Chronic obstructive pulmonary disease (COPD) is a disorder characterized by airflow limitation that is not fully reversible. The severity and magnitude of the symptoms increase as the disease progresses, leading to significant disability and a negative effect on quality of life.1–3 Despite optimal treatment with pharmacological agents, classic pulmonary rehabilitation and oxygen, many patients continue to be symptomatic.3
It is well known that respiration is an essential factor for singing and that this technique involves strong fast inspirations, followed by extended, regulated expirations, which require accurate control of breathing. 1,2,4–6
The objective of this study was to investigate the effects of weekly singing classes on maximal respiratory pressures, spirometric measurements, parameters in six-minute walk test (6MWT), maximum expiration breathing time and health-related quality of life (QoL) in patients with COPD.
Patients with COPD who were attending a maintenance pulmonary rehabilitation program (90min, twice a week) at the Physical Medicine and Rehabilitation Department in Pedro Hispano Hospital were invited to participate in the study. They had to have been diagnosed with COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD). All subjects had to have been in a stable clinical condition for at least 6 weeks before admission to the study and to have signed a written informed consent at their initial visit.
Demographics, height, weight and clinical history were recorded. All patients initially completed plethysmography (FVC, FEV1, FEV1/FVC, TLC and RV); maximal inspiratory and expiratory pressures at the mouth level (MIP, MEP); assessment of QoL employing Saint George's Respiratory Questionnaire (SGRQ), COPD Assessment Test (CAT) and EuroQoL Test; Hospital Anxiety and Depression Scale (HADS); London Chest Activity of Daily Living Scale (LCADL) and Medical Research Council Dyspnoea Questionnaire (mMRC) for dyspnea; six minutes walk test (6MWT) with documentation of time taken to recover oxygen saturation, Modified Borg dyspnea score and heart rate following the test.
Maximum expiration breathing time was always assessed by the same researcher.
The patients were enrolled in weekly classes lasting approximately 1h, for 10 weeks. The classes were coordinated by a singing teacher and a physiotherapist. The patients participated in the classes as a group and the activities included the following:
- (a)
Relaxation exercises of neck and upper and lower limb muscles, conducted by a physiotherapist (10–15min);
- (b)
Vocalization exercises, led by the singing teacher, as a preparation for singing (15min);
- (c)
Singing training for popular Portuguese songs, conducted by the singing teacher (35min).
The songs increased in difficulty as the sessions progressed and the patients were instructed to practice the songs at home during the week.
The final evaluation of the patients was performed after 10 sessions. If episodes of acute exacerbations occurred, the final assessment was performed only after a minimum of 3 weeks of clinical stability.
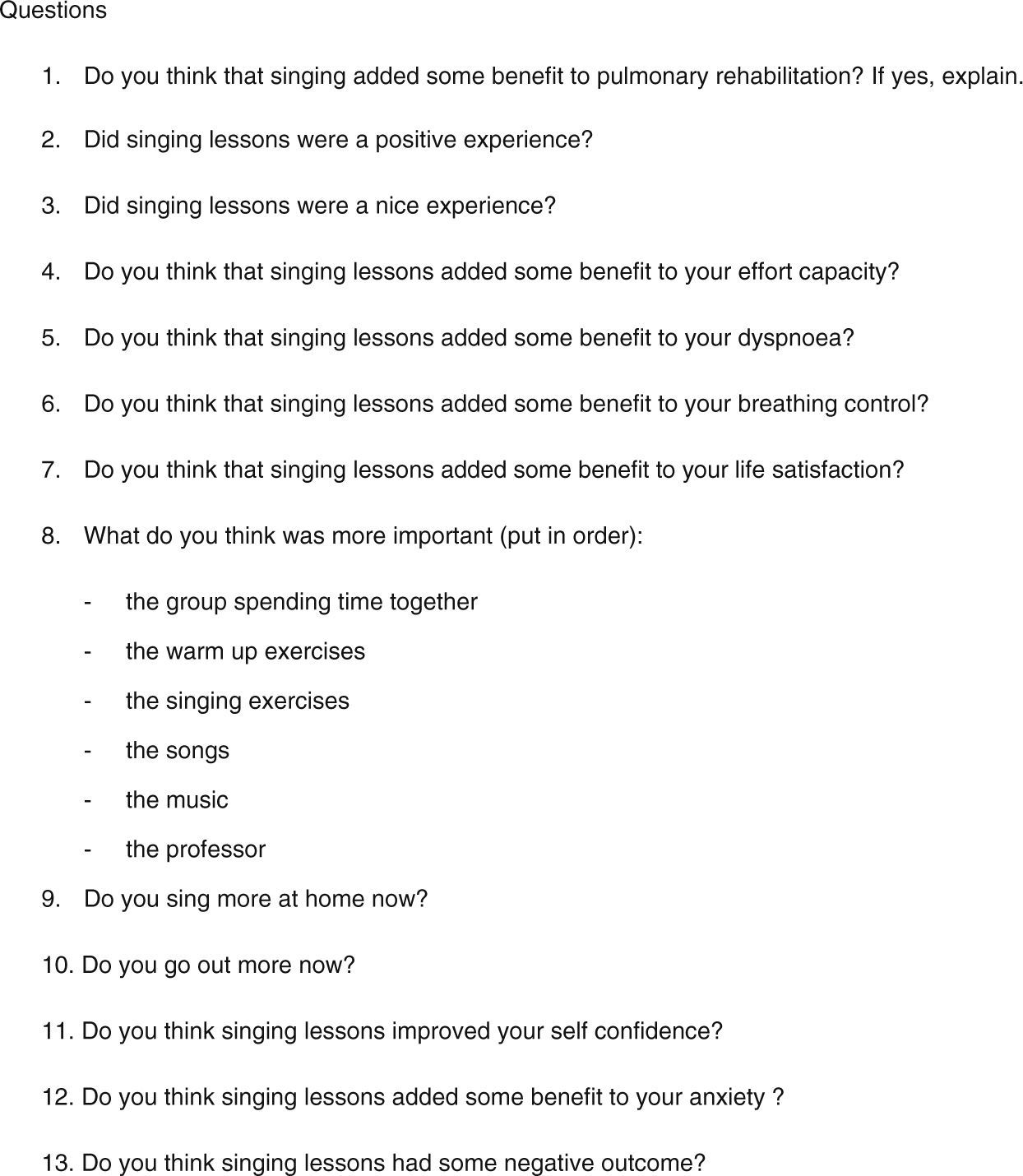
The components of the final evaluation were the same as those for the initial assessment. On final evaluation patients also responded to a questionnaire drawn up by the researchers (Fig. 1).
The study took place between February and May 2013 (10 sessions). Eight patients were selected to participate in the study but two of them were subsequently excluded.
Two patients were dropped from the study because they did not attend at least 7 sessions.
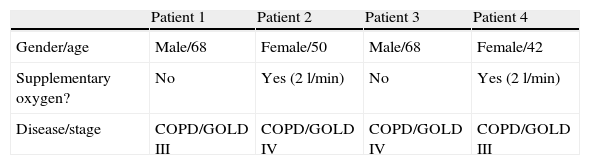
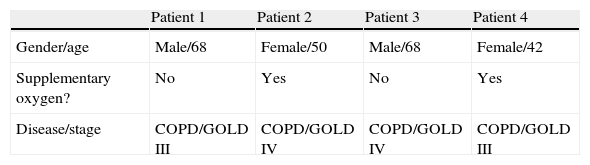
The results are listed in Tables 1 and 2.
Respiratory tests before and after the program.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
| Gender/age | Male/68 | Female/50 | Male/68 | Female/42 |
| Supplementary oxygen? | No | Yes (2l/min) | No | Yes (2l/min) |
| Disease/stage | COPD/GOLD III | COPD/GOLD IV | COPD/GOLD IV | COPD/GOLD III |
| Measurements | Patient 1 | Patient 2 | Patient 3 | Patient 4 | ||||
| BSP* | ASP** | BSP | ASP | BSP | ASP | BSP | ASP | |
| FEV1 (L) | 1.15 (45%) | 1.21 (47%) | 0.84 (33%) | 0.85 (33%) | 0.90 (34%) | 0.87 (34%) | 1.21 (54%) | 1.21 (51%) |
| FEV1/FVC (%) | 59 | 51 | 53 | 50 | 37 | 40 | 67 | 67 |
| TLC (L) | 6.14 (101%) | 5.95 (98%) | 4.72 (96%) | 4.70 (95%) | 9.38 (154%) | 7.66 (126%) | 3.90 (92%) | 3.90 (92%) |
| FVC (L) | 1.97 (59%) | 2.38 (71%) | 1.59 (53%) | 1.71 (58%) | 2.43 (72%) | 2.20 (65%) | 1.81 (66%) | 1.81 (66%) |
| DLCO/Va (mmol/min/Kpa/L) | 95 | 94 | 18 | 16 | 35 | 41 | 79 | 79 |
| RV (L) | 3.95L (163%) | 3.53L (146%) | 3.12 (180%) | 2.99 (171%) | 6.61 (272%) | 5.07 (207%) | 2.10 (143%) | 2.10 (143%) |
| MIP | 75 | 78 | 70 | 48 | 89 | 78 | 63 | 53 |
| MEP | 86 | 88 | 66 | 89 | 97 | 75 | 111 | 121 |
| 6MWT (O2 Sat) | 92 | 93 | 88 | 93 | 85 | 92 | 89 | 88 |
| 6MWT (final Borg dyspnea) | 5 | 4 | 3 | 3 | 6 | 4 | 4 | 4 |
| 6MWT (final HR) | 119 | 105 | 128 | 135 | 105 | 105 | 125 | 120 |
| 6MWT (distance/meters) | 480 | 440 | 360 | 420 | 360 | 459 | 480 | 420 |
| Expiratory time (s) | 14.9 | 12.6 | 14 | 10 | 16 | 13 | 12.5 | 8.5 |
FEV 1: forced expiratory volume in 1s; FVC: forced vital capacity; TLC: total lung capacity; DLCO/Va: ratio between carbon monoxide diffusing capacity to alveolar volume; RV: residual volume; MIP: maximal inspiratory pressure; MEP: maximal expiratory pressure; 6MWT (O2 Sat): oxygen saturation at the end of six minutes walk test; 6MWT (Final Borg Dyspnea): Modified Borg scale for dyspnea at the end of six minutes walk test; 6MWT (Final HR): heart rate at the end of six minutes walk test; 6MWT (distance/meters): distance traveled at the end of six minutes walk test.
QoL questionnaires before and after the program.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
| Gender/age | Male/68 | Female/50 | Male/68 | Female/42 |
| Supplementary oxygen? | No | Yes | No | Yes |
| Disease/stage | COPD/GOLD III | COPD/GOLD IV | COPD/GOLD IV | COPD/GOLD III |
| Measurements | Patient 1 | Patient 2 | Patient 3 | Patient 4 | ||||
| BSP* | ASP** | BSP | ASP | BSP | ASP | BSP | ASP | |
| SGRQ | 19 | 17 | 22 | 27 | 41 | 49 | 44 | 40 |
| CAT | 22 | 19 | 14 | 16 | 22 | 23 | 10 | 25 |
| EuroQoL | 7 | 8 | 7 | 8 | 11 | 9 | 28 | 10 |
| mMRC | 1 | 1 | 2 | 2 | 4 | 3 | 2 | 3 |
| HADS anxiety | 7 | 6 | 7 | 7 | 3 | 4 | 10 | 10 |
| HADS depression | 3 | 1 | 4 | 6 | 2 | 6 | 8 | 5 |
| LCADL | 13 | 17 | 21 | 22 | 19 | 26 | 36 | 33 |
SGRQ: St. George's Respiratory Questionnaire; CAT: COPD Assessment Test; EuroQoL: questionnaire to measure health status; mMRC: Modified Medical Research Council Dyspnea Scale; HADS Anxiety: Hospital Anxiety and Depression Scale, punctuation for anxiety; HADS Depression: Hospital Anxiety and Depression Scale, pontuation for Depression; LCADL: London Chest Activity of Daily Living Scale.
Despite the small number of patients it is possible to observe that the FEV1 improved from 1.15L (45%) to 1.21L (47%) for Patient 1, remained the same in Patients 2 and 3 (33 and 34%) and got worse in Patient 4 (54–51%).
No significant differences were observed in relation to residual volume (RV) and total lung capacity (TLC). In terms of maximum expiratory pressures (MEP) we found an improvement after singing lessons in only three of the patients. Patient 3 was the only patient who experienced a COPD exacerbation during study time and was the only patient not to improve MEP.
When analyzing the results for the 6-minute walk test (6mWT) we observed an increase in the distance travelled by Patient 2 and Patient 3 (60m for Patient 2 and 99m for Patient 3) and a decrease for Patient 1 and 4. Only Patient 4 had final oxygen saturations below 90% when the test was performed after the singing lessons (before the program only three patients had oxygen saturation below 90%). The expiratory time decreased in all patients tested.
In terms of quality of life questionnaires (Table 2) we found that there were no major differences between the pre- and post-singing session results.
When analyzing the answers to the questionnaire prepared by the researchers we found that all patients reported improvement in lung function control, reduced anxiety and more self-esteem after the singing lessons. In addition, all patients reported a feeling of well-being and recorded the experience as very pleasant.
The aim of the singing lessons was to improve the quality of life in patients with moderate and severe COPD, by helping them to control daily symptoms that interfere with their quality of life, as suggested in the literature.
Functionally MEP tended to improve MEP, as observed in other studies1 but these results cannot be considered valid given the low number of patients and the lack of a control group. The expiratory time decreased in all patients tested.
Despite their not having ticked major differences in quality of life questionnaires, the singing program was perceived by patients as a pleasant experience, which is similar to the results found in the literature.2,5,6
All patients said that the project should be continued and expanded.
The present data2,4 and this study suggest that singing does produce specific benefits and that participation in singing classes should be encouraged where these are available.
We extend our thanks to the singing teacher Vitor Manuel da Silva Sousa for making himself so available and his help in building, implementing and finalizing this project, which otherwise would not have been achieved.