Solitary fibrous tumor of the pleura (SFTP) is a rare tumor originating in mesenchymal cells; it represents less than 5% of all pleural tumors.1 It is generally benign but 10–30% of SFTP are malignant.2
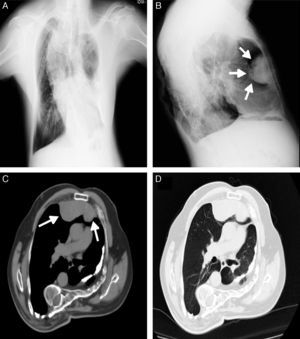
We report the case of a 61 year-old man, with a past history of bronchiectasis and severe restrictive ventilatory defect due to thoracic scoliosis (Fig. 1 A), who came to the pulmonology outpatients department with complaints of asthenia over the last year. He was an occasional pipe smoker and the physical examination showed marked thoracic deformity which limited chest expansion. A chest X-ray showed a large retrosternal opacity (Fig. 1B) and the chest computed tomography (CT) confirmed the presence of a retrosternal lobulated mass, 10.2cm×3.7cm, in the right hemithorax (Fig. 1C and D). A percutaneous CT-guided biopsy was carried out and the histology showed evidence of mesenchymal neoplasm without necrosis, significant pleomorphism or mitotic figures. The tumor cell population stained diffusely for CD 34, vimentin, bcl-2 and CD 99 and negative for S-100. Ki-67 was <5%. Although a benign SFTP was diagnosed based on the histology, a right thoracotomy was performed for diagnosis and treatment. A pedunculated tumoural mass was complete resected with segmental resection of the right upper lobe. Immunohistochemistry showed positivity for CD-34 and bcl-2 confirming SFTP. The pathological examination revealed multiple mitotic figures (12 mitoses per 10 high-power fields), mild pleomorphism, hypercellularity, focal hemorrhage and several areas of necrosis and the resection margins were tumor-free. According to these features the tumor was classified as malignant. The post-operative period was uneventful and the patient was discharged home. The patient is now in the third month after surgery without any sign of local recurrence or metastization.
SFTP is a rare tumor with generally an indolent course and good prognosis with a 10-year survival rate up to 98%.3 It occurs mainly in individuals in their sixth or seventh decades of life without gender bias. There is no association with tobacco, asbestos or other exposures. More than 50% of the patients are asymptomatic4 and the tumor is frequently an incidental finding on a routine chest X-ray. When symptomatic, the patients usually present non-specific respiratory symptoms such as dyspnea, cough and chest pain, and more rarely systemic symptoms. Occasionally, SFTP can manifest as paraneoplastic syndromes, such as hypertrophic pulmonary osteoarthropathy (Pierre Marie-Bamberger syndrome) and refractory hypoglycemia (Doege-Potter syndrome). The frequency of these syndromes increases with tumor size.
Malignant SFTP is uncommon and its incidence varies from 7% to 60%. It rarely arises from a pre-existing SFTP undergoing malignant transformation. The role of percutaneous CT-guided biopsy is not yet established because its diagnostic accuracy is low5 and it can underestimate the degree of malignancy given the size and histological heterogeneity of these tumors. Therefore, a pre-surgical diagnosis should not affect the decision to perform surgery for benign and malignant SFTP. According to the world Health Organization Classification for soft tissue tumors, the malignant SFTP is diagnosed if one or more of the following histologic features are present: hypercellularity, pleomorphism, tumor necrosis, more than 4 mitoses per ten high-power fields and infiltrative margins. Immunohistochemistry may be useful in differentiating the SFTP from mesotheliomas and intrapleural sarcomas. Generally SFTP is vimentin, CD34, CD99 and bcl-2 positive and cytokeratin negative.
Complete resection of tumor is the treatment of choice, the only demonstrated effective treatment and the most important prognostic factor.6 The choice of surgical approach (video-assisted thoracoscopic surgery (VATS) and standard thoracotomy) is essentially based on tumor size and the difficulty of removal. The role of adjuvant radio and chemotherapy in malignant SFTP remains unclear since there is no systematic assessment due to the rarity of the tumor. Despite this, there are some reports showing good response to adjuvant radiotherapy in tumors with incomplete resection.6 Recurrence rates for completely resected malignant SFTP range from 14% to 63%4 in pedunculated and sessile tumors, respectively, and occur mainly in the first 24 months after surgery. Despite a complete resection, malignant SFTP can have a poor prognosis with a 5-year rate survival of 45,5%.5 Recurrent tumors should be resected and combined chemotherapy with temozolomide and bevacizumab can be considered in locally advanced, recurrent or unresectable malignant SFTP.7
We report a case of a malignant SFTP, a rare pleural tumor that although completely resected and potentially with good prognosis, should have long-term follow-up due to the high risk of local and metastatic recurrence.
Conflicts of interestThe authors have no conflicts of interest to declare.