We investigated the measurement properties of the incremental step test in subjects with moderate to severe asthma.
MethodsSubjects with moderate to severe persistent asthma were recruited from a tertiary university hospital specializing in treating severe asthma. All subjects performed one cardiopulmonary exercise test (CPET) and two incremental step tests (IST) in random sequences. Pulmonary gas exchange was measured during all exercise tests. The measurement properties investigated were reliability by intraclass correlation coefficient (ICC), measurement error by the standard error of measurement and minimum detectable difference, construct validity by Pearson's correlation, and interpretability by the ceiling and floor effects.
ResultsFifty subjects (38 females, mean [SD], age 43.7 [11.6] yr, % FEV1 70 [14.3], BMI 28.5 [5.3] kg/m2) completed the study. The peak oxygen uptake (peak VO2) for the CPET was 27.6 [±6.8] ml/kg/min, for the first IST was 22.3 [±5.3] ml/kg/min and for the second IST was 23.3 [±5.3] ml/kg/min. The IST presented excellent reliability (ICC=0.93, CI95% 0.88-0.96), very good measurement error (2.5%), and construct validity for peak VO2 measurement compared to the CPET (r = 0.85; p < 0.001) to assess exercise capacity in subjects with moderate to severe asthma, with appropriate ceiling (10%) and floor (0%) effects.
ConclusionThe IST presented excellent reliability and very good measurement error and validity to assess exercise capacity in subjects with moderate to severe asthma, without ceiling or floor effects.
Subjects with asthma often limit physical exercise to avoid respiratory symptoms,1 which leads to a detrimental health cycle and an aversion to performing exercise and reduces their exercise capacity and activity in daily life.2-3 However, exercise training has been shown to be an important adjunctive therapy for asthma treatment that improves exercise capacity and health-related quality of life.4-5
The cardiopulmonary exercise test (CPET) is the gold standard for measuring exercise capacity; however, the CPET is expensive and requires specialized equipment and a qualified operator. Field walk tests have been used to assess exercise capacity because they are simple, less costly, and less time consuming;6 however, they require corridors of at least 10 meters for appropriate execution.7 Step tests have been considered a reproducible alternative for evaluating the maximum exercise capacity due to their portability, low cost, and ability to be applied without requiring large spaces.8
The incremental step test (IST) has been considered reproducible and reliable in subjects with COPD,8 bronchiectasis,9 hospitalized subjects with acute lung diseases,10 and pulmonary hypertension,11 However, the measurement properties of the IST have not been investigated in adults with asthma. Therefore, the current study aimed to investigate the measurement properties of the IST in subjects with moderate to severe asthma.
MethodsStudy designThis study was approved by the Ethics Review Board of the Clinical Hospital (47710715.9.0000.0068), and all participants provided written informed consent. The subjects with asthma were evaluated on two nonconsecutive days, at least 48 hours apart. On day 1, anthropometric indices, clinical asthma control (Asthma Control Questionnaire, ACQ), and lung function (spirometry) were assessed. After that, the subjects were randomized to perform either a cardiopulmonary exercise test (CPET) or two incremental step tests. On day 2, the subjects performed the other test, the CPET or IST, according to randomization.
All incremental tests were performed using a metabolic gas analyzer. Subjects were instructed to use a bronchodilator (400 μg of salbutamol) 15 minutes before each test to obtain a better performance on the cardiopulmonary exercise.12
ParticipantsSubjects with asthma aged between 18 and 60 years with a body mass index (BMI) between ≥20 and ≤ 40 kg/m2 were recruited from a university hospital during a routine medical consultation. They were diagnosed with moderate or severe persistent asthma according to the Global Initiative for Asthma13 and clinically stable for at least six months (i.e., no hospitalizations, emergency care, or changes in medication in the last 30 days for at least 30 days). All patients received short- and long-acting bronchodilators and inhaled corticosteroids, and none received immunobiological monoclonal therapy. The exclusion criteria were the presence of cardiovascular, musculoskeletal, or other chronic pulmonary diseases; uncontrolled hypertension or diabetes; active cancer; use of oral corticosteroids; smokers or ex-smokers (≥10 packs/year or stopped smoking for a period equal to or longer than 12 months); and pregnancy or breastfeeding.
MeasurementsAsthma controlThe ACQ-714 validated for Brazilian Portuguese15 was used. The questionnaire has seven questions for daytime and nocturnal asthma symptoms, activity limitations, dyspnea, wheezing, use of a rescue bronchodilator (short-acting β2-agonist) in the past week and the forced expiratory volume in the 1st second (FEV1, in % of predicted, prebronchodilator).16 The responses are given on a 7-point scale, and the overall score is the mean of the responses (0=totally controlled, 6=severely uncontrolled). Values greater than or equal to 1.5 indicate uncontrolled asthma; values between 0.75 and 1.5 indicate partially controlled asthma, and values less than 0.75 indicate fully controlled asthma.14
Lung functionPulmonary function testing was performed according to the current American Thoracic Society (ATS)/European Respiratory Society (ERS) guidelines.17 Forced vital capacity (FVC), FEV1, and the FEV1/FVC ratio absolute values were obtained and expressed as percentages according to the reference values for the Brazilian population.18
Cardiopulmonary exercise testingThe CPET was performed using an electric treadmill ergometer (Jaeger™) linked to a digital exercise evaluation system with a gas analyzer (Vyntus CPX™). The peak oxygen uptake (peak VO2), minute ventilation (VE), carbon dioxide production (VCO2), respiratory exchange ratio (RER), heart rate (HR), modified Borg score for dyspnea (BD), and leg fatigue (BF) at rest and at the end of the exercise test were analyzed. The criteria for exercise interruption before symptom limitation were in accordance with the American Thoracic Society/American College of Chest Physicians guidelines,19 The following conditions were also used as interruptions to the exercise test: loss of leg coordination, mental confusion, and dizziness or fainting, as previously established.19
The ramp protocol was used with a fixed speed and a 2% increase in the slope every minute. Before the test, the subject was asked to choose one of the following speeds: 2.4, 3.6, 4.8, 6.0, or 7.2 km/h; therefore, the protocol was individualized.20-21 Before the exercise test, the subjects were exposed to all speeds for periods between 1 and 3 minutes before choosing the velocity. The criteria for the CPET test interruption included the following: chest pain suggestive of ischemia; complex ectopy; second- or third-degree heart block; a fall in the systolic pressure of 20 mmHg from the highest value; arterial hypertension (250 mmHg systolic; 120 mmHg diastolic); severe desaturation (SpO2 of 80% accompanied by symptoms or signs of severe hypoxemia).
Incremental step testThe subjects with asthma stepped up and down on a 20 cm high wooden bench (width 40 cm, depth 60 cm) as previously described.8 An audio signal dictating the stepping rate played on a compact disc. The initial stepping rate was 10 steps/min, with a one-step increment every 30 s up to the tolerance limit. The researcher interrupted the test when the subject was unable to keep the pace for 15 s.22 The tests were performed using a system with a gas analyzer (Vyntus CPX™), and the variables recorded were the same as those for the CPET. The results from IST-1 and IST-2 were used to perform the reliability analyses. Two ISTs were performed on the same day with a rest period of at least 30 minutes between them. The second test was performed when the participant's vital signs had returned to baseline levels to ensure the same clinical conditions for the patient in both tests. The IST with better performance regarding the peak VO2 value was called the best IST (b-IST). The values from the b-IST were used for validity and interpretability analyses.
Statistical analysisStatistical analysis was performed using Sigma Stat statistical software, version 2.03 (SPSS Inc., USA). The normality of the data was assessed using the Kolmogorov–Smirnov test. Categorical variables were expressed as an absolute number, percentage, and frequency. A paired t-test was used to compare the variables of the CPET versus the b-IST and IST–1 versus IST–2. The Wilcoxon test was used for nonparametric data. All p values less than 0.05 were considered to be indicative of statistical significance.
Analysis of the measurement propertiesReliabilityThe property reliability involves three domains: reliability, error measurement, and internal consistency. However, as this study is about a field test, internal consistency has not been evaluated. The reliability of the IST was analyzed by test-retest scores (IST-1 and IST-2) using intraclass correlation coefficient (ICC) model 2,1 (absolute subtype agreement for single measurements) with 95% confidence intervals (CI95%). The classification adopted was <0.40= low, from 0.40 to 0.75= moderate; from 0.76 to 0.90= substantial and > 0.90= excellent.23
The measurement error is associated with the absolute error of the measurement.24 The test and retest scores for each test were evaluated by the standard error of measurement (SEM) and the minimal detectable change with 90% confidence (MDC90). SEM was analyzed using the SEM=Standard Deviation√1-ICC. The SEM was considered very good if <5% of the total score, good if ≥5% and <10%, doubtful if ≥10% and <20%, and negative if >20%.25 The MDC90 was calculated considering the number of steps in the IST–1 and IST–2 as follows: score ranged in the test, subtracted from the score in the retest, and divided by √2×SEM.26 The limits of agreement and precision of peak VO2 between the b-IST and CPET and between the IST-1 and IST-2 were calculated using the Bland and Altman method.27
Construct validityThe validity was analyzed by the correlation of peak VO2 (l/min) obtained from both the CPET and IST–b. The hypothesis is that the correlation between peak VO2 assessed via the CPET and IST-b was strong and positive. Pearson's correlation test was used. The classification adopted was r<0.30 indicating a weak correlation; 0.30≥ and <0.60 as moderate; and r >0.60 as strong.28
InterpretabilityThe floor and ceiling effects were analyzed and considered to be present if 15% or more of the individuals reached the minimum or maximum score in the evaluation, respectively.23
ResultsFrom a total of 338 subjects eligible for this study, 286 were excluded for the following reasons: 154 were aged >60 years, 24 refused to participate, 15 had heart diseases, 14 had a BMI ≥40 kg/m2, 13 had other associated lung diseases, 9 were smokers, 9 presented gait impairment, 5 were not clinically stable, 5 were pregnant, 4 were participating in another research protocol, and 38 were for other reasons. Therefore, 50 subjects completed the study, and their characteristics are described in Table 1. For the CPET, 10 subjects (18.5%) chose a speed of 3.6 km/h, 38 subjects (70.3%) chose a speed of 4.8 km/h, 5 subjects (9.2%) chose a speed of 6.0 km/h and one subject (1.8%) chose a speed of 7.2 km/h.
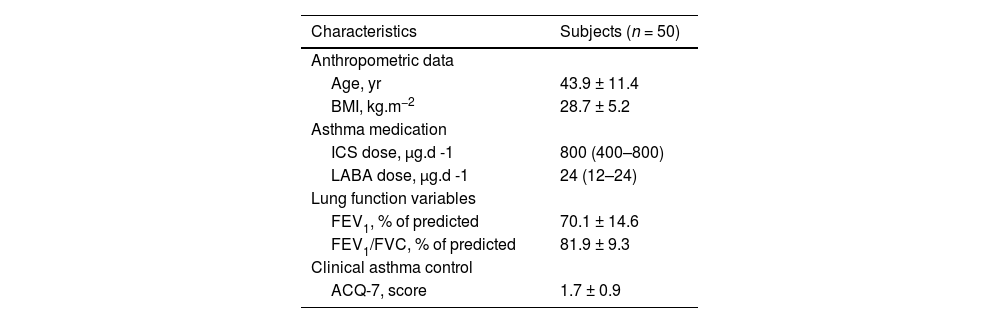
Characteristics of adults with asthma.
Legend: Data are presented as the mean ± SD or interquartile interval. BMI, body mass index; ICS, inhaled corticosteroid; LABA, long-action β2 agonist; FEV1, forced expiratory volume in the 1st second; FVC, forced vital capacity; % of predicted value for the Brazilian population18; ACQ, Asthma Control Questionnaire; yr, years old; kg*m−2, kilograms per square meter; µg.d −1, micrograms per day.
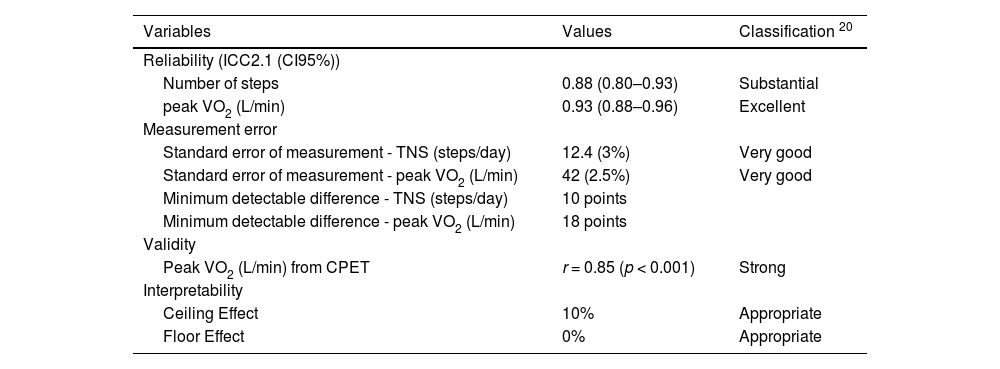
Reliability analysis demonstrated an ICC of 0.88 (95% CI 0.80–0.93) for the total number of steps and 0.93 (95% CI 0.88–0.96) for peak VO2 (l/min), showing substantial and excellent reliability. The means of the peak VO2 from IST-1 (1673 ± 0.42 l/min) and IST-2 (1754 ± 0.43 l/min) were similar (p > 0.05) (Table 2). The total number of steps and peak VO2 showed a very good measurement error between test-retest, SEM% 12.4 Total Number of Steps (TNS) (3%) and MDC90 42 TNS (2.5%) (Table 3).
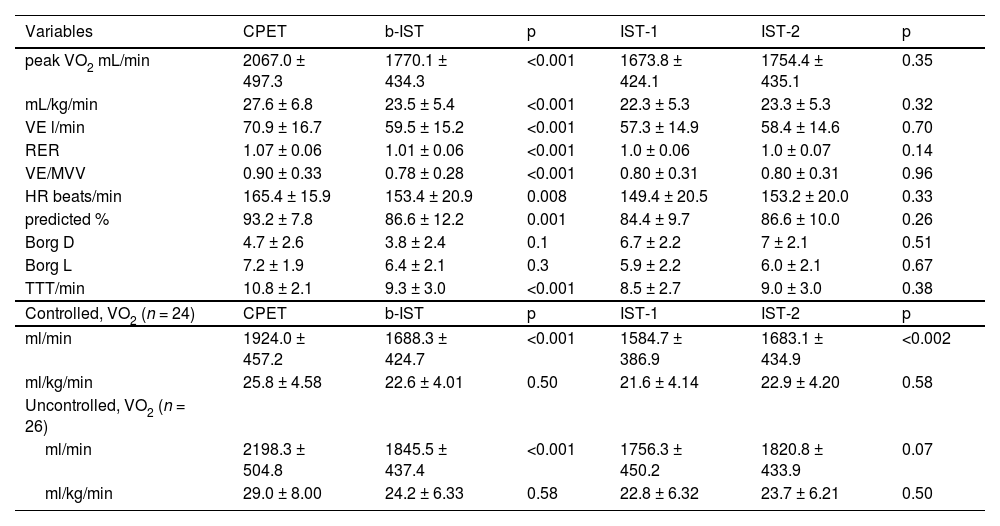
Comparison of physiological responses on the CPET versus the b-IST and on IST-1 and IST-2 in subjects with asthma and comparison between controlled and noncontrolled (n = 50).
Legend: Data are presented as the means ± SD or n (%). peak VO2 L/min, peak oxygen uptake milliliters per minute; kg, kilograms; VE, minute ventilation; RER, respiratory exchange ratio; VE/MVV, minute ventilation per maximum voluntary ventilation; HR, heart rate; Borg D, dyspnea score; Borg L, leg discomfort score; TTT, total test time; Controlled, subjects with controlled asthma (ACQ<1.5 scores); Uncontrolled, subjects with uncontrolled asthma (ACQ>1.5).
Measurement properties of the modified incremental step test for adults with moderate or severe asthma (n = 50).
| Variables | Values | Classification 20 |
|---|---|---|
| Reliability (ICC2.1 (CI95%)) | ||
| Number of steps | 0.88 (0.80–0.93) | Substantial |
| peak VO2 (L/min) | 0.93 (0.88–0.96) | Excellent |
| Measurement error | ||
| Standard error of measurement - TNS (steps/day) | 12.4 (3%) | Very good |
| Standard error of measurement - peak VO2 (L/min) | 42 (2.5%) | Very good |
| Minimum detectable difference - TNS (steps/day) | 10 points | |
| Minimum detectable difference - peak VO2 (L/min) | 18 points | |
| Validity | ||
| Peak VO2 (L/min) from CPET | r = 0.85 (p < 0.001) | Strong |
| Interpretability | ||
| Ceiling Effect | 10% | Appropriate |
| Floor Effect | 0% | Appropriate |
Legend: ICC = intraclass correlation coefficient; peak VO2= peak of oxygen uptake; TNS= total number of steps; r = Pearson's correlation. Classification according to COSMIN.20 Data are presented as n (%); intraclass correlation coefficient (ICC - 95% confidence interval). The alpha level used for this analysis was <0.7, indicating poor consistency, and ≥ 0.70 was considered adequate.
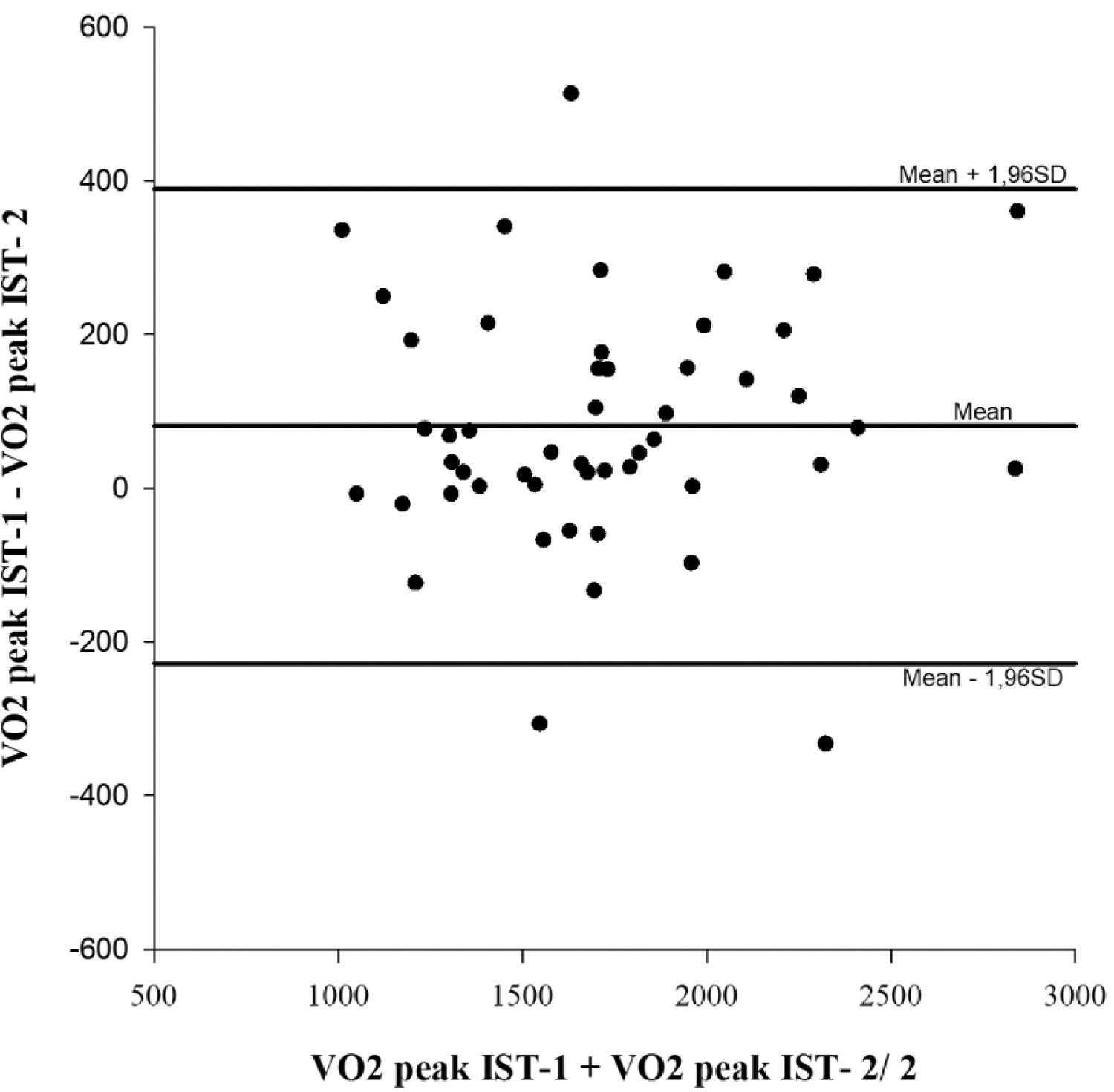
The Bland–Altman plot also showed an average difference in the peak VO2 of ± 93 mL/min between both IST tests (Fig. 1). In addition, a strong linear correlation was observed in the peak VO2 between the IST-1 and IST-2, considering the subjects altogether (r = 0.9; p < 0.0001) (Table 3).
A ceiling effect was observed in 10% of the subjects, and an appropriate floor effect was observed since none of the subjects presented (0%) (Table 3).
The CPET and the b-ISTDifferences were observed between the CPET and the b-IST when peak VO2 was evaluated in ml/min. In addition, a between-group difference was observed according to the disease control comparing controlled (n = 24) versus uncontrolled asthma (n = 26) (Table 2). However, no difference between those groups was observed [CPET: controlled 1,925 ± 458 vs. uncontrolled 2,198 ± 505 mL/min (p = 0.06); b-IST: controlled 1688 ± 425 vs. uncontrolled 1846 ± 437 mL/min (p = 0.20)]. On the other hand, when the subjects' weight was considered (peak VO2 in mL/kg), no difference was verified intra- or intertest when comparing subjects with controlled versus uncontrolled asthma (p = 0.09).
A lower cardiopulmonary response was observed on the b-IST compared to the CPET, except for perceived exertion in terms of dyspnea and leg fatigue (Table 2). In addition, a strong linear correlation was observed in the peak VO2 between the b-IST (Table 2) and the CEPT (r = 0.85; p < 0.001), and homoscedasticity was observed between the two tests.
DiscussionTo the best of our knowledge, this is the first study to describe the reliability, measurement error, construct validity, and interpretability of the incremental step test for subjects with moderate or severe asthma following the recommendations of COSMIN measurement properties.29
The reliability of the IST in our study (ICC: TNS=0.88; peak VO2 =0.93) was similar to those reported for subjects with COPD (ICC: TNS=0.99; peak VO2 =0.99).8 The similar reliability observed in the IST between asthma and COPD subjects could probably be explained by the fact that both had reduced exercise capacity resulting in high dyspnea and fatigue levels (Table 2). The reliability values were slightly higher in the COPD subjects, perhaps because they had lower exercise capacity than those with asthma.30 Another possible explanation could be the use of the same step-test protocol. Studies using different types of step tests have shown reliability between substantial to excellent (ICC between 0.77 and 0.99) in healthy adults 31 and older adults with other respiratory diseases.32-33 Moreover, the IST measurement error indicated by the error measurement value between IST-1 and IST-2 was less than 5% for TNS (3% - 12.4 steps) and peak VO2 (2.5% - 0.04 L/min), which is classified as very good. The MDC was used to identify the variation between tests, and the retest can be considered to be due to the subject's performance change and not an internal error of the test. Our study showed a very good MDC (TNS=9.7 steps; peak VO2 =17.9 L/min). These findings are similar to those reported by Munari et al.,34 who observed an SEM of 4.27 when evaluating physiological responses to the 6-min step test in subjects with COPD.
The Bland–Altman limits of agreement for peak VO2 in our study were narrow with a high degree of reliability for exercise capacity during IST-1 and IST-2. These results are in agreement with those performed using the Chester step test for subjects with COPD.35 Later, the same group showed that the IST is also reproducible in subjects with bronchiectasis.9 Our results corroborate those obtained by Coquart et al. (2015),36 which also found good reliability and higher performance during the second 6MST in patients with COPD. Other authors suggest that the learning effect can be a plausible explanation for justifying better performance in the second test compared to the first. Dal Corso et al. (2013)8 found an increase of approximately 5% TNS in the second IST performed on the same day with a negative mean difference in the Bland and Altman analysis in subjects with COPD. In addition, we did not observe floor or ceiling effects in our patients using the IST. The number of steps taken by subjects with asthma ranged from 49 to 425, and only 10% of the subjects climbed 250 steps.
Our results showed that the IST is valid for measuring exercise capacity compared to the CPET (r = 0.85, p < 0.001). Moreover, since even the profile of incremental field tests is not strictly linear, they are very close to that.37 Therefore, the IST can be considered accurate for assessing exercise capacity at a submaximal level, evidenced by the ICC values of 0.88 (95% CI 0.80–0.93) for the total number of steps and 0.93 (95% CI 0.88–0.96) for peak VO2 (l/min), showing substantial and excellent reliability.
Despite this, the present study also demonstrated that IST is not interchangeable with the CPET since the subjects with moderate to severe asthma did not reach the maximal exercise capacity. A difference of approximately 15% in the peak VO2 was observed between the IST and the CPET. In accordance with our results, previous studies with obese women have suggested that a self-paced step test (six-minute step test, 6MST) elicits a lower cardiopulmonary response than the CPET performed on a cycle ergometer (approximately 0.35 l/min).38 We chose to evaluate exercise capacity in subjects with asthma using a treadmill protocol because this procedure has been used in most studies that evaluated the benefits of exercise training in asthmatic subjects.39-40
Similarly, the population included in this study had uncontrolled asthma, as expected in subjects with moderate to severe disease. This disease severity profile reproduces most subjects allocated to studies involving physical capacity and asthma. Freitas et al. (2021)41 showed that overweight and/or obese subjects with asthma have the worst clinical control (2.8 ± 0.7 scores). These results reinforce ours, showing that subjects with BMI>24.9 kg/m2 also had uncontrolled asthma. The same study also showed that obesity, anxiety, and depression symptoms were associated with the poorest clinical outcomes.42 In the present study, we observed a difference in the peak VO2 (in mL/min) between the CPET and IST between individuals with controlled or noncontrolled asthma; however, no difference was observed when the peak VO2 was normalized by body weight (mL/kg/min). These results only suggest that the difference observed was a consequence of body weight and not asthma control.
Other studies have evaluated field tests in subjects with asthma, and they observed similar results. Jürgensen et al. (2016)43 compared the CPET with the Incremental Shuttle Walk Test in young obese women and showed that the ISWT induced a lower peak VO2 than the CPET (1,678±269 versus 1,934±319 mL/min, respectively). However, we believe that the IST is superior to walking tests in subjects with asthma because it is an activity that requires greater ventilation in a subject's daily life. Additionally, climbing stairs is a common limitation reported by subjects with asthma that can trigger fatigue and shortness of breath symptoms.
Certain limitations should be noted in the present study. A major limitation of this study was the sample of 50 subjects. Terwee et al. 201221 recommend one hundred participants for studies with unidimensional instruments and analysis of reliability. However, several studies have used samples of 50 participants, and the sample was considered to be a good size for statistical tests. In addition, the IST was compared with the CPET, which is considered the gold standard for assessing exercise capacity. However, the CPET is an expensive test, which makes a much larger sample difficult. Another limitation is that our sample consisted mainly of women; however, asthma prevalence is higher in adult females.44 In our opinion, the higher female prevalence does not reduce the relevance of our findings; however, some caution should be taken in extrapolating our results to male subjects with asthma and other asthma endotypes. Finally, despite the limitations presented above, our study has a major strength: the randomization of patients to perform the CPET and IST, which was important to reduce bias.
ConclusionsOur results demonstrate that the IST showed excellent reproducibility and strong validity in subjects with moderate to severe asthma. These results suggest that the IST provides a reliable measure of exercise capacity and can be used in clinical practice and research. However, we recommend that two tests minimize the learning effect. In addition, future studies are needed to assess whether the IST is a valid instrument to assess responsiveness to pharmacological and nonpharmacological treatments in this population.