Aspergillus fumigatus (AF) might lead to a range of pulmonary spectrum of diseases. These include allergic bronchopulmonary aspergillosis (ABPA), aspergilloma, chronic cavitary pulmonary aspergillosis and invasive aspergillosis.1 Despite the fact that Aspergillus colonization rate in cystic fibrosis (CF) can be up to 60%, invasive aspergillosis is considered a very rare complication.2–5 The authors describe a case of a CF patient with ABPA, whose disease progressed to subacute invasive aspergillosis.
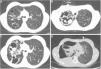
The patient was a 20-year-old female with CF (F508del/F508del) diagnosed at age 3. She presented with lung and sinus involvement characterized by cystic, cylindrical and varicose bronchiectasis more prominent in right upper lobe (Fig. 1A), severe obstructive ventilatory defect (FEV1 41%), chronic colonization by methicillin-sensitive Staphylococcus aureus, AF and Candida spp. in repeated sputum cultures, as well as chronic sinusitis and nasal polyposis. The patient had a history of recurrent hospitalizations due to haemoptysis, some requiring embolization. She also had exocrine pancreatic insufficiency, poorly controlled diabetes, hepatic cirrhosis and presented undernourished (IMC 17.5kg/m2).
(A) Thoracic CT undertaken in 2010, where are identifiable cystic and cylindrical bronchiectasis more prominent in the right side. (B, C) Thoracic CT during hospitalization of the patient in 2011, showing pulmonary thick-walled cavities, with some material within the cavity, and also multiple new scattered nodular opacities, as well as some peripheral pleural based areas of consolidation. (D) Right sided hydropneumothorax.
At the time of transfer to the adult clinic, there was evidence of increasing values of total immunoglobulin (Ig) E (between 387 and 790IU/mL) and elevated specific IgE (5.5IU/mL) and IgG (116 mgA/L) to AF, as well as the presence of precipitins to AF. Despite these values, the patient remained clinically stable, without lung function decline or worsening of arterial blood gas values or recent changes in chest X-ray. Taking this into account and due to the high risk of diabetes decompensation and hepatotoxicity, it was decided against corticosteroid or antifungal treatment. She was started on a pulmonary rehabilitation program in hospital and was referred for evaluation for lung and liver transplantation. After 1 year, the patient was admitted to the pulmonology ward, complaining of cough worsening, increase in sputum volume and purulence, dyspnea, bloody sputum and fever, which had evolved over 4 weeks. It was at this stage that occurred the first isolation of Pseudomonas aeruginosa from sputum culture, which led to IV tobramycin and ceftazidime. Pseudomonas aeruginosa, AF and Aspergillus flavus persisted to grow in sputum. Meanwhile, she underwent bronchial embolization due to haemoptysis. On day 7, the patient developed pleuritic chest pain, with evidence of worsening of pulmonary opacities in chest X-ray and a significant increase in total IgE (1378IU/mL) and specific IgE (9.15IU/mL) and IgG (>200 mgA/L) to AF. Treatment for ABPA exacerbation was started with oral prednisolone (1.5mg/kg) and itraconazole (5mg/kg). After initial improvement, she presented clinical worsening, recurrence of fever and development of new cavities and nodular opacities on CT (Fig. 1B and C). Therefore vancomycin was added, the antifungal was switched to IV voriconazole and prednisolone dose reduced, allowing for the diagnosis of sub-acute invasive aspergillosis. However, she continued to deteriorate and developed a right-sided hydropneumothorax (Fig. 1D) and died the following day.
At present, when dealing with CF, the diagnosis of pulmonary aspergillosis syndromes may be challenging, because of the overlapping clinical and radiological features.3,4 Most frequently associated to CF is Aspergillus colonization and the development of ABPA.2–4 CF patients rarely develop invasive forms of aspergillosis, but disseminated aspergillosis has been occasionally described complicating ABPA.3–5 Although each entity will have distinct risk factors, the occurrence of Aspergillus overlap syndromes are increasingly being recognized.3–5 In the present case, the patient was admitted with a condition suggestive of an infective exacerbation of CF, which was treated with broad spectrum antibiotics. However, the clinical deterioration presented and poor response to antibiotics, in conjunction with serological data, led to the decision to treat her for ABPA exacerbation with oral prednisolone and itraconazole, according to recommendations.2 Despite this, the patient developed radiological features suggestive of subacute invasive aspergillosis and so the diagnosis of subacute invasive aspergillosis was assumed based on clinical, radiological and serological criteria, since the patient did not present conditions for invasive procedures. Although invasive pulmonary aspergillosis usually occurs in severely immunocompromised patients, in this case, the corticosteroid treatment, immunosuppression related with diabetes and malnutrition as well as underlying chronic lung disease could together indicate predisposition for invasive aspergillosis. In the few other reported cases of CF patients with ABPA who developed invasive aspergillosis, most of them relate to patients who were under corticotherapy for ABPA and the majority had also an adverse outcome.3–5 However, there is no clear definition of the dose and duration that enables the identification of patient who are at risk. With this case, the authors intend to emphasize that invasive aspergillosis, despite being rare in CF patients with ABPA, may be a life-threatening complication. A high level of clinical suspicion is necessary for early recognition and appropriate treatment of this condition, which may consist of broad antifungal coverage, to prevent a poor evolution or long term lung damage.
FundingThe authors declare that no funding was received for this paper.
Conflicts of interestThe authors have no conflicts of interest to declare.