Unlike large population studies about cardiovascular components and how they adapt to intensive physical activity, there is less research into the causes of enlargement of the respiratory system in athletes (e.g. vital capacity, maximum flow rates and pulmonary diffusion capacity). The purpose of this research was to study and compare pulmonary function in different types of sports and compare them with controls in order to find out which sports improve lung function the most.
Materials and methodPulmonary functional capacities, vital capacity (VC), forced vital capacity (FVC), forced expiratory volume in one second (FEV1) and maximum voluntary ventilation (MVV) of 493 top athletes belonging to 15 different sports disciplines and of 16 sedentary individuals were studied. Pulmonary function test was performed according to ATS/ERS guidelines.
ResultsBasketball, water polo players and rowers had statistically higher vital capacity (VC), forced vital capacity (FVC), forced expiratory volume in one second (FEV1) than the healthy sedentary control individuals. Football and volleyball players had lower VC while FVC was higher in the football group compared to controls. Peak expiratory flow was lower in boxing, kayak, rugby, handball, taekwondo and tennis. The maximum voluntary ventilation (MVV) was significantly higher in water polo players and rowers. Boxers had statistically lower MVV than the controls. Players of other sports did not differ from the control group.
ConclusionThe study suggests that specific type of training used in basketball, water polo or rowing could have potential for improving pulmonary function and rehabilitation.
Lung function tests provide qualitative and quantitative evaluation of pulmonary function and are of the highest importance in estimating the fitness of an individual from a physiological point of view.1 Spirometry is a physiological test that measures how an individual inhales or exhales volumes of air as a function of time. It is the most commonly used pulmonary function test in the objective assessment of respiratory system function.2 Lung volume is fairly well predicted on the basis of age, height and weight, but lung volumes which are larger than predicted have been repeatedly observed in athletes compared to their control counterparts who are not engaged in any kind of regular physical exercise.3,4 There are some physiological explanations as to why athletes have higher lung volumes, but still, this is an uncharted field.5 Studies about athletes’ respiratory functions are rather limited or have been tested on too small number of participants, mostly related to individual sports.6,7 There is also a lack of up-to-date interventional studies in the field.
The aim of this study, therefore, was to examine the pulmonary functional capacities of the different groups of top athletes, discover in which sports the respiratory parameters are the best and to compare them with sedentary controls.
Materials and methodsParticipantsFour hundred and ninety three asymptomatic Caucasian international level competitors (18–34 years of age; mean age 21±4) who attended a regular check-up programme over a four-year period were included in the study. The study involved athletes who had actively played competitive sports for at least five years and trained at least 15h a week. Spirometric data for each participant were consecutively collected for that period of time. Participants were not considered eligible for the study if they had a training break of more than 6 months during their athletic career.
The study included the following sports: athletics (n=12), cycling (n=39), boxing (n=19), football (n=19), kayak (n=34), kickboxing (n=10), basketball (n=67), volleyball (n=70), rugby (n=43), handball (n=102), wrestling (n=10), taekwondo (n=10), tennis (n=13), water polo (n=14) and rowing (n=15).
The admission criteria for the 16 sedentary controls were they were not connected with any particular sport and did not have a regular exercise programme. All participants were non-smokers, and none had a history of recurrent respiratory illness, such as asthma or a chronic cough.
Ethical approvementThe study was approved by Ethics Committee of the School of Medicine University of Belgrade.
DesignBefore being tested, examinees were asked to have a light dinner before 8PM and light breakfast before 8AM. No intake of stimulants such as alcohol or caffeine or any other drug was allowed in the 12h before testing. Information on participant age, date of birth, and the number of years of training was obtained verbally. Participants were informed of research requirements prior to attendance and signed consent forms on arrival for testing. It was made clear that they could discontinue the testing at any time.
The testing took place in laboratory settings, at the same time of day (morning 09–11AM), using the same instruments and techniques. Measurements were carried out under standard environmental conditions; comfort temperature (between 18 and 22°C), atmospheric pressure of 760mmHg, and relative atmospheric humidity of 30–60%. The temperature, humidity and atmospheric pressure were continuously measured at the lab.
Spirometry was performed using the (Turninac, Pneumotah) Pony FX (Cosmed Pulmonary Function Equipment; Italy). Pulmonary function test followed the ATS/ERS guidelines.8 Spirometry was performed in a sitting position in arm chairs at the place of training before any warm-up, wearing light clothing and a nose clip. Pulmonary function tests were performed three times for each participant and the best technique was accepted. The highest level for forced vital capacity (FVC) and forced expiratory volume in one second (FEV1), were taken independently from the three curves.
Body mass (kg; Seca 761 scales, ±0.5kg; Seca Co., Germany) and stature (m; Cranlea JP60 portable stadiometer, +0.001m; Cranlea & Co) were also measured using standardised anthropometric techniques. Body mass index (BMI) was calculated for all the participants as the ratio of body mass (kilograms) divided by body height (metres) squared. The participants percentage of body fat (BF%) was measured using the bioimpedance segmental body composition analyzer (BC-418 Segmental Body Composition Analyzer, Tanita, Illinois, USA).
StatisticsContinuous data are expressed as mean±SD. Categorical data are expressed as frequencies. Statistical significance was set for a 2-tailed p value<0.05. The mean values of anthropometric characteristics and of pulmonary functional capacities of different groups of athletes have been compared by means of Students’ ‘t’ distribution test, and the level of significance is shown below the tables. All analyses were adjusted for age and body mass index.
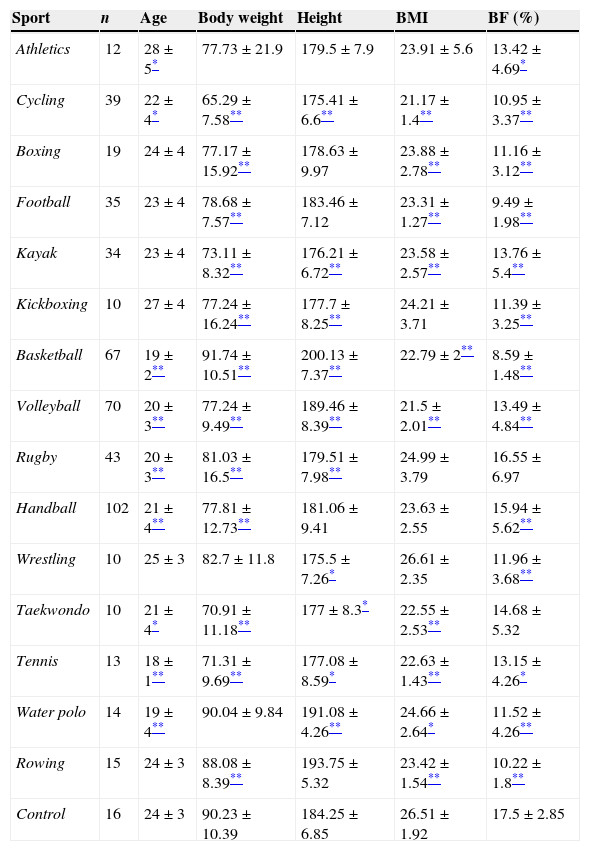
ResultsThe mean and standard deviation of age, height, weight and anthropometric characteristics of different groups of athletes and of sedentary controls are presented in Table 1. Statistically significant high differences were observed in height and weight compared to controls in almost all sports (p<0.01), except for athletics, wrestling and water polo where no significant difference was observed. Basketball players were the tallest and heaviest. The wrestling group was the shortest, while the taekwondo players were the thinnest. In accordance with previous observations, body mass index (BMI) was significantly different to controls in almost all groups (p<0.01), except in the case of athletics, rugby and handball where no significant difference was registered. Percentage of body mass had a high statistical significance in almost all groups compared to controls (p<0.01), while in the case of athletics and tennis the significance was not high, but was significantly different to the controls (p<0.05). There were no significant differences in the case of taekwondo and rugby players. Out of all the athletes rugby players had the highest percentage of body fat, while the lowest was found in basketball group.
Demographic and anthropometric characteristics of athletes and control group.
| Sport | n | Age | Body weight | Height | BMI | BF (%) |
|---|---|---|---|---|---|---|
| Athletics | 12 | 28±5* | 77.73±21.9 | 179.5±7.9 | 23.91±5.6 | 13.42±4.69* |
| Cycling | 39 | 22±4* | 65.29±7.58** | 175.41±6.6** | 21.17±1.4** | 10.95±3.37** |
| Boxing | 19 | 24±4 | 77.17±15.92** | 178.63±9.97 | 23.88±2.78** | 11.16±3.12** |
| Football | 35 | 23±4 | 78.68±7.57** | 183.46±7.12 | 23.31±1.27** | 9.49±1.98** |
| Kayak | 34 | 23±4 | 73.11±8.32** | 176.21±6.72** | 23.58±2.57** | 13.76±5.4** |
| Kickboxing | 10 | 27±4 | 77.24±16.24** | 177.7±8.25** | 24.21±3.71 | 11.39±3.25** |
| Basketball | 67 | 19±2** | 91.74±10.51** | 200.13±7.37** | 22.79±2** | 8.59±1.48** |
| Volleyball | 70 | 20±3** | 77.24±9.49** | 189.46±8.39** | 21.5±2.01** | 13.49±4.84** |
| Rugby | 43 | 20±3** | 81.03±16.5** | 179.51±7.98** | 24.99±3.79 | 16.55±6.97 |
| Handball | 102 | 21±4** | 77.81±12.73** | 181.06±9.41 | 23.63±2.55 | 15.94±5.62** |
| Wrestling | 10 | 25±3 | 82.7±11.8 | 175.5±7.26* | 26.61±2.35 | 11.96±3.68** |
| Taekwondo | 10 | 21±4* | 70.91±11.18** | 177±8.3* | 22.55±2.53** | 14.68±5.32 |
| Tennis | 13 | 18±1** | 71.31±9.69** | 177.08±8.59* | 22.63±1.43** | 13.15±4.26* |
| Water polo | 14 | 19±4** | 90.04±9.84 | 191.08±4.26** | 24.66±2.64* | 11.52±4.26** |
| Rowing | 15 | 24±3 | 88.08±8.39** | 193.75±5.32 | 23.42±1.54** | 10.22±1.8** |
| Control | 16 | 24±3 | 90.23±10.39 | 184.25±6.85 | 26.51±1.92 | 17.5±2.85 |
Data are expressed as mean±SD. BMI, body mass index; BF, body fat.
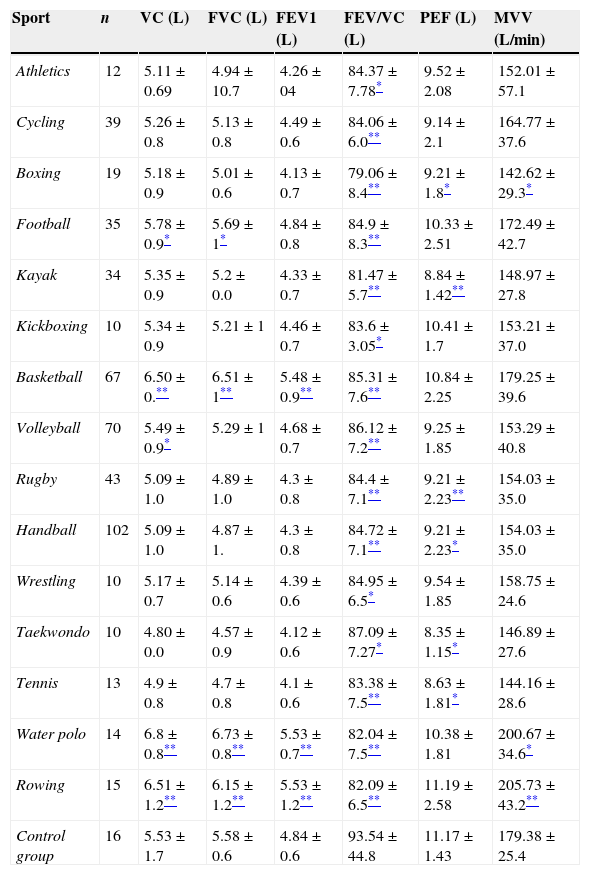
Table 2 exhibits the mean and standard deviations of VC, FVC, PEF (expressed in litres), FEV1/FVC, MVV (l/min) of the different sports and of the sedentary group. VC was significantly higher in basketball, football, water polo and rowing than in the control group (p<0.01), while in case of volleyball, VC was lower (p<0.05). Other groups did not differ from controls. Statistically significant differences were found in football, basketball, rowing and water polo comparing to control group when observing FVC (p<0.05; in case of football p<0.01). There was a statistically significant difference in FEV1 from controls for basketball, water polo and rowing (p<0.01). However when analysing PEF value, the difference was not statistically different in athletics, cycling, football, kickboxing, basketball, volleyball, water polo and rowing, while other sports did have a statistically significant difference compared to controls (p<0.05). MVV differed statistically for boxing and water polo (p<0.05), while statistical significance was higher in rowing (p<0.01) compared to controls. Boxers had statistically significant lower values of MVV than controls (p<0.01).
Comparison of respiratory parameters between athletes and the control group.
| Sport | n | VC (L) | FVC (L) | FEV1 (L) | FEV/VC (L) | PEF (L) | MVV (L/min) |
|---|---|---|---|---|---|---|---|
| Athletics | 12 | 5.11±0.69 | 4.94±10.7 | 4.26±04 | 84.37±7.78* | 9.52±2.08 | 152.01±57.1 |
| Cycling | 39 | 5.26±0.8 | 5.13±0.8 | 4.49±0.6 | 84.06±6.0** | 9.14±2.1 | 164.77±37.6 |
| Boxing | 19 | 5.18±0.9 | 5.01±0.6 | 4.13±0.7 | 79.06±8.4** | 9.21±1.8* | 142.62±29.3* |
| Football | 35 | 5.78±0.9* | 5.69±1* | 4.84±0.8 | 84.9±8.3** | 10.33±2.51 | 172.49±42.7 |
| Kayak | 34 | 5.35±0.9 | 5.2±0.0 | 4.33±0.7 | 81.47±5.7** | 8.84±1.42** | 148.97±27.8 |
| Kickboxing | 10 | 5.34±0.9 | 5.21±1 | 4.46±0.7 | 83.6±3.05* | 10.41±1.7 | 153.21±37.0 |
| Basketball | 67 | 6.50±0.** | 6.51±1** | 5.48±0.9** | 85.31±7.6** | 10.84±2.25 | 179.25±39.6 |
| Volleyball | 70 | 5.49±0.9* | 5.29±1 | 4.68±0.7 | 86.12±7.2** | 9.25±1.85 | 153.29±40.8 |
| Rugby | 43 | 5.09±1.0 | 4.89±1.0 | 4.3±0.8 | 84.4±7.1** | 9.21±2.23** | 154.03±35.0 |
| Handball | 102 | 5.09±1.0 | 4.87±1. | 4.3±0.8 | 84.72±7.1** | 9.21±2.23* | 154.03±35.0 |
| Wrestling | 10 | 5.17±0.7 | 5.14±0.6 | 4.39±0.6 | 84.95±6.5* | 9.54±1.85 | 158.75±24.6 |
| Taekwondo | 10 | 4.80±0.0 | 4.57±0.9 | 4.12±0.6 | 87.09±7.27* | 8.35±1.15* | 146.89±27.6 |
| Tennis | 13 | 4.9±0.8 | 4.7±0.8 | 4.1±0.6 | 83.38±7.5** | 8.63±1.81* | 144.16±28.6 |
| Water polo | 14 | 6.8±0.8** | 6.73±0.8** | 5.53±0.7** | 82.04±7.5** | 10.38±1.81 | 200.67±34.6* |
| Rowing | 15 | 6.51±1.2** | 6.15±1.2** | 5.53±1.2** | 82.09±6.5** | 11.19±2.58 | 205.73±43.2** |
| Control group | 16 | 5.53±1.7 | 5.58±0.6 | 4.84±0.6 | 93.54±44.8 | 11.17±1.43 | 179.38±25.4 |
Data are expressed as mean±SD. FVC, forced vital capacity; FEV1, forced expiratory volume in 1s; PEF, peak expiratory flow; VC, vital capacity; FEV1/VC, Tiffeneau-Pinelli index; MVV, maximum voluntary ventilation.
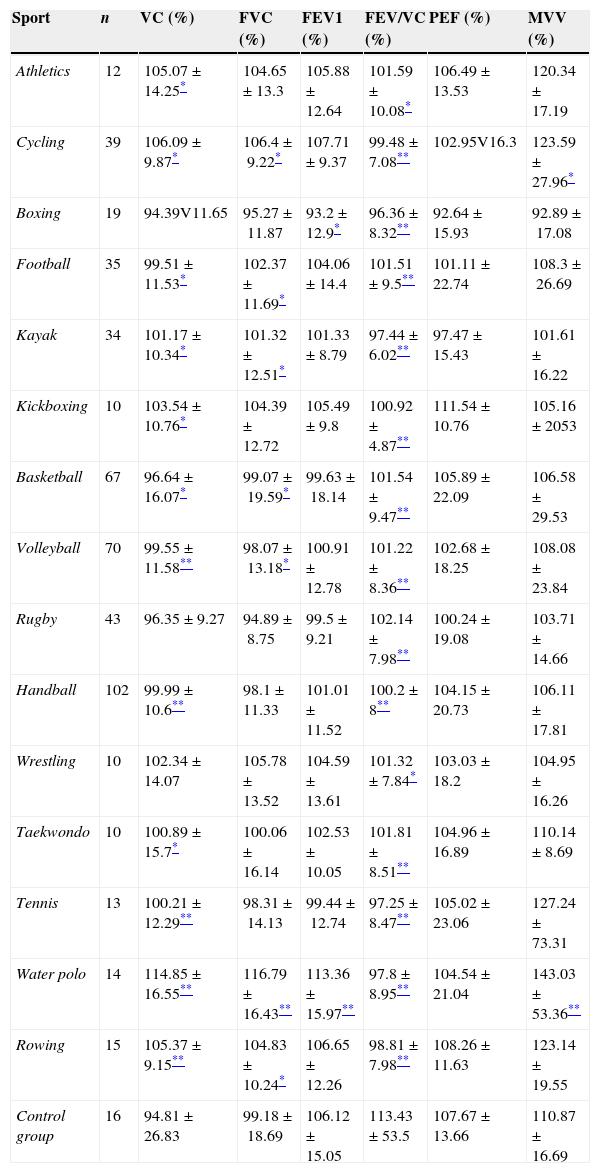
Table 3 shows percentage of the actual realised value from predicted ones of respiratory parameters. There was a statistically significant difference in VC from the control group in all groups, except for boxing and rugby. In the case of FVC, a statistically significant difference was registered in cycling, football, kayak, basketball, volleyball, water polo and rowing. Observing FEV1, a statistically significant difference was registered in only boxing and water polo groups compared to controls (p<0.05, p<0.01, respectively). There was no significant difference in values of PEF among athletes from controls. Maximal voluntary ventilation was statistically significantly different in case of cycling and water polo (p<0.05, p<0.01, respectively).
Comparison of respiratory parameters between athletes and the control group in percentage.
| Sport | n | VC (%) | FVC (%) | FEV1 (%) | FEV/VC (%) | PEF (%) | MVV (%) |
|---|---|---|---|---|---|---|---|
| Athletics | 12 | 105.07±14.25* | 104.65±13.3 | 105.88±12.64 | 101.59±10.08* | 106.49±13.53 | 120.34±17.19 |
| Cycling | 39 | 106.09±9.87* | 106.4±9.22* | 107.71±9.37 | 99.48±7.08** | 102.95V16.3 | 123.59±27.96* |
| Boxing | 19 | 94.39V11.65 | 95.27±11.87 | 93.2±12.9* | 96.36±8.32** | 92.64±15.93 | 92.89±17.08 |
| Football | 35 | 99.51±11.53* | 102.37±11.69* | 104.06±14.4 | 101.51±9.5** | 101.11±22.74 | 108.3±26.69 |
| Kayak | 34 | 101.17±10.34* | 101.32±12.51* | 101.33±8.79 | 97.44±6.02** | 97.47±15.43 | 101.61±16.22 |
| Kickboxing | 10 | 103.54±10.76* | 104.39±12.72 | 105.49±9.8 | 100.92±4.87** | 111.54±10.76 | 105.16±2053 |
| Basketball | 67 | 96.64±16.07* | 99.07±19.59* | 99.63±18.14 | 101.54±9.47** | 105.89±22.09 | 106.58±29.53 |
| Volleyball | 70 | 99.55±11.58** | 98.07±13.18* | 100.91±12.78 | 101.22±8.36** | 102.68±18.25 | 108.08±23.84 |
| Rugby | 43 | 96.35±9.27 | 94.89±8.75 | 99.5±9.21 | 102.14±7.98** | 100.24±19.08 | 103.71±14.66 |
| Handball | 102 | 99.99±10.6** | 98.1±11.33 | 101.01±11.52 | 100.2±8** | 104.15±20.73 | 106.11±17.81 |
| Wrestling | 10 | 102.34±14.07 | 105.78±13.52 | 104.59±13.61 | 101.32±7.84* | 103.03±18.2 | 104.95±16.26 |
| Taekwondo | 10 | 100.89±15.7* | 100.06±16.14 | 102.53±10.05 | 101.81±8.51** | 104.96±16.89 | 110.14±8.69 |
| Tennis | 13 | 100.21±12.29** | 98.31±14.13 | 99.44±12.74 | 97.25±8.47** | 105.02±23.06 | 127.24±73.31 |
| Water polo | 14 | 114.85±16.55** | 116.79±16.43** | 113.36±15.97** | 97.8±8.95** | 104.54±21.04 | 143.03±53.36** |
| Rowing | 15 | 105.37±9.15** | 104.83±10.24* | 106.65±12.26 | 98.81±7.98** | 108.26±11.63 | 123.14±19.55 |
| Control group | 16 | 94.81±26.83 | 99.18±18.69 | 106.12±15.05 | 113.43±53.5 | 107.67±13.66 | 110.87±16.69 |
The results discussed above indicate that football, water polo, rowing and basketball players had higher values of VC compared to the controls. Volleyball players had lower values of VC than the controls. Higher values of forced vital capacity were registered in basketball, water polo and rowers compared to controls. It contrasts with previous reports which found that all athletes, regardless of the sport, had higher lung volumes than physically inactive persons 3,4,6,9,10. Our study showed that the researched respiratory parameters in athletes had approximately the same value of lung volumes as the control group, except for above mentioned groups.
As the lung volumes depend on height, higher values are expected in all tall athletes 2.
We found higher value in basketball, water polo and rowers who were significantly taller than controls. But, in the case of volleyball players, even they were taller than controls, VC was registered lower than controls. There was no difference in height among football players and controls. It would suggest that although height and age are the most commonly used predictive factors for lung volumes, other factors, including fat free mass (FFM), thoracic diameter and trunk length, may predict lung volume in athletes. It is therefore likely that both anatomical and mechanical factors may account for differences in lung volume.11
A previous study had shown that water polo training for more than 7 years generated growth of ventilatory lung function. Analysis shows that constant long term water polo training in the context of young player's training, the quantity and duration leads easily to measurable improvements in ventilatory lung function, compared to the general population.12,13 Analysing water polo as a sport, it has been shown that it is an ‘intermittent’ sport comprised of intense bursts of activity of <15s duration with intervening, lower intensity intervals averaging <20s duration. Physiological measurements obtained during a game indicate the cumulative effect of repeated sequences of activities and suggest there is a high metabolic demand on the athletes. The multiple individual skills and movements required for playing water polo also place considerable demands on the neuromuscular system.14 In addition, regular swimming practice may tend to alter the elasticity of the lungs and the chest wall which leads to improvement in the lung function.15 Also, the way they perform the activity is different; the load of the water pressure against the chest wall and elevated airway resistance as the result of immersion could constitute a conditioning stimulus as well as the requirement that inspirations must occur rapidly from functional residual capacity during short intervals between strokes. Ventilation is restricted in every respiratory cycle for one moment to next, producing a condition of intermittent hypoxia which is a stimulus to increase respiration. Overall, the respiratory muscles and the diaphragm of the swimmers are required to develop greater pressure as a consequence of immersion in water during the respiratory cycle, thus leading to functionally better respiratory muscles. These factors when combined together play an important role in developing better lung functions in swimmers compared to the other athletes.14–16
Other significantly different parameters are observed in basketball, water polo and rowing (FEV1 was higher, following VC, FVC), PEF was lower in boxing, kayak, rugby, handball, taekwondo and tennis. In terms of body composition, we did not find any significant parameter which could explain lower values, except the percentage of body fat which was the highest in rugby group and could be limiting factor for FEV1. The other possible explanation is the type of respiratory muscle training. Experimental settings have shown that endurance and aerobic training caused significant improvement in PEF as compared to other types of training which is not the case in boxing.10,6 Moreover, the MVV was significantly greater only in boxing, indicating that perhaps the pattern of training (high static and dynamic)11 caused significant improvement in MVV.
It should be taken into account that spirometric values in athletes are derived from reference data from the general population which cannot be used either for elite athletes or for individuals who are engaged in active training process. There is evidence that even mild exercise in the general population may affect lung volumes indices leading to higher FEV1 and FVC but also to lower age-related FEV1 decrease over time.12,17
This finding is even more marked in elite athletes with intense exercise leading to 10–20% higher FEV1 values compared to the general population.18–20
Thus, in athletes normal spirometric values real lung volumes may be understimated and perhaps mask restrictive or obstructive lung disease which may be detected after bronchial dilation test.21 It seems that the creation of spirometric reference values and prediction equations for athletes maybe of value although the effect on the diagnostic accuracy of spirometry in this patient population is unknown.19–21
Myrianthefs P and associates found that ATS/ERS equation significantly overestimated or underestimated spirometric values in a sample of general Greek urban, non-athletic population leading to the misclassification of a significant percentage of individuals.21,22 We can say that our study agrees with the previously mentioned study. However, to explain the difference in the lung volumes in different sports, more extensive and detailed research with each group of players is required.
ConclusionBasketball, water polo and rowers had higher vital capacity, forced vital capacity and forced expiratory volume in one second than the normal sedentary control individuals. The maximum voluntary ventilation was also recorded in water polo and the rowing group. These sports could be recommended for the improvement of the lung function if respiratory parameters were tested on a larger number of participants. Even more so, could water polo and rowing be suggested at an early age, to strengthen the lung function. It should perhaps be considered that these sports or their specific way of training might be involved in pulmonary rehabilitation programmes.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.