Adherence to medication is a complex phenomenon that may vary in form and intentionality. In COPD, as in many chronic diseases, poor adherence behaviors are a well-known factor of therapeutic failure.1 The patients’ understanding of their disease and therapy are constructs based on social and cultural factors,2 and health-related beliefs will influence the patient adherence to therapy. In the evaluation of adherence, self-reported questionnaires are currently the most widely used tools.3 The 7 items Measure of Treatment Adherence (MTA) is a validated tool for studying the adherence to medication,4 and the Beliefs about Medicines Questionnaire (BMQ) is useful for exploring the relationship between beliefs and adherence.5,6 However, to understand this complex and subjective phenomena, qualitative methods have also been used in production of knowledge,7,8 complementing quantitative studies. We present the preliminary results of an ongoing study aimed at understanding the patterns and reasons for non-adherence and how the patients’ representation of COPD influence adherence to inhaled medication.
Participants over 40 years old diagnosed as suffering from COPD according to GOLD criteria were included. The MTA, the BMQ, and a demographic, socioeconomic, clinical and an easy-to-answer survey on COPD were used. After completion of the questionnaires, semi-structured interviews were carried out. Participants were encouraged to justify their opinions and behaviors, according to Grounded Theory qualitative methodology. The objective was to obtain new information from patients themselves. Field-notes were made during the interview, and each interview was analyzed before the next one. A quantitative and qualitative analysis of the variables was then performed.
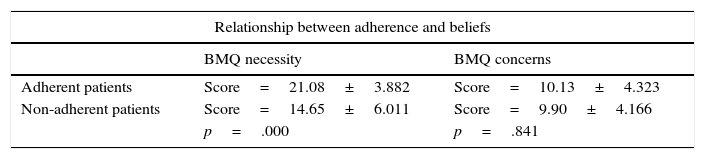
Of the 174 participants (mean age=67.8 years), 78.2% were males, the majority (85.1%) living in predominantly urban spaces, 85% were of low educational level (≤4 years of school) and 66.1% low income (≤530 €). The mean FEV1 was 52.1%±19% and 36.7% of patients mentioned ≥2 exacerbations in the previous year. A total of 163 participants completed the MTA questionnaire: 50 referred to one or more poorly adherent behaviors, but only 25 (15.3%) were considered non-adherent. The relationship between adherence, beliefs about medication, and GOLD stage and classification is shown in Table 1. Some participants reported forgetting to take the medication, carelessness with schedules or letting the medication run out. Others reported complete withdrawal, usually for economic reasons. Other patterns of non-adherence were, when less symptomatic, suspension of all medication, reduction in the number of inhalations, suppression of one dose, usually at night, use of the medication only in exacerbations, and suppression of one of the inhalers. In case of worsening of symptoms, the two patterns of incorrect adherence were the increased frequency of the number of inhalations and anticipation of the schedule of prescribed inhalations. The reasons for non-adherence were: use according to need, economic reasons, confusion or misunderstanding of therapy, fear of side effects, and dependence on others. Only 4 patients experienced unpleasant side effects of medication. There were 4 domains of poor adherence: health-related experiences, economic, behavioral, and health-related beliefs. The reasons given for good adherence behaviors were discipline in medication compliance, daily routines, having a caregiver, the use of rapid relief medication, confidence in the physician or in the medication, having reserve medications, previous negative experiences and ease of medication acquisition. We found 3 domains of good adherence: health-related behaviors, health-related experiences and health-related beliefs. The majority of participants recognized COPD as a chronic disease and a serious illness (88.6% and 78.6%, respectively). Some justified the severity because of their symptoms (41.3%) or limitations (22.4%), being incurable (7.7%) and because of recreational limitations (3.4%). Paradoxically, only 4 participants mentioned fear of dying. However, only 11.7% of patients referred to the disease by its correct name, 41% attributed other names to it, 15.5% did not know what they were suffering, 16.6% referred not to the disease but to the affected organ or function, 12.3% to symptoms, and 3% to its etiology.
Adherence to inhaled medication.
| Relationship between adherence and beliefs | ||
|---|---|---|
| BMQ necessity | BMQ concerns | |
| Adherent patients | Score=21.08±3.882 | Score=10.13±4.323 |
| Non-adherent patients | Score=14.65±6.011 | Score=9.90±4.166 |
| p=.000 | p=.841 | |
| Relationship between adherence and GOLD 2016 stage and classification | ||||
|---|---|---|---|---|
| GOLD | ||||
| I | II | III | IV | |
| Patients (%) | 8.6 | 40.8 | 35.6 | 15 |
| Non-adherent (%) (p=.039) | 25 | 23 | 9.8 | 4 |
| GOLD | ||||
|---|---|---|---|---|
| A | B | C | D | |
| Patients (%) | 15.5 | 22.4 | 9.8 | 52.3 |
| Non-adherent (%) (p=.025) | 40 | 16.2 | 11.7 | 10.1 |
COPD is represented by patients as a chronic and severe disease, since it is symptomatic and limiting. Fear of hospitalization or death was not valued by the participants in this study. In many chronic diseases, non-adherence appears to depend on the balance between perceived necessity and specific medication concern, but in our survey only necessity beliefs are associated with adherence. Compliance is also related with the clinical and functional severity of the disease. In fact, the evaluation of treatment necessity is based in the perception of the necessity. Concerns about inhaled medication are not related to side-effects, and do not appear to significantly affect adherence. MTA was chosen because it is validated by the Portuguese population. However is not specific for inhaler devices nor to COPD, and when compared to the Test of Adherence to Inhalers9 or the Morisky Medication Adherence Scale,10 may not be able to capture some patterns of non-adherence. This may, to some degree, justify the low level of non-adherence. However, recently published studies reported variability in the prevalence of poor adherence, when using different methods or instruments, and different populations.11
New information obtained was related to the patterns and reasons for non-adherence, and to behavior actions that reinforce compliance. The more important practical differences between patient and doctor cultural perception about the treatment lies in its usefulness in prevention of exacerbations and disease progression.
Conflicts of interestThe authors have no conflicts of interest to declare.