It is a widely held view that messenger RNA (mRNA) COVID-19 vaccines, including mRNA-1273 (Moderna) and BNT162b2 (Pfizer-BioNTech), effectively reduce the risk of SARS-CoV-2 infection and COVID-19-related hospitalization. Unexpectedly however, despite the protective effects of those vaccines, as many as 25% of the individuals currently being admitted to Intensive Care Units (ICUs) are fully vaccinated against COVID-19.1,2 It is hypothesized that as vaccine coverage increases, breakthrough cases will rise proportionately.
Chest X-ray scoring systems quantifying the severity and monitoring the progression of the disease were developed during COVID-19 outbreak. Retrospective studies investigating their prognostic accuracy have demonstrated that these systems help predict mortality in patients with COVID-19.3,4 Notably, the COVID-19 chest radiography (CARE) score, a chest radiography rating system which assesses the extension of the ground-glass opacities (GGs) and consolidations (Cos) in three distinct radiograph zones (upper, middle, and lower lung), has been validated and has predicted in-hospital mortality.5
While recent evidence suggests that mRNA vaccinations may attenuate disease severity in breakthrough COVID-19 patients requiring hospitalization,7,6 its impact on critically ill patients receiving non-invasive respiratory support (i.e., high-flow nasal oxygen, or continuous positive airway pressure, or noninvasive ventilation) remains unclear. The current study set out to retrospectively investigate the effect of mRNA vaccination on the extent of lung involvement as assessed by the CARE score in breakthrough COVID-19 patients receiving high-flow nasal oxygen (HFNO) because of severe hypoxemic acute respiratory failure (hARF) that was unresponsive to conventional O2–therapy. The patients studied were admitted to an Intermediate Respiratory Care Unit (IRCU).
The chest X-rays (CXRs) of 32 consecutive, fully vaccinated patients (the vaccinated group) and of 41 unvaccinated patients (the unvaccinated group), all critically ill and affected with COVID-19, admitted to the SARS-CoV-2 IRCU of the University-City Hospital in Padua between 1 September 2021 and 31 December 2021 were retrospectively reviewed. The criteria for admission to the IRCU was the inability of conventional O2-therapy to maintain SaO2 ≥ 92%. All the patients meeting these criteria were contacted and asked to sign informed consent forms releasing their medical records for review. The need for ethical approval was waived by the local Ethics Committee given the study's retrospective design and the fact that the unit's standard treatment protocol was consistently followed for all the patients involved.
All of the CXRs taken during the patients’ RICU stay were reviewed. The severity of lung involvement was evaluated using the CARE score. A radiologist with 12 years of experience in thoracic imaging and blind to the patients’ information examined the CXRs and scored them using the CARE system. The patients’ scores at the time of their admission, their highest score during their IRCU stay, and their highest GG and Co sub-scores were reviewed and compared.
The patients’ baseline demographic and clinical features, clinical symptoms and laboratory test results at the time of their IRCU admission and their clinical outcomes were likewise reviewed and compared.
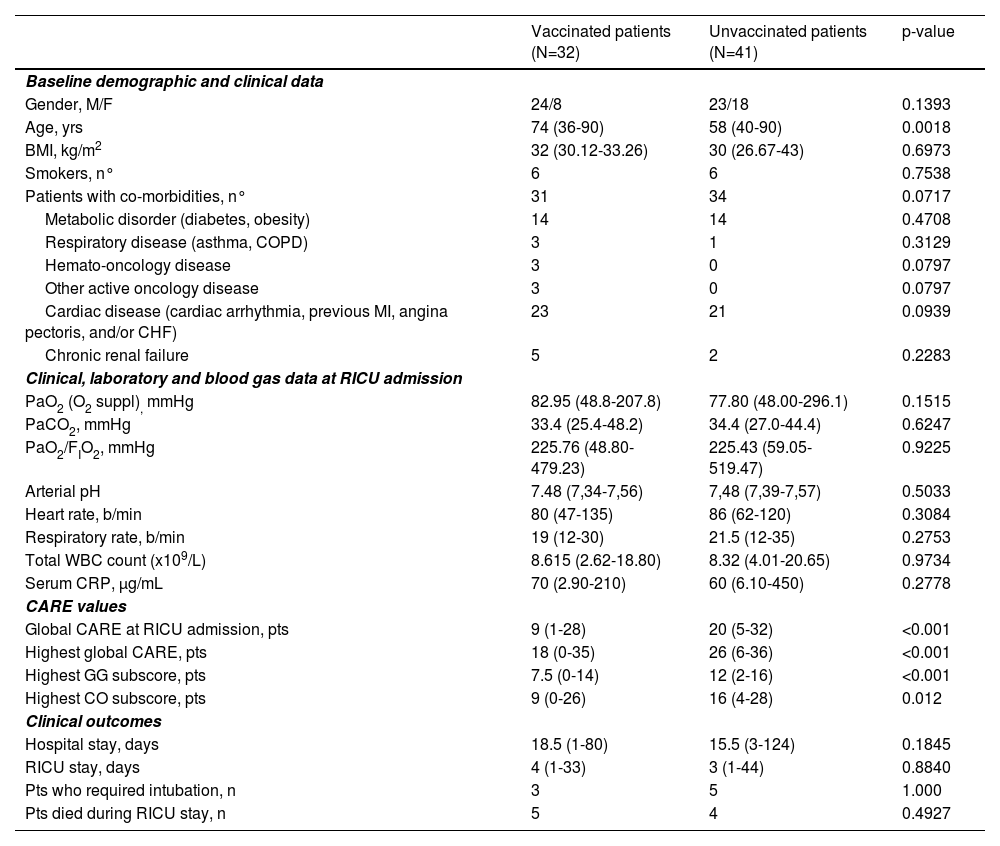
All of the patients in the vaccinated group had successfully completed the COVID-19 mRNA vaccination course, meaning two standard doses of the Pfizer-BioNTech COVID-19 vaccine; none of them had received a booster dose. The mean time interval between the last vaccine dose and admission to the IRCU was 5.86 (0.9-8.8) months. Genomic sequence analysis, performed only in the vaccinated patients, identified, without exemption, the SARS-CoV-2 delta variant. With the exception of age, the baseline characteristics and clinical and laboratory data of the patients at the time of admission to the IRCU were not significantly different in the two groups. The patients in the vaccinated group were, in fact, significantly older [74 (36-90) vs 58 (40-90) yrs; p=0.0018]. The CARE score at the time of IRCU admission, the highest score during their IRCU stay, as well as the highest GG and Co sub-scores were significantly worse in the unvaccinated group. The clinical outcomes of the patients in the two groups were not significantly different (Table 1). The stratified log-rank test indicated that the vaccinated patients had slightly longer survival times in relation to their unvaccinated counterparts [mean survival time: 95.53 (95%CI, 80.76 to 110.30) vs 83.22 (95%CI, 75.82 to 90.61) days; p= 0.2261]; their hazard ratio of death was 0.5174 (95% CI, 0.1780 to 1.5039).
Patients’ baseline demographic and clinical characteristics, clinical, laboratory and blood gas data at RICU admission, CARE values and clinical outcomes.
Values are expressed as median (interquartile range). P-values refer to differences between vaccinated and unvaccinated groups. (BMI= Body Mass Index; CARE= COVID-19 chest radiography score; CO= consolidation; CRP= C-Reactive Protein; GG= Ground Glass; MI= myocardial infarction; RICU= Respiratory Intensive Care Unit; WBC= White Blood Cell).
An analysis of the study's data suggests that mRNA vaccination conferred a protective effect on the extent of lung involvement in the breakthrough COVID-19 patients with severe hARF requiring HFNO treatment. The study's results are in line with those described by Lee et al. who, on the basis of the clinical and imaging characteristics of 412 hospitalized COVID-19 patients, concluded that those with COVID-19 breakthrough infections had a significantly higher proportion of CT scans without pneumonia with respect to their unvaccinated counterparts.8
While the CARE scores of the vaccinated patients were significantly lower, the PaO2/FIO2 ratio, a widely used indicator of hypoxemia reflecting the extent of acute lung damage, was not significantly different in the two groups. The result could be explained by the fact that although hypoxemia caused by the SARS-CoV-2 infection is primarily due to the ventilation/perfusion (V/Q) mismatch in non-aerated lung regions (something which can be assessed by the CARE score), in 3 out of the 32 vaccinated patients it was associated to submassive pulmonary embolism, a disorder that cannot be accurately assessed by the scoring system.
Since the individuals in the vaccinated group were significantly older, it is possible that the vaccination's protective effect on mortality risk may have been offset by the age difference between the vaccinated and unvaccinated groups. A recent analysis by Italian investigators confirmed, in fact, that old age was by far the most significant risk factor for COVID-19 mortality in hospitalized patients.9
While it is true that the limited number of patients analyzed here and the study's retrospective nature may have caused a bias, its findings demonstrate that mRNA vaccination may exert a protective effect on pulmonary involvement in the breakthrough COVID-19 patients undergoing HFNO for severe hARF and confirm the importance of a judicious, mass vaccination strategy.