Pseudoaneurysm is a rare abnormality of the pulmonary arteries. Pulmonary artery pseudoaneurysm (PAP) may develop due to primary lung cancer or metastatic lung disease, a rare phenomenon; the proposed mechanism for its formation involves direct tumour invasion and erosion of the vessel wall.1 Due to hemoptysis and the risk of rupture and enlargement, therapy is essential. Transcatheter embolization is a possible approach,1,2 but little has been reported in this context. In this report, we describe an uncommon case of a PAP secondary to squamous-cell lung cancer and approach with coil embolization.
A 60-year-old male was admitted to the emergency department with a 3-week history of recurrent episodes of moderate hemoptysis. Past medical history was significant for 2-month diagnosis of squamous-cell lung cancer staged as cT4N2M0–IIIB (mass in the right upper lobe involving the upper lobar bronchus and extending into the peribronchovascular regions of the upper and middle lobes) under chemotherapy with Carboplatin and Gemcitabine. Physical examination was normal, except for diminished breath sounds in the right upper lung field. Blood test revealed anaemia (8.4g/dL), leucocytosis (23120/µL) and elevation of serum C-reactive protein levels (14.54mg/dL). Chest radiography showed a cavitary mass with an air-fluid level in the right upper lobe with ipsilateral mediastinal shift.
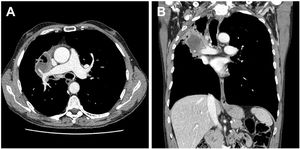
The diagnosis of superimposed infection secondary to the lung tumour was assumed, and the patient was hospitalized. An empiric antibiotic therapy with Piperacillin/Tazobactam and Aminocaproic Acid intravenous infusion was started. No microbiological isolates were found in blood, urine, or sputum. Contrast-enhanced chest computed tomography (CT) was performed, revealing a cavitary mass involving the pulmonary artery branch to the middle lobe, causing stenosis in its proximal segment and distal ectasia (Fig. 1). Fiberoptic bronchoscopy identified a vascular infiltrative lesion in the right upper lobe bronchus with no evidence of active bleeding at that time, therefore no endoscopic intervention was performed.
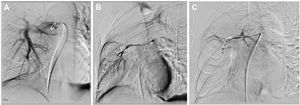
Given the persistence of moderate hemoptysis and anaemia, after a multidisciplinary meeting comprising Pulmonology and Interventional Radiology, transcatheter arterial embolization of the vascular lesion was decided upon. Under conscious sedation, the right pulmonary artery was catheterized via the right femoral vein using the ultrasound control. The angiography detected the presence of a fusiform pseudoaneurysm of the middle lobe branch of the pulmonary artery, with a maximum diameter of 5-mm and an extension of 2-cm between the origin and the arterial bifurcation (Fig. 2). After superselective catheterization, the lesion was embolized with several detachable coils of 0.018-inch size and 3-6mm diameter with the proximal coil placed 2-mm from the origin. The final angiographic study demonstrated complete occlusion of the PAP (Fig. 2). There were no complications. The patient was discharged with occasional blood-streaked sputum, and no anaemia. A follow-up chest CT after 1 month showed coils in the middle lobe branch of the pulmonary artery with occlusion of distal branches. The patient remained with only some episodes of blood-streaked sputum, predominantly in the morning, and a blood test without haemoglobin decrease.
Hemoptysis originates from the pulmonary arteries in less than 10% of patients,3,4 and pseudoaneurysm is the main cause of bleeding.5 Their wall consists of either a single layer of the arterial wall or the surrounding tissue and thus poses a higher risk of rupture.1,2 PAP may be associated with various etiologies such as infection, with tuberculosis being the most common, bronchiectasis, trauma, iatrogenesis, vasculitis, and malignancy.2,5,6 According to some reported cases, PAP due to primary lung cancer is rare and is commonly combined with tumour necrosis.6 The squamous-cell carcinoma is the most frequent carcinoma involved in PAP, due to its biological features that make it prone to necrosis.6 In this case, the PAP was secondary to tumour progression involving a peripheral branch of the right pulmonary artery.
PAPs can be treated by interventional radiologists using minimally invasive endovascular techniques as an alternative to surgical management1. Due to its rarity, mainly isolated case reports about endovascular treatment have been published.4,7 To the best of our knowledge, few cases have been reported in the literature on endovascular management of pulmonary artery lesions caused by lung tumours.4,6 Various techniques for effective embolization have been described using several embolic agents, such as, coils, vascular plugs, stents, and liquid agents.1,4,6,7 In this case, coil embolization was chosen due to the operator's previous experience with bronchial embolization. Detachable coils have the advantage of allowing better control of their liberation, and so complications, such as coil migration and vessel wall damage are diminished.7
The presented case supports the current evidence showing that pulmonary artery endovascular management is an effective, safe, and minimally invasive therapeutic approach for the treatment of hemoptysis in patients with lung tumors4, although few centres perform it.
AuthorshipARG and EMT wrote the manuscript. ES and TS followed the patient. IM was the radiologist who reported the vascular lesion on contrast-enhanced chest CT. TP was the interventional radiologist who performed the procedure and ARG followed the procedure. ARG, EMT, ES, TS, IM, and TP read and approved the final manuscript.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical ConsiderationsWritten informed consent was obtained for use of clinical data and publication.