Subjects with chronic obstructive pulmonary disease (COPD) may be characterized by muscle dysfunction and symptoms such as dyspnea and fatigue, which may lead to reduced physical activity (PA) levels.1
In COPD, functional exercise capacity as measured by the 6-minute walking test (6MWT) is known to be significantly associated with different PA variables such as walking time/day,2 number of steps/day and time spent/day in different PA intensities, mainly moderate-to-vigorous (MVPA).3 However, a large systematic analysis concluded that the quality of the evidence for these associations is still relatively low.4 Furthermore, Mesquita et al.5 corroborated these findings by showing that changes in the 6MWT are very weakly related to changes in time spent/day in different PA intensities (sedentary: r = −0.26, light: r = 0.25 and moderate-to-vigorous [MVPA]: r = 0.24).
Total volume is a composite variable that corresponds to the product of duration versus intensity of a given effort. It is often used in the context of exercise training, including in patients with COPD.6 However, it is rarely considered in the context of the total volume of PA in daily life (PADL), especially in the literature of patients with COPD. One can reach the same total PA volume in a certain period through many combinations of time spent in different intensities of PADL, i.e., sedentary, light and MVPA. Moreover, the association of the 6MWT with total PA volume/week has not yet been investigated. Therefore, the aim of this study was to investigate the independent association of functional exercise capacity (assessed by the 6MWT) with total PA volume/week in patients with COPD, as well as to compare this association with those concerning 6MWT and time spent/day in different PA intensities.
A retrospective study was conducted comprising baseline data from subjects with COPD assessed for admission in a pulmonary rehabilitation program performed at the University Hospital of Londrina, Brazil. The present sample concerns the combination of patients from a previously published study7 and an ongoing study (ClinicalTrials.gov number, NCT03127878). Both studies were approved by the institutional Research Ethics Committee and all participants signed an informed consent term prior to inclusion. Data collection occurred from 2010 to 2019, and the initial assessments, inclusion and exclusion criteria from the two abovementioned studies were similar. Inclusion criteria were: diagnosis of COPD according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD)1; absence of any regular physical training in the preceding year; clinical stability defined as absence of exacerbations within the last month; and absence of severe comorbidities that could interfere with the assessment protocol (e.g., orthopedic, rheumatological, neurological or cardiovascular). Concerning the analysis of the present study, individuals were excluded in cases of unavailable data from the 6MWT or incomplete data from the PADL assessment, i.e., not achieving the pre-established minimum wearing time for a valid day (see below).
Objective assessment of PADL was performed using a validated PA monitor (SenseWear® Armband, BodyMedia, USA).8 Subjects were instructed to wear the monitor during daytime for 7 consecutive days. A valid day was considered as containing at least 8 h/day of wearing time, excluding sleep periods during the day.9 Total energy spent during the week was defined as the “total PA volume/week”. Time spent/day in PA performed at specific intensities (i.e., sedentary [<1.5 metabolic equivalents of task, METs], light [1.5–3 METs], and MVPA [>3 METs]) was also quantified, both in absolute values and adjusted as a percentage of the respective wearing time. Functional exercise capacity was assessed by the best of two 6MWT, performed according to international standards.10
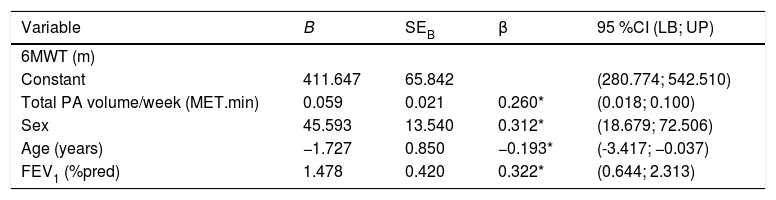
Normality in data distribution was evaluated using the Shapiro–Wilk test and results were described as mean ± standard deviation or median [interquartile range 25–75%], accordingly. Correlations were evaluated by the Spearman’s coefficient. Multiple regression model was performed to investigate the associations between 6MWT and total PA volume/week, with adjustments for sex, age and FEV1 %predicted.
The statistical softwares used were SPSS 22.0 (IBM, USA) and GraphPad Prism 6.0 (GraphPad Software Inc., USA). Significance level was defined as P < 0.05.
Data from 125 subjects with COPD were screened but 33 of them were excluded due to incomplete assessments. Therefore, 92 subjects were analyzed (46 male; 66 ± 8 years; FEV1 50 ± 16%predicted; 6MWT 472 ± 73 m; wearing time of the PA monitor 14.4 ± 1.5 h/day; mean ± SD). Median [interquartile range] of total PA volume/week was 1281[1089–1585] MET.min, whereas time spent/day in sedentarism, light activities and MVPA were 569[465–641], 254[147–338] and 32[12–72] min/day, respectively.
There was positive correlation between total PA volume/week and 6MWT (r = 0.30; P = 0.004). In the multiple regression analysis, total PA volume/week explained 26% of the variation in the 6MWT (independently of sex, age and FEV1%pred) (Table 1). Time spent/day in each specific intensity (sedentary, light and MVPA) both in absolute values and in percentage of the wearing time, was more weakly correlated with the 6MWT (0.06 < r < 0.27), corroborating the previous literature.4 Furthermore, total PA volume/week was strongly correlated with time spent/day in sedentarism, light activities and MVPA (r = −0.59, r = 0.84 and r = 0.79, respectively; P < 0.0001 for all).
Summary of the multiple regression analysis.
| Variable | B | SEB | β | 95 %CI (LB; UP) |
|---|---|---|---|---|
| 6MWT (m) | ||||
| Constant | 411.647 | 65.842 | (280.774; 542.510) | |
| Total PA volume/week (MET.min) | 0.059 | 0.021 | 0.260* | (0.018; 0.100) |
| Sex | 45.593 | 13.540 | 0.312* | (18.679; 72.506) |
| Age (years) | −1.727 | 0.850 | −0.193* | (-3.417; −0.037) |
| FEV1 (%pred) | 1.478 | 0.420 | 0.322* | (0.644; 2.313) |
P < 0.05; B = unstandardized regression coefficient; SEB = standard error of the coefficient; β = standardized coefficient; 95% CI = 95% Confidence Interval; LB = Lower Bound; UB = Upper Bound; 6MWT = 6-minute walking test; PA = physical activity; FEV1 = forced expiratory volume in the first second.
This was the first study to show a significant and independent association between functional exercise capacity (i.e., 6MWT) and PADL assessed from a different perspective in COPD: total PA volume/week. This association is welcome in the sense that improvements in exercise capacity may be necessary to make patients more active and less sedentary.5 Moreover, it was highly correlated with traditional PADL outcomes (time spent/day at different PA intensities). The “PA volume/week” perspective reflects PA guidelines’ recommendations and incorporates different intensities of PA into a single and comprehensive outcome. Therefore, this preliminary report suggests that this is a reasonable and promising approach, since increasing total PA volume/week (regardless of whether this increase occurred at any intensity) may be a more realistic way of achieving PADL improvements in severely debilitated patients. Further investigation of its measurement properties (i.e., sensitivity to changes due to interventions such as pulmonary rehabilitation) may advance the understanding of its usefulness. In conclusion, total PA volume/week in daily life is significantly and independently associated with functional exercise capacity in patients with COPD.
Funding informationThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. However, all authors were supported by individual scholarships or grants from Fundação Araucária, CAPES, CNPq or FUNADESP, Brazil.
Conflict of interestThe authors have no conflict of interest to disclose.
We acknowledge the support of Fundação Araucária, Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Fundação Nacional de Desenvolvimento do Ensino Superior Particular (FUNADESP), Brazil. In addition, we are grateful to colleagues from the Laboratory of Research in Respiratory Physiotherapy for their contributions to this study.