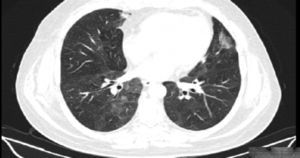
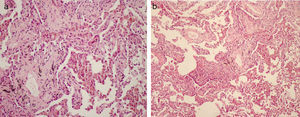
Desquamative interstitial pneumonia (DIP) is a rare interstitial pneumonia usually associated with cigarette smoke.1,2 It is characterized by the accumulation of intra-alveolar macrophages, sometimes associated with giant cells.1,3 The diagnosis may be suggested by patchy ground-glass opacification with a predilection for the mid and lower lung lobes on high-resolution computed tomography (HRCT); subpleural involvement is also typical. Irregular lines, traction bronchiectasis, cysts, emphysema, and nodules are other possible findings of DIP.4 Bronchoalveolar lavage fluid nearly always contains an increased number of alveolar macrophages.2,4 Histologically, DIP is characterized by the accumulation of macrophages in the alveolar spaces associated with interstitial inflammation and/or fibrosis. The macrophages usually contain light brown pigment. Lymphoid nodules and a sparse but distinct eosinophilic infiltrate are common.3 Surgical lung biopsy is still required to make a definitive diagnosis.1–3
Transbronchial lung cryobiopsy (TBLC) is a new endoscopic technique that has recently shown superior diagnostic yield to conventional transbronchial biopsy (TBB).5–7 The advantage of the cryoprobe, compared with conventional TBB or TBB using jumbo forceps is that larger pieces of tissue, without crush artifacts, can be extracted during the freeze-thaw cycle, allowing the identification of complex pathologic patterns. The technique permits visualization of peripheral structures of the secondary pulmonary lobule and facilitates immunohistochemical staining. In addition, TBLC can be performed on an outpatient basis and is both an easier and safer procedure for patients with comorbidities, as it reduces the complications and mortality associated with surgical lung biopsy.6
Most of the data available to date is on TBLC overall diagnostic yield and complication rates.5 However, it is also important for clinicians to know the diagnostic accuracy of TBLC in particular diffuse lung diseases, especially in cases in which histologic evaluation is an essential component of multidisciplinary diagnostic approach, as is the case with DIP.
Our aim was to investigate the diagnostic accuracy of TBLC in patients with clinical and radiological findings compatible with DIP who underwent a multidisciplinary diagnostic evaluation.
Between September 2014 and September 2015, 48 patients underwent TBLC as part of an interstitial lung disease diagnostic approach at the pulmonology department at Centro Hospitalar São João in Porto, Portugal. The patients were anesthetized and intubated with a rigid bronchoscope under jet ventilation. Endoscopic exploration of the bronchial tree was performed through the endotracheal tube using a video bronchoscope, and a Fogarty balloon was introduced into the selected lobe. Subsequently, under fluoroscopic guidance, the transbronchial biopsy was performed using a flexible cryoprobe (2.4mm in diameter and 900mm in length). The cryoprobe was introduced through the flexible bronchoscope work channel, which was connected to a cryosurgical system (Erbokryo CA, Erbe, Germany). The tissue was frozen following the Joule-Thomson principle, using gas decompression (carbon dioxide) at the tip of the probe.
TBLC confirmed the diagnosis of DIP in all five patients (four women) in whom this condition was suspected. Their mean age was 45.2±8.5 years and they were all active smokers. Three of the patients reported dyspnea on exertion, one reported dry cough, and one had no relevant respiratory symptoms. One of the women had systemic sclerosis. Three patients had a moderate restrictive ventilatory pattern (FVC 64.9%±8.2%), and all five patients had mild diffusion capacity impairment (DLCO 57.5%±8.4%). All the patients had a ground-glass pattern with a lower-lung predilection on the thoracic HRCT scan (Fig. 1). Two patients had eosinophilic alveolitis in the bronchoalveolar lavage fluid, while the other three had a higher total cell count with a normal differential.
TBLC was performed in different segments of the same lobe in four patients (right lower lobe in three cases and left lower lobe in one) and in two lobes (right superior and lower lobes) in one patient. Three patients underwent four biopsies, one underwent three biopsies, and one underwent two. The mean size of the samples was 5mm (range, 3–8mm). The histologic features were compatible with DIP (Fig. 2). One patient had a pneumothorax, which required chest tube insertion; none of the patients had significant hemorrhage.
All the patients had a definitive diagnosis of DIP after the final multidisciplinary diagnostic evaluation. The results from this series support previous findings showing that TBLC seems to be a reliable, effective, and safe diagnostic tool for collecting a representative lung sample. TBLC may have a major role in the multidisciplinary work-up of DIP, an entity that has traditionally required surgical lung biopsy for an accurate diagnosis.
Conflicts of interestThe authors have no conflicts of interest to declare.