Inflammatory myofibroblastic tumour of the lung, or pulmonary inflammatory pseudo tumour, includes a spectrum of pulmonary lesions1 of unknown aetiology.2 It is an unusual tumour, or tumour-like mass, and accounts for less than 1% of all tumours of the lung, with no significant racial or geographical differences. It should be considered as a possible diagnosis in a patient usually younger than 40 years, male or female, presenting a pulmonary peripheral mass or nodule in the chest X-ray or CT scan. Although controversial, it is usually defined as a nonneoplastic process characterized by a proliferation of spindle cells, associated with a variably dense polymorphic infiltrate of mononuclear inflammatory cells. Because they mimic malignant tumours, both clinically and radiologically, they are also called quasineoplastic lesions.3 In the majority of cases growth of the lesions is slow, and the diagnosis is difficult before surgery.4 Although the aetiology is not well defined, a background history of respiratory infections is sometimes present, and because of that some authors suggest a reactive inflammatory origin. The behaviour of this lesion is variable and usually benign,5 but occasionally it may have a malignant course, with recurrence or metastasis in a minority of cases. The diagnosis is usually established after complete surgical resection, the treatment of choice, and curative in most cases. Recurrence is seen occasionally, if the resection is not complete, or the lesions are multiple. The great majority of inflammatory myofibroblastic tumours are pulmonary, but lesions have also been reported in other organs,6 such as digestive tract, larynx, heart or central nervous system.
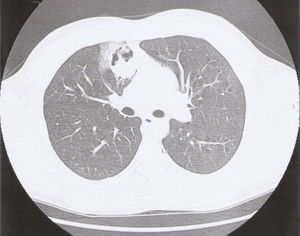
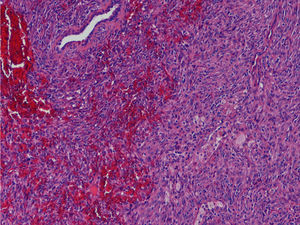
A 24-year-old man, a non-smoker, presented at the emergency department with complaints of cough, haemoptysis, dyspnoea on exertion, fever (38°C) and excessive sweating at night, with two days of evolution. He had no relevant pathologic background, and physical examination was normal. On the chest X-ray we found a right infrahilar shadow, the bronchoscopy was normal as were the respiratory function and the blood tests. The first computed tomography (CT) of the chest showed a 44mm heterogeneous (well-circumscribed and probably cavitated) ovoid mass (Fig. 1), located in the inner right upper lobe, near the middle lobe. The differential diagnosis was lung abscess, round pneumonia, pulmonary tuberculosis, aspergilloma and tumour. After a 3-week course of antibiotics, a second CT, now with intravenous iodinated contrast, showed a homogenous mass of the same size and location, and the patient was transferred for surgical evaluation, and resection of the right upper and middle lobe. Histopathological examination revealed spindle cell proliferation, with storiform or fascicular pattern, with foci of haemorrhage, inflammatory infiltrate of lymphocytes, neutrophils, eosinophils and aggregates of foam cell (Fig. 2). Rare Touton giant cells were also found. No significant cytological atypia was identified. The neoplastic cells were diffusely and strongly positive for immunostaining for ALK and histiocytic marker CD163, while weakly and focally positive for smooth muscle marker SMA and cytokeratin CAM5.2.
The inflammatory myofibroblastic tumour is an uncommon tumour of the lung and an uncommon cause of haemoptysis, but must be considered in a young person7 with a mass or a nodular lesion, although its clinical and radiological presentation is nonspecific. Half of the patients are asymptomatic, the lesion being a radiological finding, but the usual patient complaints are cough, dyspnoea, haemoptysis, chest pain, fever and weigh loss. In this case, despite the rarity of this entity, the form of presentation is consistent with that commonly described in the literature, but the chest pain, although a relatively common symptom, was not present. In our case, as is usual, the diagnosis was chirurgical,8 and the treatment was complete surgical resection.
Conflicts of interestThe authors have no conflicts of interest to declare.