Pulmonary rehabilitation (PR) has proved a valuable1 and cost effective2 tool for the treatment of chronic respiratory diseases and its benefits have been increasingly recognized by the medical community. However, it is often underutilized for a multitude of reasons such as inaccessibility, limited local offer and poor knowledge of how to refer.3–5
To this end, strategies have been developed to extend PR to primary care (PC) as a way of reaching a larger number of patients who may benefit from this therapeutic approach6. In Portugal, this issue was recently addressed by National Health authorities and the extension of PR to PC is supposed to be ongoing until the end of 2017 (Despacho n.° 6300/2016, Diário da República, 2.ª série N.° 92 – 12 de maio de 2016).
However, before embarking on such a strategy, the authors believe that a more precise assessment of the current state of PR at PC is needed. With this in mind, taking advantage of the organizational model of our Local Health Unit which groups a General Hospital (in which we develop our hospital-based pulmonary rehabilitation program – PRP) and 14 PC units under the same shared administrative board, we conducted an anonymous survey among all PC specialists and residents to ascertain their knowledge about indications, benefits, available resources and hindrances to the referral of patients to PR.
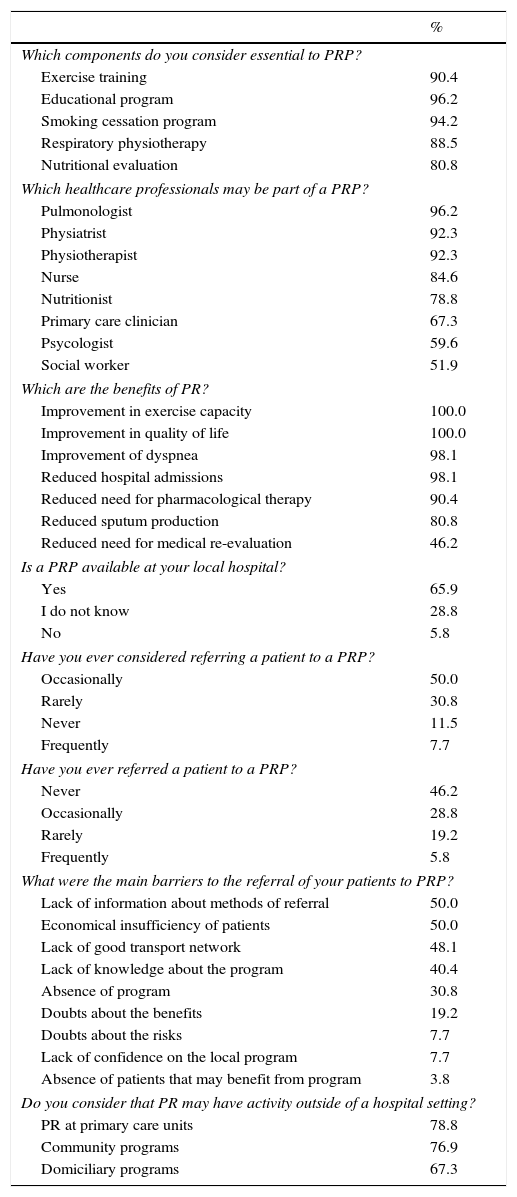
From a population of 108 PC physicians, we obtained 52 answers (48.1%) to our enquiry (Table 1). Most (55.8%) clinicians had over 30 years of clinical practice and followed between 50 and 100 patients with chronic respiratory diseases, of which COPD was clearly the most prevalent (84.6%) and the one more frequently considered as candidate for PRP (98.1%). Some benefits of PR were recognized, namely the improvement in exercise performance, quality of life and of degree of dyspnea. Most PC physicians (67.3%) were eager to actively participate in PR, despite the fact that more than a third of the physicians did not know that their local hospital had a PRP. Those who knew, sometimes thought about referring their patients, but only rarely actually did so. When asked why, they mentioned the lack of information regarding the means of referral and economic and transportation difficulties as the main hindrances. Risk concerns were exceedingly low (mentioned only by 7.7% of our respondents).
Pulmonary rehabilitation and primary care (n=52).
| % | |
|---|---|
| Which components do you consider essential to PRP? | |
| Exercise training | 90.4 |
| Educational program | 96.2 |
| Smoking cessation program | 94.2 |
| Respiratory physiotherapy | 88.5 |
| Nutritional evaluation | 80.8 |
| Which healthcare professionals may be part of a PRP? | |
| Pulmonologist | 96.2 |
| Physiatrist | 92.3 |
| Physiotherapist | 92.3 |
| Nurse | 84.6 |
| Nutritionist | 78.8 |
| Primary care clinician | 67.3 |
| Psycologist | 59.6 |
| Social worker | 51.9 |
| Which are the benefits of PR? | |
| Improvement in exercise capacity | 100.0 |
| Improvement in quality of life | 100.0 |
| Improvement of dyspnea | 98.1 |
| Reduced hospital admissions | 98.1 |
| Reduced need for pharmacological therapy | 90.4 |
| Reduced sputum production | 80.8 |
| Reduced need for medical re-evaluation | 46.2 |
| Is a PRP available at your local hospital? | |
| Yes | 65.9 |
| I do not know | 28.8 |
| No | 5.8 |
| Have you ever considered referring a patient to a PRP? | |
| Occasionally | 50.0 |
| Rarely | 30.8 |
| Never | 11.5 |
| Frequently | 7.7 |
| Have you ever referred a patient to a PRP? | |
| Never | 46.2 |
| Occasionally | 28.8 |
| Rarely | 19.2 |
| Frequently | 5.8 |
| What were the main barriers to the referral of your patients to PRP? | |
| Lack of information about methods of referral | 50.0 |
| Economical insufficiency of patients | 50.0 |
| Lack of good transport network | 48.1 |
| Lack of knowledge about the program | 40.4 |
| Absence of program | 30.8 |
| Doubts about the benefits | 19.2 |
| Doubts about the risks | 7.7 |
| Lack of confidence on the local program | 7.7 |
| Absence of patients that may benefit from program | 3.8 |
| Do you consider that PR may have activity outside of a hospital setting? | |
| PR at primary care units | 78.8 |
| Community programs | 76.9 |
| Domiciliary programs | 67.3 |
The majority (78.8%) had never received training in PR, but were open to having it in the future.
These results impart a few important messages. Number one, PRPs – namely hospital-based PRPs such as ours need to be better advertised within our local medical communities so as to be considered as a real therapeutic opportunity for patients that sometimes remain only in PC. Number two, a clear and unobstructed method of communication between hospital based PRP and PC should be created to remove the referral obstacles and also to allow a correct identification of patients who would be good candidates for the different settings of PR. Not all patients can be managed at PC based PR; this depends mainly upon precise risk stratification that perhaps needs to be further debated. Number three – training is the key! PC specialists and residents should be offered specific training in PR (which they are apparently keen to obtain) and this training should ideally take place before they are asked to take an active part in prescribing PR. This would probably help to facilitate communication, surpass referral barriers and correctly allocate patients to the different settings of PR.
Despite the fact that our results may only reflect a local perspective and that regional asymmetries may exist, we believe further investigation (perhaps a national survey) should be conducted to assure that PC physicians are fully prepared to take on the challenge demanded of them, that of receiving PR in their particular contexts by the end of 2017.
Authors’ contributionsGonçalo Samouco and Luís Vaz Rodrigues conceived the idea, developed the initial draft of the survey and wrote the manuscript. Margarida Maurício, Luis Ferreira, Vitória Martins and Inês Sanches reviewed and suggested improvements upon the initial draft. Gonçalo Samouco, Luís Vaz Rodrigues and Margarida Maurício collected and analyzed the data from the survey. All authors have read and approved the final version.
Conflict of interestThe authors have no conflict of interest to declare.