The search for physiological indexes which are capable of reproducing predictable success of weaning has not yet produced satisfactory results.1–3 Recognition of the exact time of return to spontaneous ventilation is essential for better prognosis, reducing costs and mortality.1,2
In the past, a large number of predictive physiological indicators of successful discontinuation of ventilation support have been developed. These indicators have great sensitivity, but lac specificity, so some patients have had to go back on ventilation assistance, which increases unsuccessful weaning rates.1–3
The Rapid Shallow Breathing Index(RSBI) is the most reliable calculation for predicting weaning success. Alteration in patient voluntary breathing patterns, making it superficial, fast and fatiguing without the aid of ventilatory support will bring RSBI's values above 105, therefore indicating failure to wean and not indicating discontinuation of mechanical ventilation.4
Capnography is a registration or graphic visualization of the variation of carbon dioxide (CO2) in the respiratory cycle performed through a sensor that directly measures the gas concentration. Initially in each expiratory cycle, CO2 pressure (PCO2) is zero. Afterwards, during expiration, alveolar gas elimination begins, increasing PCO2 values, stabilizing and reaching a plateau. At the end of the exhalation a fall occurs, indicating the beginning of inspiration. The monitor reports CO2 end-expiratory pressure (PET(CO2)) and the waveform.3,5,6 We expected that abnormal capnography and increased PET (CO2) would relate with mechanical ventilation weaning failure.6 As there are no studies which show the capnography relevance like physiological predict index, the overall study objective is to identify the relationship between RSBI and capnography with successful withdrawal from artificial ventilatory support.
After being approved by Ethics Committee from UCPel (200884), a cross-sectional study was carried out at the ICU of University Hospital, Pelotas, Brazil.
Patients who had been less than 48hours on mechanical ventilation and had entered a weaning protocol were excluded. Fifteen patients (11 males) had 20 attempts at weaning and participated in this study. The sample was calculated considering a power of 80% and a difference of 30bpm/L in the RSBI averages in the success and failure groups. The indication of mechanical ventilation were acute respiratory failure and comorbidities: two were in cases of stroke, two were enterectomy postoperatives, four of pneumonia, two cases of chronic obstructive pulmonary disease (COPD), two COPD associated with pneumonia, one case of acute renal insufficiency, one postoperative of gut surgery and one case of acute respiratory distress syndrome. The weaning process followed the recommendations of the III Brazilian Consensus of Mechanical Ventilation.1 The criteria for weaning failure were: RR>35bpm, oxygen saturation<90%, HR>140bpm, SBP>140 or <90mmHg and signs of agitation or alteration of consciousness levels.1
The weaning indexes evaluated were capnography and RSBI. RSBI is obtained in the first (RSBI1’) and 30th minute (RSBI30’) of mechanical ventilation disconnection. Sensitivity and specificity of RSBI were also evaluated.
For the PET(CO2) and the capnography, a capnograph sensor was placed between the orotracheal/tracheostomy tube and the T-tube, which was connected to the Dash® 4000 monitor. Capnography and PET(CO2) values were recorded in six breath cycles at five minute intervals up to the total of 30minutes.
Based on the capnography waves presented by Díez-Picazo,5 the graphics collected were described as normal or altered. Two or more consecutive waves were the criterion to define an altered capnography.
The sample consisted of 15 patients with 20 mechanical ventilation weaning attempts, of which 13(65%) were successful, and 7(35%) were unsuccessful in the process.
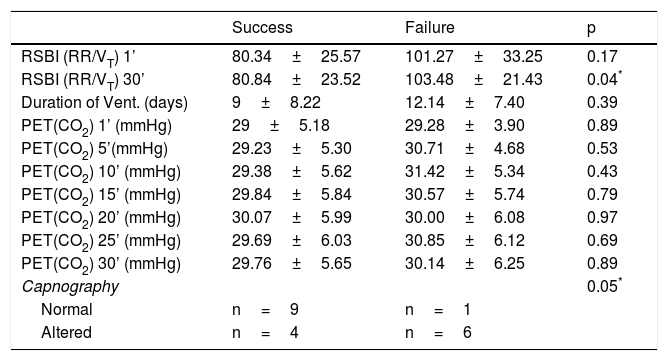
The Weaning success group had lower values in the RSBI30’ than the failure group as well as more waves considered normal on capnography(p ≥ 0.05). While variables not related to the success of weaning were: RSBI in the first minute (RSBI1’), duration of mechanical ventilation, PET(CO2)1’, PET(CO2)5’, PET(CO2)10’, PET(CO2)15’, PET(CO2)20’, PET(CO2)25’ and PET(CO2)30’(Table 1).
Comparison between success group and failure group in Weaning.
| Success | Failure | p | |
|---|---|---|---|
| RSBI (RR/VT) 1’ | 80.34±25.57 | 101.27±33.25 | 0.17 |
| RSBI (RR/VT) 30’ | 80.84±23.52 | 103.48±21.43 | 0.04* |
| Duration of Vent. (days) | 9±8.22 | 12.14±7.40 | 0.39 |
| PET(CO2) 1’ (mmHg) | 29±5.18 | 29.28±3.90 | 0.89 |
| PET(CO2) 5’(mmHg) | 29.23±5.30 | 30.71±4.68 | 0.53 |
| PET(CO2) 10’ (mmHg) | 29.38±5.62 | 31.42±5.34 | 0.43 |
| PET(CO2) 15’ (mmHg) | 29.84±5.84 | 30.57±5.74 | 0.79 |
| PET(CO2) 20’ (mmHg) | 30.07±5.99 | 30.00±6.08 | 0.97 |
| PET(CO2) 25’ (mmHg) | 29.69±6.03 | 30.85±6.12 | 0.69 |
| PET(CO2) 30’ (mmHg) | 29.76±5.65 | 30.14±6.25 | 0.89 |
| Capnography | 0.05* | ||
| Normal | n=9 | n=1 | |
| Altered | n=4 | n=6 |
RSBI: Rapid Shallow Breathing Index; RR: respiratory rate; VT: tidal volume; PET(CO2): CO2 end-expiratory pressure; ‘:minute. Results are presented as means±standard deviation.
Taking into account capnography, the success group had nine normal and four altered capnography waves, while the failure group had one normal and six altered capnography (p=0.05).
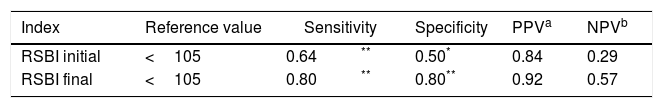
The RSBI1’ showed regular sensitivity (0.64), low specificity(0.50), positive predictive value of 0.84 and negative predictive value of 0.29, with an accuracy of 65%.
The RSBI30’ showed better results, with regular sensitivity (0.80), regular specificity (0.80), positive predictive value of 0.92 and negative predictive value of 0.57, with an accuracy of 80%(Table 2).
The main finding of this study was the association of weaning success with RSBI at 30th minute (RSBI30’) and with the capnography.
The RSBI is the most specific index for predicting success at weaning.4,7 Despite a good indicator, studies suggest that the RSBI performed in the first two minutes of disconnection cannot predict success or failure at weaning.2
In the literature, Lee,2 presented specificity values of 0.72 and sensitivity of 0.11. Yang & Tobin,4 presented of 0.64 for specificity and 0,97 for sensitivity. We observed the specificity of 0.50 in RSBI1’ and 0.80 in RSBI30’, and sensitivity of RSBI1’ of 0.64 and RSBI30’ of 0.80, showing better indicators after 30minutes of evaluation compared to the first minute.
Our study shows that PET(CO2) was not a factor associated with weaning, and that RSBI was related as a predictor after the 30th minute, showing better sensitivity and specificity. In addition, we verified that the analysis of the graphics of capnography can be effective and collaborate in the evaluation of the patient to weaning process.
The limitations of this study are the small sample size and the fact that the analysis of capnography, although done by the same evaluators to maintain parameters, was performed subjectively,5 being limited to the graphic of normal/altered.
Ethics approvalThe Human Research Ethics Committee from Catholic University of Pelotas approved this study under number 200884.
Author statementI affirm that all authors have read and agreed the Statement for Authors.[91]
Conflict of InterestNone.
- Home
- All contents
- About the journal
- Metrics
- Open access