Tuberculosis (TB) is an example of a long-standing epidemic: it has evolved over more than 2000 years and is the ninth leading cause of death worldwide and the leading cause of infectious disease.1 Homelessness is widely acknowledged as a TB risk factor: in fact, the need to address the most vulnerable and hard-to-reach groups – among which the homeless are listed – has been recently highlighted in an action framework aiming at the elimination of TB in low-incidence countries.2 In Portugal, data from 2011 shows that TB incidence among homeless was five times higher than within the general population.3 This study intended to identify socio-demographic and health-related variables in the general population and among TB patients that are associated with TB incidence in the homeless population.
This was a retrospective study focused on a seven-year period (2008–2014) and on the 18 districts of mainland Portugal. Information regarding TB incidence and patients’ characteristics, such as homelessness status (defined as someone living in the streets with no shelter or lacking a fixed address), HIV co-infection, foreign-born, alcohol abuse (based on subjective information – CAGE questionnaire4) and illicit drug abuse (considered if there are withdrawal or tolerance symptoms, not including occasional consumption) was extracted from the Portuguese TB surveillance system (SVIG-TB). Socio-demographic and health-related data, such as total population, population density, working age population (aged 15–64 years), elderly population (aged ≥65 years), immigrant population, unemployed population, physicians (proportion in the population) and HIV notification rate, were collected from Statistics Portugal, Employment and Vocational Training Institute and National Health Institute Doutor Ricardo Jorge.
The longitudinal effect of the studied variables on the incidence rate of TB among the homeless was estimated by a mixed-effects linear regression model with: (1) a random intercept taking the inter-district variability into account; (2) a residuals variance function depending exponentially on the fitted values.5 Comparison between models was based on the likelihood ratio test for nested models and on the Akaike Information Criteria (AIC) otherwise.6 Statistical analysis was performed with the R language and software environment for statistical computation, version 3.3.2.7
TB incidence rate in mainland Portugal has steadily decreased from 24 cases per 100000 inhabitants in 2008 to 17 cases per 100000 inhabitants in 2014. However, the incidence rate of TB among the homeless has not accompanied the same decreasing trend: it remained approximately stable from 1.2 cases per 100000 inhabitants in 2008 to 0.97 cases per 100000 inhabitants in 2014.
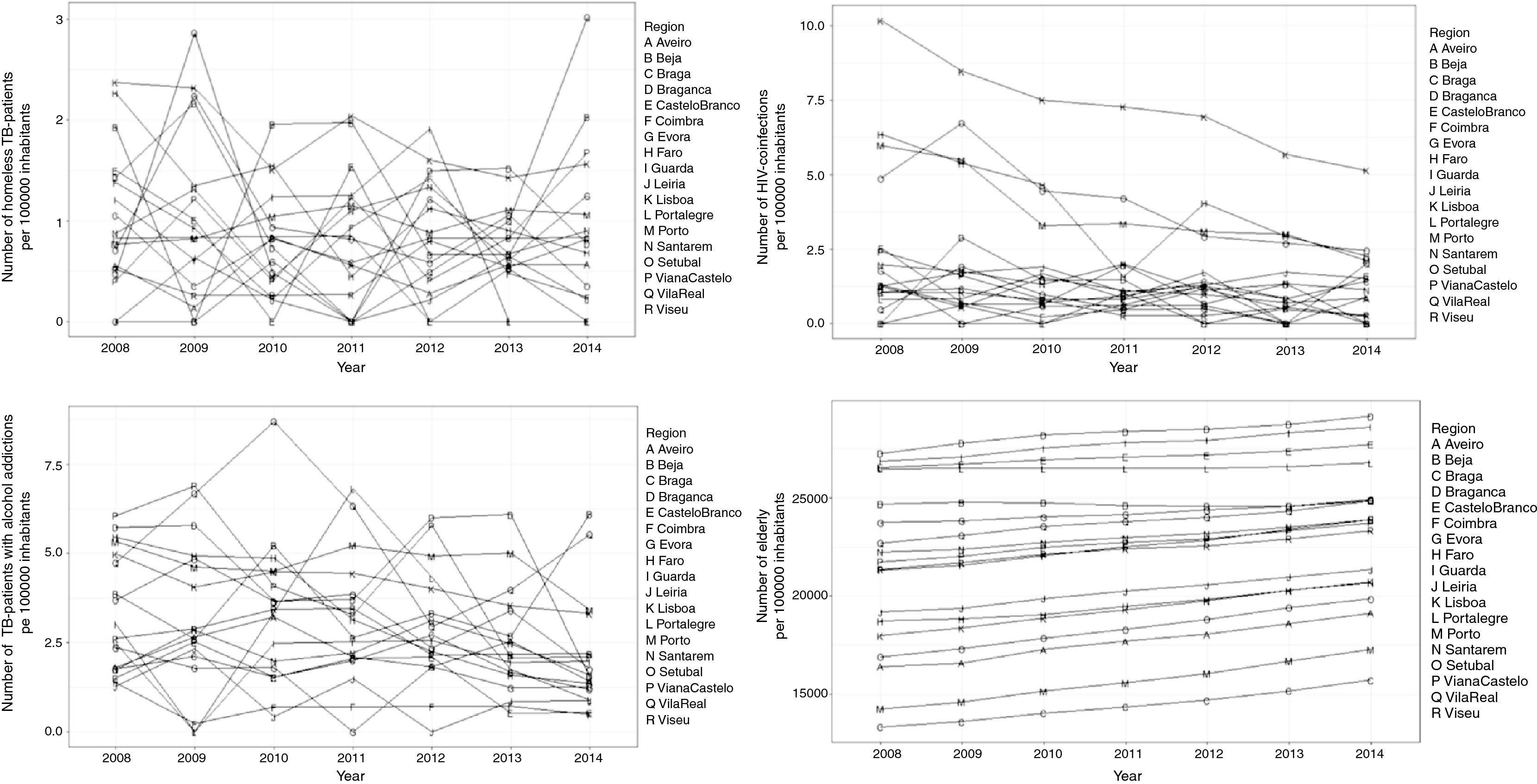
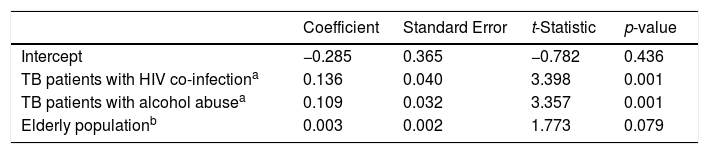
Our results indicate that TB incidence rate among homeless people is associated with HIV co-infection and alcohol abuse among TB patients and the proportion of elderly people in the overall population. Fig. 1 describes the longitudinal evolution of homeless TB patients per 100000 inhabitants per district and the predictors found to be associated. Table 1 describes the results obtained from the fitted regression model: briefly, an increase of 100 HIV co-infected cases or alcohol abusers among TB patients is associated with an increase on the incidence of TB among the homeless by an average of 14 or 11 cases per 100000 population, respectively. The proportion of elderly people has a smaller impact: an increase of 1000 elderly persons in the general population is associated with an increase on the incidence of TB among the homeless by an average of 3 cases per 100000 population.
Estimates obtained from the fitted regression model evaluating the effects of HIV co-infection and alcohol abuse among TB patients, and the proportion of elderly population, in the longitudinal evolution of the TB incidence rate among homeless people. The standard deviation of the random effect was estimated at 0.138 (0.057–0.339) while the power of the variance exponential function was of 0.595 (0.232–0.959).
The relationship between alcohol abuse and TB, as well as between TB and the elderly, has been previously acknowledged.8,9 Moreover, HIV co-infection is universally recognized as the single most important risk factor for TB in regions with a high TB burden.10 Importantly, both alcohol abuse and HIV infection have been previously associated to homeless TB patients.3
Our study has a number of strengths that ought to be highlighted: we collected data from the whole of mainland Portugal for a period of seven years, obtained from several national institutions. On the other hand, a few limitations should also be acknowledged: although TB notification is mandatory, reporting coverage may be particularly low among the homeless, given that this high-risk group may tend to avoid primary care facilities, delaying or preventing a timely TB diagnosis; and finally, as all data was extracted from national databases, we were limited by the degree of completeness and accuracy, as well as by the variables considered, which may have left out important indicators.
Overall, this study allowed us to conclude that preventive interventions targeting HIV co-infected and alcohol abusers among TB patients, as well as the elderly in the general population, may decrease TB incidence rate among homeless people. In fact, although an early diagnosis and effective treatment remains the cornerstone strategy, complementing this approach with preventive measures targeting social determinants and biological risk factors, such as the ones highlighted, may be useful to achieve the target of TB elimination in Portugal and other low-burden countries.
FundingThis work was supported by the contribution of Iceland, Liechtenstein and Norway, through the EEA Grants, under the Public Health Initiatives Programme (PT 06), grant number 138DT1. Olena Oliveira was supported by the project NORTE-08-5369-FSE-000041, financed by the Operational Program Norte 2020 and co-financed by the European Social Fund through a doctoral grant (UMINHO/BD/47/2016). Rita Gaio was partially supported by CMUP (UID/MAT/00144/2013), which is funded by FCT (Portugal) with national (MEC) and European structural funds (FEDER), under the partnership agreement PT2020.
Specific author contributionsAna Luísa Vieira drafted the manuscript, Olena Oliveira and Marta Gomes supported data collection, Rita Gaio provided the statistical analysis, Raquel Duarte conceived and designed the study and all authors revised the manuscript and approved its final version.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ana Luísa Vieira would like to thank Catarina L Santos for medical writing advice.