High-flow nasal cannula (HFNC) therapy is a novel technique of oxygen therapy that delivers heated and humidified oxygen via a special device at a rate of up to 60L/min.1 HFNC has some physiological effects, including a low level of positive airway pressure, reduction of nasopharyngeal resistance, pharyngeal dead space washout, humidification, and better control of mucociliary clearance.2 HFNC has been used as a mode of noninvasive respiratory support for acute hypoxemic respiratory failure without hypercapnea with adults, children, and neonates.3 Recently, the clinical indications of HFNC have been expanded to post-extubated patients under intensive care or following surgery, those undergoing bronchoscopy, and those with the status of “do not intubate”.3 Here, we describe a post-gastrectomy case with chronic lower respiratory tract infection, which was well controlled by domiciliary nocturnal HFNC.
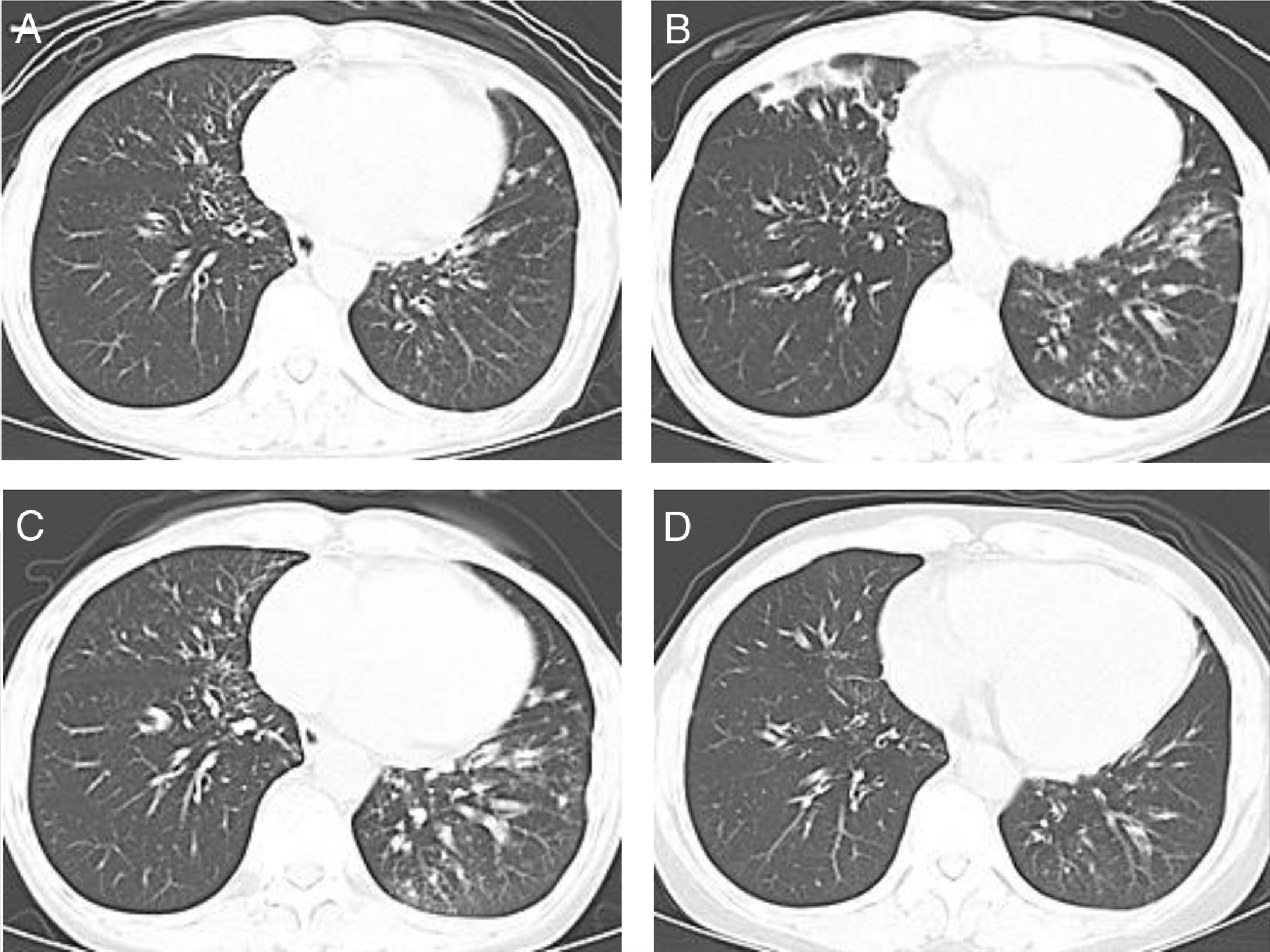
The patient is a 62-year-old, non-smoking, woman who was diagnosed with gastric cancer and was treated by total gastrectomy when she was 60. At the time of diagnosis of gastric cancer, chest computed tomography (CT) revealed mild bronchial wall thickening in both lower lobes (Fig. 1A). Six months after gastrectomy, follow-up chest CT showed consolidation in the right middle lobe and left lingular segment and consolidation, mucus plug, and centrilobular nodules in both lower lobes (Fig. 1B). Therefore, she was referred to the Department of Respiratory Medicine in Hikone Municipal Hospital.
She complained of productive cough without postnasal discharge. She was not on any medication, including proton pomp inhibitors. Laboratory test results revealed white blood cell counts of 5880/μL, C-reactive protein of 0.29mg/dL, and antinuclear antibody titer of 1:40. The % predicted forced vital capacity and % predicted forced expiratory volume in 1s were 2.07L (81.4%) and 1.56L (75.3%), respectively. Sinus CT revealed mild mucosal thickening and opacification of the right ethmoid and sphenoid sinuses and the bilateral maxillary sinuses; Lund–Mackay staging system score was 4. Fiber-optic bronchoscopy revealed purulent bronchial secretions from both inferior lobar bronchi, but there were no detected organisms, including bacteria and acid-fast bacilli. We administered low-dose macrolide therapy with clarithromycin 200mg once daily. However, 1 month later, we discontinued the low-dose macrolide therapy because of hepatotoxicity. Instead, we administered mucolytic agents such as carbocysteine 500mg three times daily.
Nineteen months after gastrectomy, follow-up chest CT showed improvement of the consolidation in the right middle lobe and left lingular segment, but there were no changes in the mucus plug and the centrilobular nodules in both lower lobes (Fig. 1C). There was also a persistent productive cough. Twenty-three months after gastrectomy, we initiated domiciliary nocturnal HFNC (myAIRVO™2, Fisher and Paykel Healthcare, Auckland, New Zealand) for humidification without oxygen at a flow rate of 30L/min and temperature of 34°C. Two months after the initiation of domiciliary nocturnal HFNC, the patient reported that the productive cough had reduced by half. Furthermore, repeat chest CT revealed decrease of mucus plug and centrilobular nodules (Fig. 1D). This patient did not have any of the adverse reactions induced by HFNC, such as pneumothorax, aerophagia, skin irritation, or epistaxis. During this clinical course, the patient had not undergone pulmonary rehabilitation.
This chronic lower respiratory tract infection appeared after total gastrectomy. Recurrent aspiration pneumonia is frequently observed in patients who have undergone total gastrectomy because of the esophageal reflux of the intestinal contents and swallowing dysfunction.4 Therefore, the chronic lower respiratory tract infection in this patient could have been caused by chronic aspiration.
In this patient, domiciliary humidification through HFNC was able to decrease the chest CT abnormalities (Fig. 1B–D) and the symptoms of productive cough. Rea et al.5 reported that domiciliary humidification through HFNC improved the lung function and quality of life of patients with chronic lower airway disorders, including chronic obstructive pulmonary disease and bronchiectasis. These effects of HFNC are considered to be caused by improvement in mucociliary clearance.6 Chronic aspiration after total gastrectomy is mainly induced by nocturnal esophageal reflux.4 This patient used HFNC only at night. Therefore, HFNC was considered to protect the patient from nocturnal aspiration, in addition to improving mucociliary clearance in this patient.
Rea et al. used HFNC at 20–25L/min of flow rate and temperature of 37°C at an average of 1–2h per day, which was short, because mucociliary clearance of 3h of daily use had been demonstrated by Hasani et al.6 This patient used HFNC for more than 6h per day, every night. Future studies are required to evaluate the effect of HFNC in patients with different diseases and different settings.
Patients with chronic lower respiratory tract infection are usually treated with antibiotics, including macrolides, mucolytic agents, and bronchodilators. We conclude that HFNC can be an additional treatment option for airway management in such patients.
FundingNone of the authors have any disclosure or financial support regarding this report.
Conflicts of interestThe authors have no conflict of interest regarding this report.
We have no acknowledgements.