Post-intubation tracheal stenosis (PITS) continues to be challenging in terms of diagnosis, management and prevention. Recurrence is common because of excessive granulation tissue formation and an insidious process of scar contracture. Topical application of mitomycin-C (MMC) as an adjuvant treatment for endoscopic management of stenosis has shown good results. The authors aimed to evaluate the results of MMC topical application following bronchoscopic dilatation as an adjuvant in PITS treatment.
MethodsRetrospectively selected patients with PITS who had had rigid bronchoscopy (RB) dilatation followed by MMC application as adjuvant to endoscopic treatment. MMC in a concentration of 0.4mg/ml was applied with a cotton stiletto around the stenotic lesion and granulation tissue for 3min.
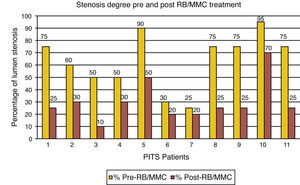
ResultsEleven patients with PITS, with a median initial tracheal stenosis of 75% of the lumen, underwent RB/MMC treatment. Mean MMC sessions performed/patient was 3.5, with good response and prolonged decrease in granulation tissue formation in 55% of cases, moderate in 18% and relapse in 27%. Mean stenosis improvement was 34%.
ConclusionsTopical MMC application at 0.4mg/ml concentration seems to be associated with good results as adjuvant in PITS management with decrease in granulation tissue and sustained improvement in lumen diameter.
O diagnóstico, tratamento e prevenção da estenose traqueal pós-entubação (ETPE) continua a ser um desafio. A recorrência é comum devido à formação excessiva de tecido de granulação e a um processo insidioso de cicatrização constritiva. A aplicação tópica de mitomicina-C (MMC) tem mostrado bons resultados como tratamento adjuvante na manipulação endoscópica das estenoses traqueais. Os autores tiveram como objetivo avaliar os resultados da aplicação tópica de MMC, após dilatação broncoscópica, como tratamento adjuvante da ETPE.
MétodosDoentes com ETPE selecionados retrospetivamente, nos quais foi efetuada dilatação com broncoscópio rígido (BR) seguida da aplicação tópica de MMC como adjuvante no tratamento endoscópico. A MMC na concentração de 0,4mg/ml foi aplicada com um estilete recoberto com algodão, em redor da lesão estenótica e tecido de granulação, durante 3 minutos.
ResultadosEm 11 doentes com ETPE, com mediana de estenose inicial de 75% do diâmetro do lúmen traqueal, foi aplicado o tratamento sucessivo com BR/MMC. A média de sessões com aplicação de MMC efetuada por doente foi de 3,5. Observou-se uma boa resposta e redução duradoura na formação de tecido de granulação em 55% dos casos, moderada em 18% e recorrente em 27%. A melhoria média no diâmetro da estenose foi de 34%.
ConclusõesA aplicação tópica de MMC na concentração de 0,4mg/ml parece estar associada a bons resultados quando utilizada como adjuvante no tratamento das ETPE. Esses resultados devem-se à diminuição na formação de tecido de granulação e melhoria sustentada no diâmetro do lúmen traqueal.
Post-intubation tracheal stenosis (PITS) is the most common benign cause of upper airway stenosis occurring in 1–4% of ventilated patients.1 Management usually involves choosing between endoscopic and open reconstructive procedures.1 Surgical resection and anastomosis is considered the definitive treatment. Bronchoscopic intervention is an important therapeutic alternative with some advantages.1–4 However, in both procedures, recurrence is common (40–70%) over a period of months to years, because of an excessive granulation tissue formation and an insidious process of scar contracture.1,5,6 Mitomycin-C (MMC) is an antineoplastic antibiotic agent that inhibits fibroblast proliferation, modulating wound healing and scarring.1,2,5 Its topical application as adjuvant treatment in endoscopic management of stenosis has shown good results,2,5–8 suggesting that modulation of the wound healing process can play a major role in improving the success rate and reducing the need for frequent procedures in PITS.5,9 The aim of this study was to evaluate the results of topical MMC application after bronchoscopic dilatation as adjuvant procedure in PITS treatment.
MethodsRetrospective selection of patients with PITS observed over the last 6 years (2006–2012) in the Bronchoscopy Unit of Pulmonology Department of the Gaia Hospital Center – Portugal, who had had Rigid Bronchoscopic (RB) dilatation followed by MMC application as adjuvant to endoscopic treatment. RB dilatation from 8.5 to 14mm was performed in all patients. Balloon dilatation was used before RB dilatation in 2 cases of severe stenosis to prevent excessive trauma. Whenever granulation tissue was associated to a fibrotic stricture, radial cuts with Nd-YAG laser or electrocautery were performed at low doses according to the degree of stenosis, before combined RB dilatation and MMC application (RB/MMC treatment). Argon plasma coagulation (APC) and criotherapy were also used, mostly because of exuberant granulation tissue and the benefits of their haemostatic properties. All the described procedures were applied before starting RB/MMC treatment in each patient and also later in selected cases depending on the recurrence of granulation and stenosis characteristics. In each session RB/MMC treatment was the final procedure. MMC was prepared in the Hospital Pharmacy at a 0.4mg/ml concentration, temporarily stored in a syringe, kept inside a cooler which was maintained at 5°C and covered by silvered protection to keep out the light, following the product recommendations. MMC was handled with great care and applied with an impregnated cotton stiletto around the stenotic lesion and granulation tissue for 3min, thereafter cleaned with a cotton stiletto soaked in NaCl 0.9% solution. Any product excess was returned to the pharmacy for appropriate management. All patients were clinically and endoscopically re-evaluated one month after the first MMC session and then monthly for 6 months or until stabilized. More than one RB/MMC session was performed depending on how the process evolved. Besides the interventional techniques performed and results with RB/MMC adjuvant treatment, patients were evaluated for type, location, extension and stenosis diameter (lumen %). RB was performed with the patient's written informed consent and this treatment was approved by the Ethics Committee of our Hospital.
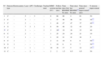
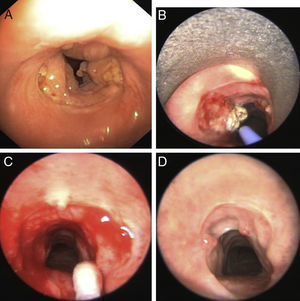
ResultsDuring the period studied, MMC was applied as adjuvant to endoscopic treatment in 11 patients with PITS: 6 women and 5 men, with a mean age of 58.4 (±12.7; min 39, max 72) years old. All patients had different degrees of respiratory stridor at initial physical examination. The initial stenosis diameter varied from 25% to 90% of the tracheal lumen, with a median stenosis diameter of 75%. Stricture was mostly located 1–3cm below vocal chords, with involvement of 1–3 tracheal rings. A fibrous ring conformation (complex stenosis) was observed in 9 cases and 2 presented with half ring (simple stenosis) (Table 1). RB dilatation and topical MMC application was performed as described in all patients. All patients were prescribed systemic steroids (prednisolone dose of 0.5mg/kg/day) for 7 days after procedure to help control inflammation. Depending on the stenosis characteristics – presence of granulation tissue and/or fibrosis – Nd-YAG laser was performed on 7 patients, electrocautery in 4, APC in 3 and criotherapy in 2 selected cases (Table 1). Dumon tracheal stent 16mm/4cm (Novatech.SA; La Ciotat, France) was placed in 2 patients (Table 1); one because of cartilage destruction with tracheomalacia and another because of recurrent granulation tissue related to permanent tracheostomy. The mean number of MMC sessions/patient was 3.5 (min 1; max 10), with prolonged decrease in granulation tissue in 6 (55%) cases, moderate in 2 (18%) and relapse in 3 (27%). As demonstrated in graphic 1 there was a reduction in stenosis diameter in all patients, with a noticeable improvement in granulation tissue formation after RB/MMC treatment (Table 1). In 4 cases we observed 50% reduction in stenosis diameter (Table 1 and Fig. 1), in 2 patients 40% and 3 improved by 25–30%. The median of final airway diameter was 75% of the lumen, with a stenosis total mean improvement of 34%. The mean time from decrease in granulation to clinical improvement was 27.5 months (Fig. 2).
PITS individual treatment description.
| N° | Stenosis type | Electrocautery | Laser | APC | Criotherapy | Tracheal stent | MMC sessions (N°) | Follow-up time (mo) | Time since first RB/MMC Tx (mo) | Time since last RB/MMC** Tx (mo) | Time since general improvement* (mo) | % stenosis improvement |
| 1 | C | – | 5 | – | 3 | – | 8 | 68 | 66 | 4 | 61 | 50 |
| 2 | C | – | 3 | – | – | – | 1 | 57 | 56 | 56 | 53 | 30*** |
| 3 | C | – | 2 | – | – | – | 1 | 48 | 47 | 47 | 37 | 40*** |
| 4 | S | – | 7 | 3 | 1 | 1 | 8 | 50 | 48 | 32 | 43 | 20 |
| 5† | C | – | 3 | – | – | 1 | 3 | 20† | 19 | 16 | 15 | 40 |
| 6 | C | – | 2 | – | – | – | 1 | 25 | 24 | 24 | 21 | 10 |
| 7 | C | 1 | 1 | – | – | – | 1 | 22 | 21 | 21 | 18 | 5 |
| 8 | C | 1 | – | – | – | – | 2 | 11 | 10 | 6 | 8 | 50*** |
| 9 | S | 1 | – | – | – | – | 1 | 10 | 8 | 8 | 7 | 50*** |
| 10 | C | 1 | – | 1 | – | – | 10 | 18 | 17 | 5 | 12 | 25*** |
| 11 | C | – | – | 2 | – | – | 2 | 2 | 1.5 | 0.5 | 0.5 | 50 |
N°, patient number; C, complex; S, simple; APC, argon plasma coagulation; MMC, mitomycin-C; RB, rigid bronchoscopy; mo, months; Tx, treatment; %, percentage.
Clinical improvement and reduction in granulation tissue formation were noticed in most patients 1–6 months after the first MMC application. Response and need for additional procedures depended on stenosis type and characteristics. Some recurrence of granulation tissue was observed in almost all patients at certain times, but they generally become more responsive to simple dilatation and with a long lasting response after MMC application.
No therapeutic option gives 100% result in PITS and all procedures can cause additional injury particularly restenosis by granulation tissue formation and fibrosis.1,4,7,9 Relapse is relatively frequent and is the main long-term problem.1,4,7 In recent years the search for alternative procedures focussed on the modulation of scar formation has increased.3,7 MMC is an anti-proliferative agent which decreases fibroblast proliferation and recurrence of granulation tissue.1,4,5 Repeated MMC applications have shown better results than a single application.1,2,10 The utility of the described doses for tracheal stenosis vary between concentrations of 0.4mg/ml and 2mg/ml,3,7,10 applied for 1–5min.4,9,10 Most studies have demonstrated efficacy and safety of topical MMC at 0.4mg/ml concentration in PITS treatment1,3,4,7,10 and the evidence suggests that the effects of topical application remain localized, with a minimal impact on the surrounding tissue.9 Doses of 1mg/ml have also been associated with improvement in recent analysis1,3 and a less traumatic airway injury from BR dilatation or laser before MMC application seems to be beneficial.1,4,9
Some studies suggest that early stenosis responds better to MMC than mature fibrotic stenosis.3,10 When fibrosis is present a combination of procedures is usually needed for treatment.1 Our case series suggests that RB dilatation followed by MMC application (0.4mg/ml) for 3min can be beneficial in the wound healing modulation, delaying and decreasing granulation tissue formation. As verified in other studies,1,5,6,9,10 we observed a clinical improvement, with a better and longer lasting response in patients treated with MMC.
RB dilatation followed by MMC application was then performed for all patients .We used a combined treatment approach with additional interventional techniques according to the presence of fibrosis, hemorrhagic risk and for management of exuberant granulation tissue. In our experience, from the first MMC application, there was a general improvement within the first 6 months.
Definitive conclusions cannot be drawn from this study because of the small size of our population and the absence of patient randomization or a control group. However, topical MMC (0.4mg/ml) application after RB dilatation as adjuvant in bronchoscopic management of PITS seems to produce good results: a decrease in granulation tissue formation and sustained improvement in lumen diameter. Further research and randomized prospective clinical trials are needed to determine the most effective concentration, time and frequency of exposure to MMC. Exploring the possibility of using MMC earlier in PITS treatment algorithm could lead to improvements for granulation tissue management in the future.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Viveiros F, Gomes J, Oliveira A, Neves S, Almeida J, Moura e Sá J. Aplicação tópica de mitomicina-C como adjuvante no tratamento broncoscópico da estenose traqueal pós-entubação. Rev Port Pneumol. 2013;19:276–280.