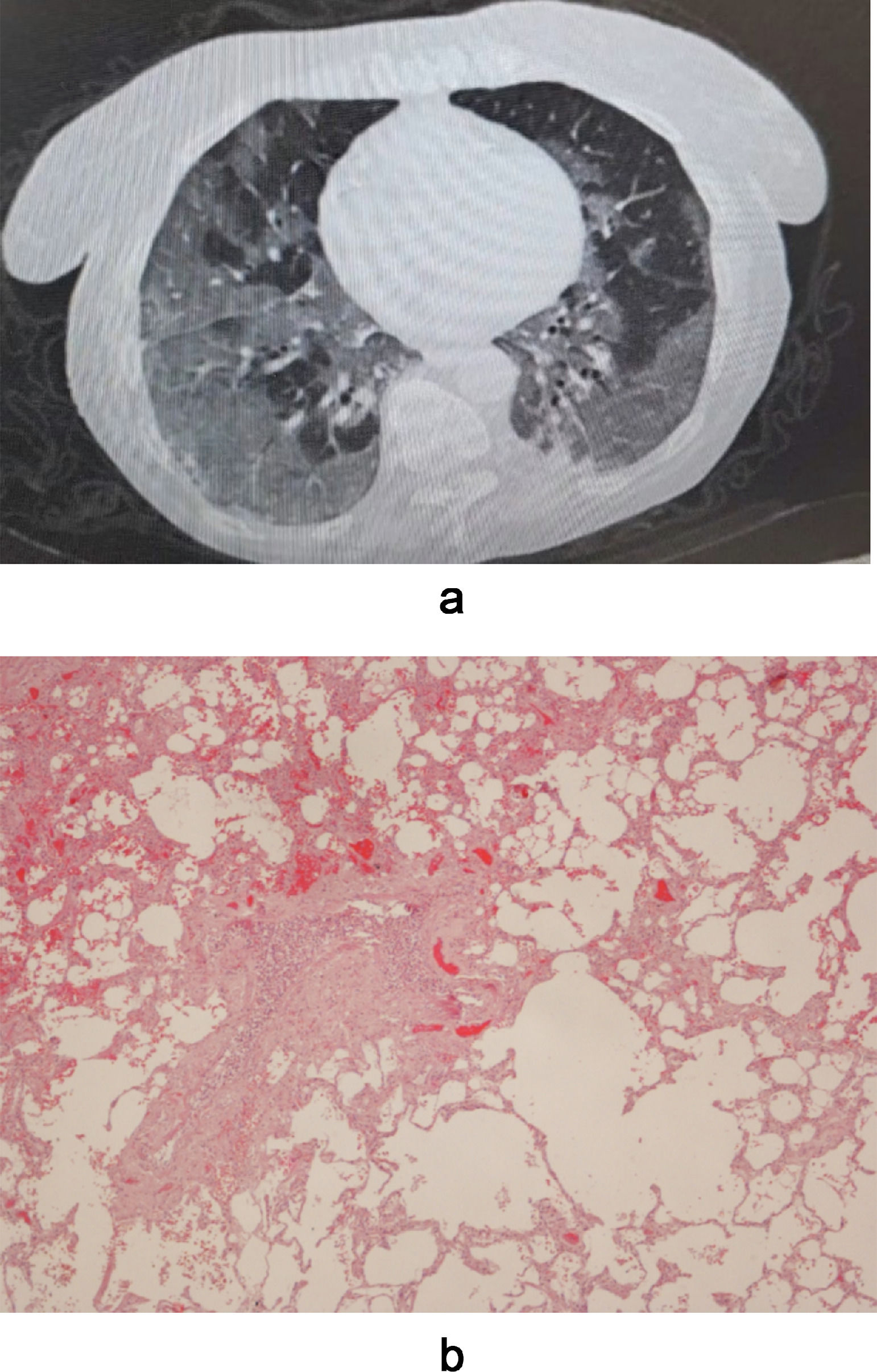
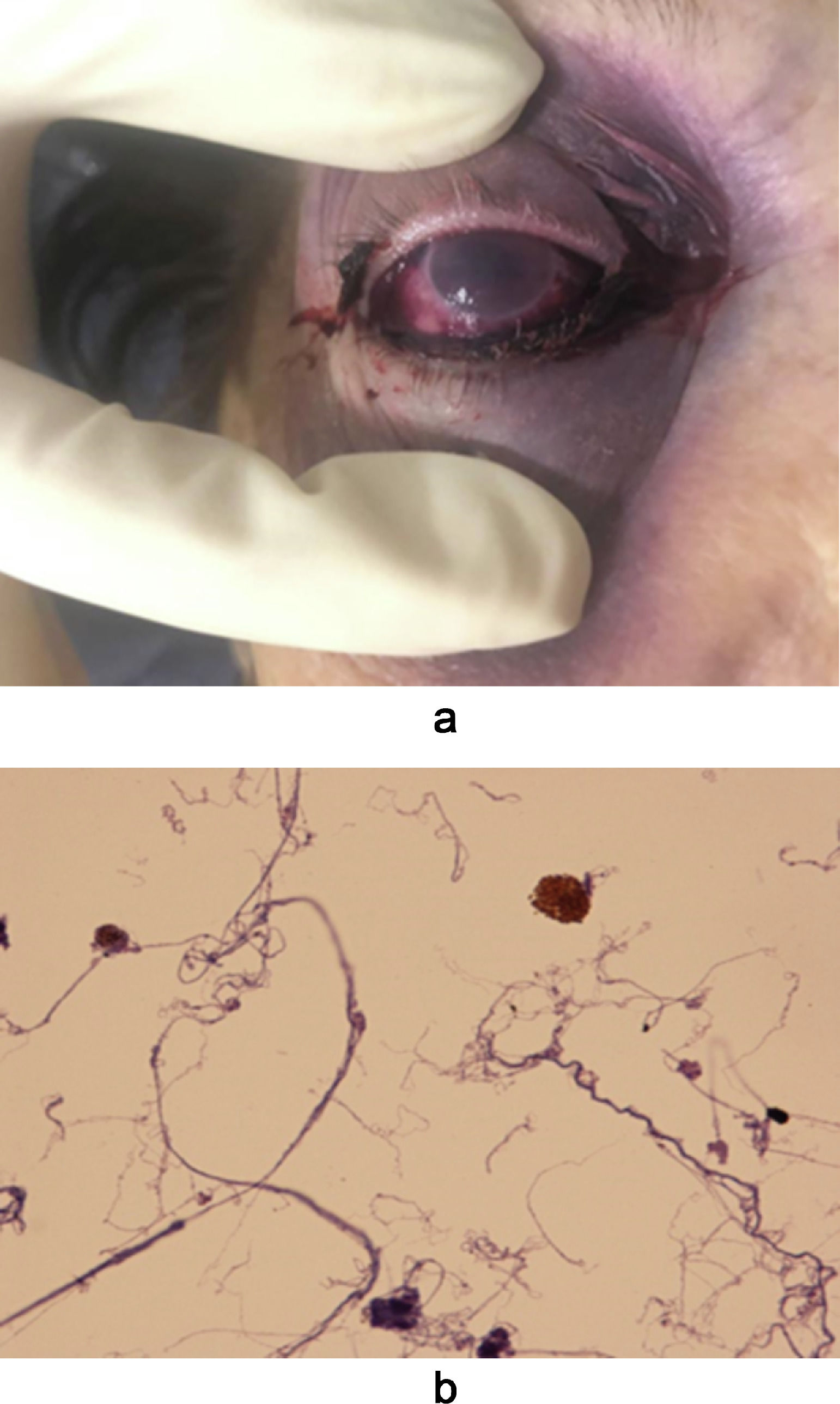
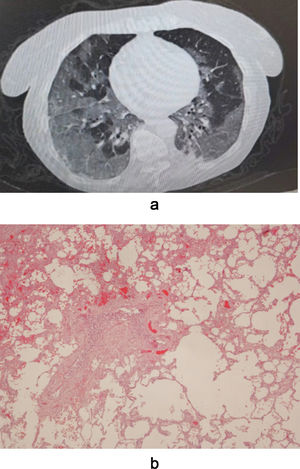
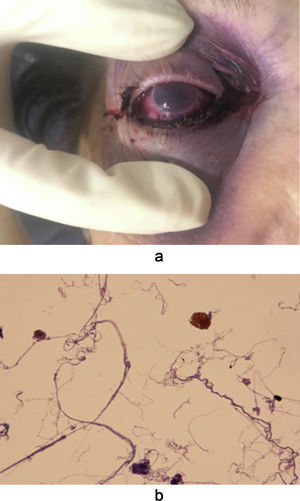
Noninvasive ventilation (NIV) and prone-positioning (PP) are life saving measures in patients with moderate COVID-19 related ARDS.1-5 Risks related to the use NIV interfaces and PP are already individually described in literature.6-8 To the best of our knowledge, in this case of a 86 year-old woman we are the first to describe the complication related to the combined use of PP and NIV via an oro-nasal mask interface. Informed written consent to publication of her clinical data was obtained from the patient's next of kin. The patient had refused COVID-19 vaccination and in November 2021 she tested positive for SARS-CoV2 infection via rapid antigen test. She was admitted after three days to the Emergency department (ED) of Bari University Hospital with persistent fever, dizzy cough and dyspnoea despite having received oral prednisone (50 mg/die), and azithromycin 500 mg/daily at home. She was rapidly escalated from conventional oxygen therapy to High Flow Nasal Oxygen (HFNC) set at 60 litres/minute, 31°C, with an oxygen fraction (FiO2) of 70% for desaturation on venturi mask. Arterial blood gas test on HFNC showed a PaO2 and FiO2 ratio (P/F) of 114. Chest X-ray showed bilateral infiltrates. According to the Berlin definition, moderate ARDS was diagnosed. Due to her old age and comorbidities, no indication for intubation was granted by ICU physician, and she was admitted to the Respiratory Intermediate Intensive Care COVID-19 Unit (RICU). CT scan confirmed bilateral lungs ground-glass opacities and middle and lower lobes subpleural consolidations (Fig. 1A). During 2nd day in RICU, the patient was switched to NIV due to increasing dyspnea, respiratory rate and use of accessory muscles. Pressure Support Ventilation (PSV mode) was started at 8 cmH2O above 11 cmH2O of positive end expiratory pressure (PEEP) using a ventilator in intentional leak configuration (V60, Philips; Respironics,USA). An 8- hour rotational interface strategy was started using either a “non-vented” oro-nasal masks (PerformaTrak Philips; Respironics,USA or Flexifit 431-Fisher&Paykel) while in lateral-positioning and “non-vented” full-face mask (PerforMax NOCTN111Respironics USA) while supine. The rationale behind the use of “non vented” interfaces was to allow the use of a heat and moisture exchanger (HME) antiviral filter to provide humidification and avoid operator contamination. HME was connected to the dedicated intentional leak circuit of the ventilator equipped with a “vent system” proximal to the HME9-10 Since the patient was not compliant with full PP, lateral-positioning was started up to 16 hours a day using the oro-nasal mask with sessions lasting not more than 4-6 hours. Furthermore, to allow prolonged ventilation light conscious sedation using a continuous infusion of dexmedetomidine (up to 0.5 mcg /kg /h) was started. On day 5 a right eye periorbital redness with a small periorbital hematoma was observed. The NIV was stopped and HFNC was resumed at prior setting but at FiO2 of 0.90 to guarantee an oxygen saturation ≥ 90%. Despite maximal medical treatment, the patient died of multi-organ failure on day 10. Autopsy was performed and reported among other things were the following remarks: COVID-19 infection, bilateral lung pneumonia and emphysema (Fig. 1B), bruising of the right eyeball (Fig. 2A). Moreover, on deep eye examination, a considerable right periorbital oedema and an extensive haemorrhagic hematoma was described. Optical microscopical evaluation of the eyes and lung layers cytology was also performed showing a haemorrhagic humour vitreous from the anterior eye chamber (Fig. 2B); while the lung showed areas of emphysema, haemorrhagic infarctions, and diffuse alveolar damage with presence of hyaline membranes.
A. Bilateral ground glass opacities in subpleural position and little consolidations in both lower lobes. B. An optical microscopical vision of layer histology of the lung showing diffuse vascular congestion, fibrotic replacement of lung parenchyma and emphysema. Diffuse alveolar damage with hyaline membranes is also present.
This is the first report of prolonged lateral-positioning and haemorrhagic trauma of the orbital cavity during NIV We hypothesise that these findings could be the result of several causes: first, the use of a oro-nasal mask instead of a total full-face mask which includes the eyes; second, the displacement of the interface into the right eye due to the lateral-positioning which caused pressure to be concentrated in the right eye and inner corner of the nose; third, the light sedation administered could have prevented the patient from feeling the interface discomfort; lastly, the low weight molecular heparin (LWMH) treatment could have predisposed the patient to bleeding. Thus, all these causes might have been responsible for the bleeding around eye globe and into the right eye chamber. It could be argued that the mask was too tight but interestingly the patient did not show any sign of nasal bridge sore which is a well-recognised site of skin breakdown.6-8 Eyes complications associated with PP are not a novelty in intubated patients, but there is a paucity of data regarding eye trauma in NIV.11 Moreover, eye protection it is not easy in spontaneous breathing awake patients for several reasons including the patient's feeling of blindness and the risk of causing damage during the spontaneous opening/closing of the patient's eyes. One could also argue that a helmet or a total-face mask should have been used in this context.12 While the first was not available in our institution, the second one was used in supine position because it was often displaced during lateral-position causing uncontrollable air leaks which decreased ventilatory assistance and increased the risk of contamination.9 Therefore, an oro-nasal interfaces was used in lateral-position.
In conclusion, we describe the ocular trauma related to the combined prolonged NIV use via an oro-nasal interface and lateral-positioning of a patient affected by COVID19 severe ARDS. Great caution should be taken with these patients due to the potential onset of side effects “The eye may be the spy of interface/NIV related injury”.