Reduced heart rate variability (HRV), a marker of autonomic system dysfunction, has been reported in patients with chronic obstructive pulmonary disease (COPD). Yet, limited data exists on the reliability of HRV measurement in this population. Here we investigated the reliability of short-term HRV measurement performed during spontaneous breathing in patients with COPD.
MethodsThirteen individuals (8 males) with moderate-to-severe COPD (FEV1 46±16% predicted; FEV1/FVC 49±13) underwent standard time and frequency domain HRV measurements derived from 5-minute electrocardiograms collected on two separate days using a SphygmoCor device. Absolute and relative reliability was assessed by a number of coefficients including within-subject random variation, systematic change in the mean, and retest correlations.
ResultsWithin-subject coefficients of variation (CV) ranged from 4.3% to 193.4%. The intraclass correlation coefficients (ICCs) ranged from 0.72 to 0.93 for parameters related to overall HRV, and from 0.57 to 0.59 for those related to parasympathetic tone in both time and frequency domains. Mean heart rate was the only parameter that showed excellent absolute and relative reliability (CV=4.3%, ICC=0.93).
ConclusionThe HRV measurements showed overall moderate-to-substantial reliability during spontaneous breathing in COPD population. Our findings support the use of HRV parameters for diagnosis and cardiac risk assessment, but only mean heart rate can be used reliably for monitoring changes in autonomic status following rehabilitation intervention in this population.
Cardiovascular disease is a common comorbidity in patients with chronic obstructive pulmonary disease (COPD).1 Autonomic system dysfunction, through sympathetic nervous overactivity, may play an important role in the initiation and progression of cardiovascular disease in this population.2 Reduced heart rate variability (HRV), a marker of autonomic dysregulation and a significant predictor of cardiac events,3 has been reported in patients with COPD.4 Therefore, monitoring HRV changes with various interventions in this population may be useful to assess their cardiovascular risk profile.
Aerobic exercise training, such as during pulmonary rehabilitation program, has the potential to influence HRV in COPD patients.5 However, measuring HRV for cardiac risk stratification or evaluation of rehabilitation program effectiveness in improving cardiac autonomic function has not yet been implemented clinically. Possible explanations for this delay are related to the complexity of HRV analysis and the instability of this measurement under various psycho-physiological conditions, which may limit its reliability.6
To the best of our knowledge, there is only one study investigating HRV measurement reliability in patients with COPD.7 Despite reporting good measurement reliability, the study employed a limited number of HRV parameters and statistical analyses to be of use for making clinical decisions. Moreover, the HRV measurement was performed under controlled respiratory rate – a procedure that is not always feasible, or requires prolonged training, in patients with more severe COPD who are those commonly referred for pulmonary rehabilitation. Therefore, we conducted this study to examine the test–retest reliability of HRV measurement from short-term electrocardiogram (ECG) recording performed during spontaneous breathing in individuals with moderate-to-severe COPD.
MethodsStudy design and populationThis study used a within-subject repeated measure design, and was conducted in an outpatient Pulmonary Rehabilitation Clinic. The study population included seventeen subjects over 50 years of age, with a physician diagnosis of COPD confirmed by clinical and GOLD spirometric criteria, in stable lung and cardiac condition (e.g., without respiratory infection or hospitalization of pulmonary or cardiac causes as well as without changes in their medication during the preceding month entering the study). The exclusion criteria were cardiac dysrhythmia, cardiac pacemaker, valvular disease, and conditions that would preclude lying supine in a relaxed position. The study was approved by the Research Ethics Board at University of British Columbia and all participants provided written informed consent.
Study procedureResting HRV data were collected on two visits within one week. Testing sessions were conducted at the same time of day (∼9:00a.m.) with the participants lying supine in a quiet and temperature controlled room, and following a rigorous standardized protocol. All participants were instructed to avoid heavy exertion for a minimum of 24h, and to refrain from taking any medication, smoking, eating, drinking alcohol and beverages containing caffeine for at least 12h before testing; conditions that could easily be achieved in clinical practice.
Prior to the initiation of the HRV measurement, patients’ characteristics including hemodynamic parameters were collected. Then, the experimental procedure was described and patients were asked to relax, breathe normally, and refrain from moving, talking, or sleeping during the procedure. A 3-lead ECG was attached to the participants’ chest in the lead II configuration, and they were left to rest in the supine position for ten more minutes before the ECG recordings were performed.
HRV measurementTime and frequency domain evaluations of HRV were obtained from short-term five-minute ECG recording performed during spontaneous breathing using a SphygmoCor® CPV device (AtCor Medical, Inc., USA). One recording was obtained at each visit.
Three time domain HRV parameters were analyzed: mean heart rate, standard deviation of normal to normal R–R intervals (SDNN), and square root of the mean squared difference of successive normal to normal R–R intervals (RMSSD). The mean heart rate and SDNN are considered to reflect both sympathetic and parasympathetic activity, while the RMSSD represents primarily the parasympathetic or vagal influences.3
Three frequency domain HRV parameters were analyzed: low-frequency (LF, 0.04–0.15Hz), high frequency (HF, 0.15–0.4Hz), and total power (TP, 0–0.5Hz). The LF power is considered to reflect both sympathetic and parasympathetic modulation of the heart, while the HF power reflects primarily vagal control and the mechanical effects of breathing on heart rate throughout the respiratory cycle.3 The ratio between LF and HF power (LF/HF) is also often used to assess the sympatho-parasympathetic balance. Ultimately, the total power is considered to be a global index of HRV.3
Following visual examination of the ECGs, only stable and artifact free recordings with normal sinus rhythm were included in the analysis. The HRV calculation was deemed unacceptable in three patients due to extreme noise or large number of ectopic beats. One participant was excluded as they were unable to complete the two testing sessions. A total of thirteen patients (8 males and 5 females) were included in the final analysis.
Statistical analysisContinuous variables were described using mean and standard deviation. Since computation of reliability coefficients depends on the assumption of normal distribution, the data was examined for normality using Kolmogorov–Smirnov test and HRV indices with skewed distribution were log-transformed using the natural logarithm (ln). A paired t-test or Wilcoxon signed-rank test was used to determine differences between the testing days. Absolute and relative reliability of HRV measurement was evaluated by changes in the mean [mean difference, 95% confidence interval (CI) mean difference, and standard deviation (SD) of the difference between the testing days], measurement variability [standard error of measurement (SEM) and coefficient of variation (CV)], and retest correlations [Pearson's (r) and intraclass correlation coefficients (ICCs), respectively].8 ICCs (2,1) were estimated using two-way analysis of variance and their values were interpreted as moderate (0.41–0.60), substantial (0.61–0.80), and excellent or almost perfect (0.81–1.00).9 A p value <0.05 was considered statistically significant.
ResultsThe study population had a mean age (±SD) of 63±6 years and moderate–severe disease severity (FEV1 46±16% predicted; FEV1/FVC 49±13). More than half the participants were in GOLD stage III (61%), and the other half were in stage II (31%) and IV (8%). Two participants were current smokers and the rest were ex-smokers. All participants were on inhaled lung medication, but none of them were on oral corticosteroids or cardiac medication influencing heart rate.
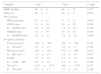
Tables 1 and 2 present the time and frequency domain HRV indices for the two testing days, and their absolute and relative reliability coefficients, respectively. None of the studied variables were statistically different between the testing days. Mean heart rate showed the smallest measurement variability with a CV% of 4.3%. The highest CV% value of 193.4% was found in the log-transformed LF/HF ratio. The other HRV parameters displayed moderate measurement variabilities with time and frequency domain CVs ranging from 11% to 32% after log-transformation. No systematic changes in any of the time or frequency HRV measurement occurred, since 95% CI for the mean difference included zero. The ICC value for mean heart rate showed excellent reliability with a value greater than 0.9, indicating that the random error accounted for approximately 10% of this measurement variability. The variables reflecting overall HRV (lnSDNN, lnLF, and lnTP) showed substantial reliability with ICC values over 0.7. In contrast, the HRV parameters reflecting primarily vagal or parasympathetic activity (lnRMSSD and lnHF) showed only moderate reliability with ICC values around 0.5.
Hemodynamic variables and heart rate variability indices on testing sessions.
| Variables | Visit 1 | Visit 2 | p value |
|---|---|---|---|
| MBP (mmHg) | 96±11 | 98±11 | 0.157 |
| SpO2 (%) | 94±2 | 94±2 | 0.632 |
| Time domain | |||
| HR (beats/min) | 77±11 | 77±12 | 0.685 |
| SDNN (ms) | 31±24 | 30±22 | 0.766 |
| lnSDNN (ms) | 3.2±0.8 | 3.2±0.7 | 0.756 |
| RMSSD (ms) | 32±39 | 33±36 | 0.874 |
| lnRMSSD (ms) | 2.9±1.1 | 2.9±1.2 | 0.940 |
| Frequency domain | |||
| LF power (ms2) | 386±703 | 285±519 | 0.327 |
| lnLF (ms2) | 4.5±1.9 | 4.3±1.7 | 0.756 |
| HF power (ms2) | 283±612 | 275±464 | 0.951 |
| lnHF (ms2) | 3.9±2.0 | 4.2±2.0 | 0.635 |
| LF/HF | 3.7±3.8 | 2.7±3.8 | 0.208 |
| lnLF/lnHF | 0.6±1.6 | 0.2±1.5 | 0.199 |
| TP (ms2) | 1137±1775 | 805±1178 | 0.357 |
| lnTP (ms2) | 5.8±1.7 | 5.7±1.6 | 0.746 |
MBP, mean blood pressure; SpO2, blood oxygen saturation; HR, heart rate; SDNN, standard deviation of all normal-to-normal RR intervals; RMSSD, root mean square of successive differences in normal-to-normal RR intervals; HF, high frequency; LF, low frequency; TP, total power; ms, milliseconds; ln, natural logarithm.
Indices of measurement variability and reliability of heart rate variability between the testing sessions.
| Variables | Mean diff. | SD diff. | 95% CI Mean diff. | SEM | CV% | r | ICC (95% CI) |
|---|---|---|---|---|---|---|---|
| HR (beats/min) | −0.5 | 4.7 | −3.1, 2.1 | 3.3 | 4.3 | 0.93# | 0.93 (0.80, 0.98) |
| lnSDNN (ms) | 0.01 | 0.5 | −0.3, 0.3 | 0.4 | 10.9 | 0.78# | 0.79 (0.48, 0.93) |
| lnRMSSD (ms) | −0.02 | 1.1 | −0.6, 0.6 | 0.8 | 26.6 | 0.55 | 0.57 (0.09, 0.83) |
| lnLF (ms2) | 0.1 | 1.2 | −0.6, 0.8 | 0.9 | 19.9 | 0.78# | 0.79 (0.48, 0.93) |
| lnHF (ms2) | −0.3 | 1.9 | −1.3, 0.8 | 1.3 | 32.4 | 0.57# | 0.59 (0.12, 0.84) |
| lnLF/lnHF | 0.4 | 1.0 | −0.2, 0.9 | 0.7 | 193.4 | 0.82# | 0.77 (0.43, 0.92) |
| lnTP (ms2) | 0.1 | 1.3 | −0.6, 0.8 | 0.9 | 15.8 | 0.71# | 0.72 (0.34, 0.90) |
HR, heart rate; SDNN, standard deviation of all normal-to-normal RR intervals; RMSSD, root mean square of successive differences in normal-to-normal RR intervals; HF, high frequency; LF, low frequency; TP, total power; ms, milliseconds; ln, natural logarithm; diff., difference between the testing days; SEM, standard error of measurement; CV, coefficient of variation; r, correlation coefficient; ICC, intraclass correlation coefficient.
The present study reports the test–retest reliability of standard indices of HRV from short-term ECG recording performed during spontaneous breathing in COPD patients. We found that the time and frequency domain parameters related with the overall HRV showed substantial reliability. In contrast, the HRV parameters associated primarily with parasympathetic tone showed moderate reliability. The only parameter related to the HRV that showed excellent absolute and relative reliability was mean heart rate.
In the current COPD population, the measurement variability analysis revealed mainly a moderate absolute HRV reliability in both time and frequency domains. These findings were similar to previous studies on HRV measurement variability performed under spontaneous breathing in healthy and clinical populations.10,11 The relative reliability showed a similar trend in our study. The ICCs in both time and frequency domain indicated substantial reliability for the overall HRV, but moderate reliability for the HRV parameters reflecting the parasympathetic tone. However, the confidence intervals for these last parameters were very wide (e.g., lnHF exhibited a 95% CI of 0.12, 0.84) precluding any practical use. These results were in line with those performed under spontaneous breathing in healthy and disease populations,10–12 which showed substantial relative reliability of the LF component of HRV as indicated by ICC values exceeding 0.7. However, while the reliability of the HF component of HRV in healthy (ICC, lnHF=0.79)10 and cardiac subjects (ICC, HF=0.77)11 remained substantial, in a disease population manifesting impairments of the respiratory system, such as individuals with spinal cord injury, the reliability of the HF component of HRV was moderate (ICC, HF=0.53),12 and similar to our results. These findings highlight the remaining controversies in regard to the reproducibility of the HF measurement, particularly when they are performed under spontaneous breathing.11,13
To the best of our knowledge, only one study examined the HRV reliability in patients with COPD. Bartels et al.7 found that the time–frequency analysis of HRV was reliable under controlled respiratory rate and oxygen hemoglobin saturation in this population. Their reported correlation coefficient of the LF domain parameter (lnLF, r=0.89) was similar to ours which was performed under spontaneous breathing. However, their better correlation coefficient of the HF domain parameters (lnHF, r=0.89) could be explained by their use of paced breathing. Since that study did not report typical error or ICCs, we cannot make any further comparisons.
In our study, we also found that the mean heart rate displayed excellent measurement variability (CV% of 4.3%) and almost perfect reliability (ICC of 0.93, with a 95% CI of 0.80, 0.98). These figures indicate that for an average resting heart rate of 77beats/min, as found in our population, a change of at least 3beats/min after an intervention can indicate a clinically important change (CV%∗mean resting HR). Given the recognized inverse relationship between heart rate and HRV, these findings indicate that the mean heart rate can be used as a reliable clinical assessment tool for obtaining information about the effectiveness of rehabilitation intervention on cardiac autonomic control in COPD population.
In conclusion, our findings support the use of HRV parameters for cardiac risk assessment, but only mean heart rate can be used reliably for therapy monitoring. The information provided by our study on the HRV reliability should be of value to researchers planning future studies to evaluate the effectiveness of rehabilitation programs in improving autonomic function in COPD population.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
We would like to thank the study participants for their time and interest in our study. We would like to acknowledge the contribution of Ashley Kirkham and Michelle Heneghan in the recruitment of the study participants, and Dr. Kathy Li from the Centre for Health Evaluation and Outcomes Science (CHEOS) for statistical consultation.