demographic and socioeconomic characteristicsThe general characteristics related to demographic, socioeconomic and health care factors are listed in Table 1. The mean age was 67.8 ± 17.3 years, with 52.9% males. Most of the patients were retired (69.8%). Over 40.2% had autonomy deficits and 14.4% were registered as social cases. These patients had a median (IQR) of 7(4) visits to the ED compared to 5(2) without social issues (p = 0,004). Disability was reported in 30.5% and 43.7% had financial insufficiency. Although there were fewer unmarried patients (single, widowed and divorced) than married patients (48.1% vs. 51.9%), they generated a higher rate of ED visits compared to married patients (6.8 ± 4.9 vs. 5.3 ± 1.9, p = 0.013).
Demographic, socioeconomic, health care and clinical characteristics of ED-FU with pulmonary disease.
| Demographic and socioeconomic characteristics | |
|---|---|
| Gender - Male | 92 (52.9%) |
| Age (years) | 67.8 ± 17.3 |
| Marital statusª | |
| Married | 82 (51.9%) |
| Single | 33 (20.9%) |
| Widowed | 16 (17.1%) |
| Divorced | 27 (10.1%) |
| Socioeconomic data | |
| Disability | 53 (30.5%) |
| Economic insufficiency | 76 (43.7%) |
| Chronically ill with special medication13 | 33 (19.0%) |
| Pensioners receiving a pension not higher than the national minimum wage | 49 (28.2%) |
| Social problems | 25 (14.4%) |
| Living alone at homeb | 29 (17.4%) |
| Institutionalized | 21 (12.1%) |
| Occupationc | |
| Retired | 118 (69.8%) |
| Paid work | 28 (16.6%) |
| Unemployed | 16 (9.5%) |
| Never worked | 6 (3.6%) |
| Domestic | 1 (0.6%) |
| Clinical characteristics | |
|---|---|
| Smoking habits ≥ 10 pack-year | 90 (52.6%) |
| Current smokersd | 40 (23.1%) |
| Respiratory diseases | |
| COPD | 84 (48.3%) |
| Chronic respiratory failure | 78 (44.8%) |
| Bronchiectasis | 28 (16.1%) |
| Asthma | 28 (16.1%) |
| Diffuse interstitial lung disease | 13 (7.5%) |
| Other diseases | |
| Arterial hypertension | 107 (61.5%) |
| Heart failure | 66 (37.9%) |
| Diabetes mellitus | 48 (27.6%) |
| Advanced cancer disease (including lung cancer) | 46 (26.4%) |
| Neurological disorders | 42 (24.1%) |
| Psychiatric disease | 37 (21.3%) |
| Chronic kidney disease | 29 (16.7%) |
| Number of comorbidities per patient | 6.6 ± 3.4 |
| Charlson Comorbidity Index | 6.1 ± 3.6 |
| Autonomy deficit | 70 (40.2%) |
| Clinical Frailty Salee | |
| Very fit/well | 2 (1.2%) |
| Managing well | 15 (8.6%) |
| Vulnerable | 70 (40.5%) |
| Mildly frail | 14 (8.1%) |
| Moderately frail | 24 (13.9%) |
| Severely frail | 35 (20.2%) |
| Very severely frail | 9 (5.2%) |
| Terminally ill | 4 (2.3%) |
Legend: COPD – Chronic obstructive pulmonary disease; Results are presented as number (percentage) or mean ± standard deviation for variables with normal distribution.
ªMissing information: n = 16.
Fifty-nine patients (33,9%) had no family physician assigned. Using the Manchester triage system, 21.3% of emergency episodes were categorized as “routine” (“green” - 20.4%) or “non-urgent” (“blue” - 0.9%). ED-FU with pulmonary disease generated 432 hospitalizations for different causes in 2019, corresponding to 41.9% of ED visits, with an average of 3.1 ± 1.7 hospitalizations per patient.
Clinical factorsThe clinical characteristics of ED-FU with pulmonary disease are listed in Table 1. Ninety patients (52.6%) had a history of smoking and the vast majority did not have a history of alcohol and/or drug addiction. Applying the CFS, 90.2% of patients were classified as "Vulnerable" to “Terminally ill.”
Regarding pulmonary diseases, COPD was the most frequent respiratory disease (48.3%), followed by 44.8% with chronic respiratory failure, 16.1% with asthma and with various pathologies overlapping. Patients with asthma were younger than other patients (56.8 ± 20.0 vs. 69.9 ± 15.9, p<0.001).
Most patients had a considerable number of comorbidities, with a mean of 6.6 ± 3.4, and 82.0% had 4 or more comorbidities.
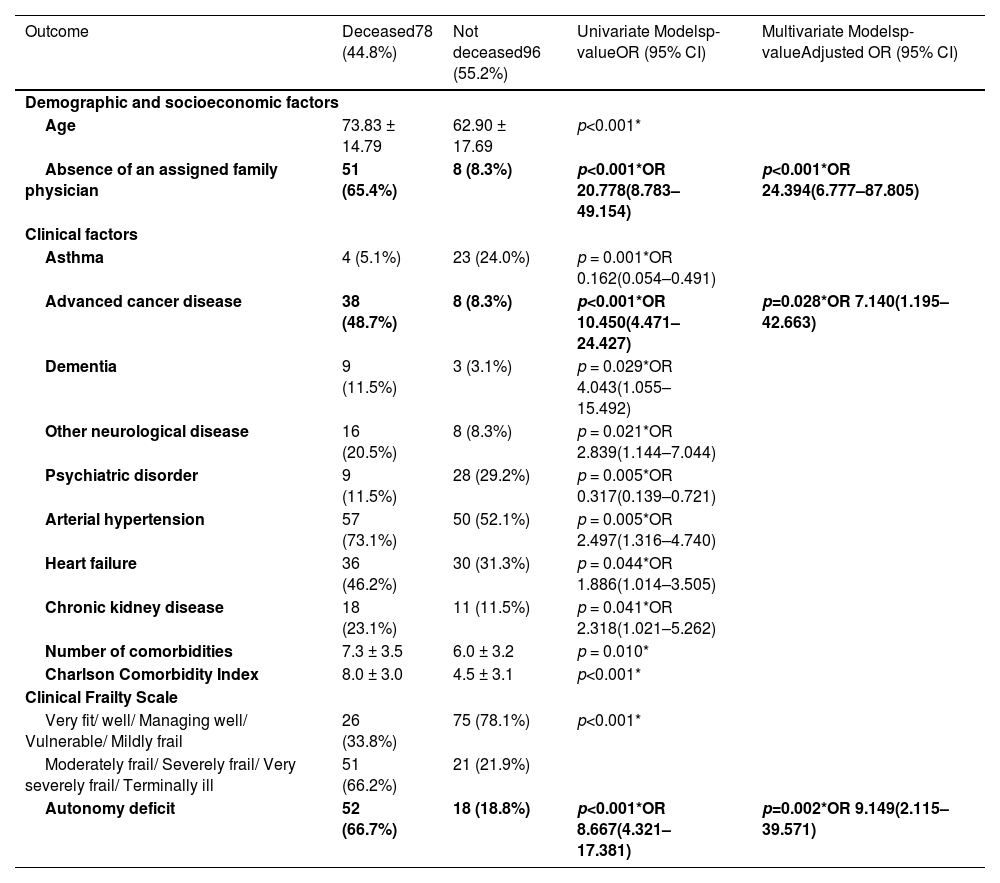
MortalityDuring the follow-up period (mean 15.7 ± 7.1 months), 78 (44.8%) patients died: 45 during 2019 (25.9%) and 33 during 2020 (25.6%). A specific analysis of this population (Table 2) showed that most patients who died were male (56.4%), retired (82.9%) and older (p<0.001). Regarding the CFS, 66.2% of individuals who died were “Moderately frail to terminally ill” patients, the vast majority (54.2%) of survivors were “Vulnerable.” The mean number of comorbidities in patients who died was higher (7.3 ± 3.5 vs. 6.0 ± 3.2, p = 0.010), the same for CCI (8.0 ± 3.0 vs. 4.5 ± 3.1, p<0.001). Of the 59 patients without a family physician, 86.4% (n = 51) died during the analysis period (< 2 years).
Characteristics of ED-FU according to the outcome during the follow-up and risk factors for mortality.
Legend: OR – Odds ratio, CI – Confidence Interval. *OR was calculated when p<0.05. Results are presented as number (percentage), mean ± standard deviation for variables with normal distribution.
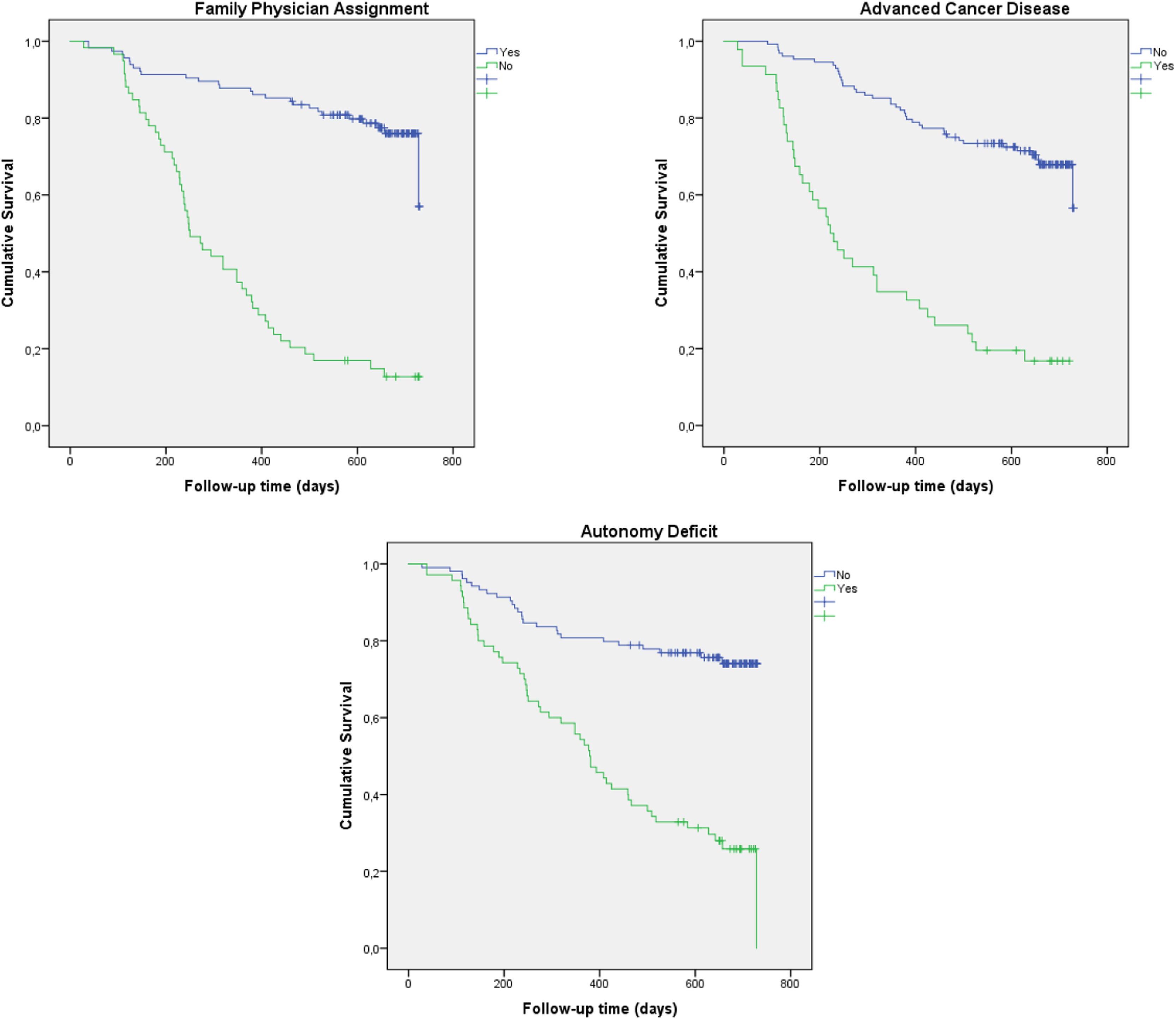
Table 2 shows the OR for mortality before and after adjustment for age, number of comorbidities and CCI. The multiple logistic regression model identified the absence of an assigned family physician, the autonomy deficit and advanced cancer disease as the main factors associated with mortality. The Kaplan-Meier survival curve for assigned family physician, advanced cancer disease and autonomy deficit showed a different survival profile with the earliest mortality in patients with advanced cancer disease (Fig. 2).
DiscussionWe evaluated 5567 ED-FU at one of the largest university hospitals in the country and we found that, despite generating a high number of episodes of urgency, only a small percentage of patients (3.1%; n = 174) affected by respiratory disease as the main clinical condition required hospitalization under pulmonology department accountability. To the best of our knowledge, this is the first national study to evaluate the profile of ED-FU with pulmonary disease and its impact on mortality.
The main finding was that a high proportion (33.9%) of pulmonary ED-FU did not have a family physician assigned in the PHC setting, and this was the most important factor associated with mortality. Pulmonary ED-FU were characterized by a high burden of chronic disease and disability. Advanced cancer disease and autonomy deficit were the other factors that most determined the prognosis.
An unexpected finding of our investigation was the relatively small number of patients with pulmonary disease as the main clinical condition and hospitalization (3.1%) in the group of ED-FU. A possible explanation may be related to a high and diversified care load for respiratory patients provided by our hospital center.14 However, this assumption needs to be supported by other studies comparing patient profiles and diagnosis within other national hospital institutions.
The profile of pulmonary ED-FU presented some predominant characteristics, such as a high mean age (67.8 years), male gender, social and economic vulnerability, high burden of chronic diseases and comorbidities, with a significant degree of disability and dependency. These clinical features were objectified by a high CCI (6.1 ± 3.6) with a high degree of “vulnerability” (40.5%) or “frailty” (49.7%) in the CFS. These results are in line with other series that report FU with more complaints and high prevalence of chronic diseases leading to increased use and high rates of hospitalization and mortality.15–17 COPD was the most frequent respiratory disease (48.6%), which is in agreement with national and international epidemiological data.18–22 There was a significant percentage of patients diagnosed with chronic respiratory failure (44.8%) and asthma (16.1%). Further, psychiatric disease was frequent (21.3%). A published analysis corroborates our finding that ED-FU were not simply inadequate consumers of ED resources, but were also associated with more mental health diseases and high prevalence of chronic diseases.15,23–25 The identification of social and economic vulnerability (43.7%) in our study is also supported by other studies.26–28
The analysis of the Manchester triage classification of emergency visits reflects a certain heterogeneity in these FU with pulmonary disease. Most ED episodes (77.6%) were classified as “immediate”, “very urgent” or “urgent” which may correspond to patients’ vulnerability and high burden of the disease. These contrast with 21.3% of emergency episodes categorized as “routine” or “non-urgent”, indicating that emergency services have become alternative care. According to more recent national estimates, 31% of ED visits in Portugal are “non-urgent”, “inappropriate” or “avoidable.”2 However, our finding of a much lower frequency of “routine” and “non-urgent” ED episodes (21.3%) points to a high burden of disease in ED-FU with pulmonary disease.
During the follow-up period, there was found to be a high mortality rate (44.8%). This finding supports the conclusion that the ED visit per se should not be seen as an adverse outcome and might be better perceived as a marker of the true need for health care.29 After applying the multivariate logistic regression analysis, with adjustment for age and comorbidities, we found that lack of assignment of a family physician, autonomy deficits and advanced cancer disease were associated with an increase of 24.4, 9.1 and 7.1 times in the risk of death, respectively. The identification of these three ED-FU profiles provides useful information for the development of tailored interventions that would address the specific needs of each type of ED-FU, e.g., patients with advanced cancer disease should be referred early to palliative care, avoiding multiple emergency visits.
In Portugal, the absence of an assigned family physician is a problem, in particular in the Lisbon region.30 Associated factors are the high number of retired people and a reduced capacity for generational renewal associated with low attractiveness of the general and family medicine specialty in the NHS.31 The lack of assignment of a family physician in this population of pulmonary ED-FU (33.9%) is a highly relevant factor, considering its very high mortality (86.4%). Moreover, the frequency of absence of a family physician was much higher than the national average of 7.3%, in 2019.1 Thus, frequent demand for emergency services may indicate barriers to the use of the health care network, as well as vulnerability and illness of people who repeatedly need care, with an impact on mortality.32 On the other hand, the association between mortality and high use of EDs by advanced cancer disease patients may reflect end-of-life episodes and point to a lack of palliative care services. Similarly, the autonomy deficit associated with multiple ED visits and mortality may also reflect the absence of structures that offer adequate health care to people with end-stage lung disease. These results reinforce the fact that articulation and integration of special levels of care, such as palliative and long-term care, with PHC and hospitals are relevant to ensure that these patients receive appropriate care.33–35 Home-care hospitalization (HCH) is also important in patients with end-stage disease.36,37 Despite the good development of HCH in our country, with 9 units in the Lisbon region, the number of available beds is still not sufficient.38,39
The integration of PHC and hospitals can be achieved through the creation of collaborative networks between the teams, allowing for the easier management of identified needs.
Study limitationsThis study has some limitations that must be addressed, primarily the fact that it is a monocentric study not allowing nationwide insight. However, our hospital center is one of the biggest university hospitals in the country, covering a wide geographical area, and serving individuals from various socioeconomic strata, mostly from urban and suburban areas. The number of people living in remote areas was not addressed or excluded directly. Another limitation relates to the retrospective nature of the study and the incomplete information present in the ED's electronic clinical records, which may have underestimated some factors associated with FU, such as psychiatric disorders, toxic habits, or social issues. Further, we cannot accurately estimate the effect of the pandemic on mortality during the follow up. Although the percentage of deaths was similar in 2019 (25.9%) and 2020 (25.6%), the causes of death in both years were not analyzed due to the absence of this information, whenever the death occurred outside our institution. The lack of a comparator group is another limitation. Details about hospital stays (type, length and severity) were not collected, and constitute another limitation that may be an issue for future investigation.
ConclusionsPulmonary ED-FU are a small group of ED-FU comprising an aged and heterogeneous group, with a high burden of chronic disease and disability. The lack of assignment of a family physician in primary care setting was the most important factor associated with mortality. The clinical factors related to prognosis were advanced cancer disease and autonomy deficit. These findings support not only the urgent need to increase accessibility to a primary care physician, but also to domiciliary hospitalization, palliative care and long-term care across national health pathways.