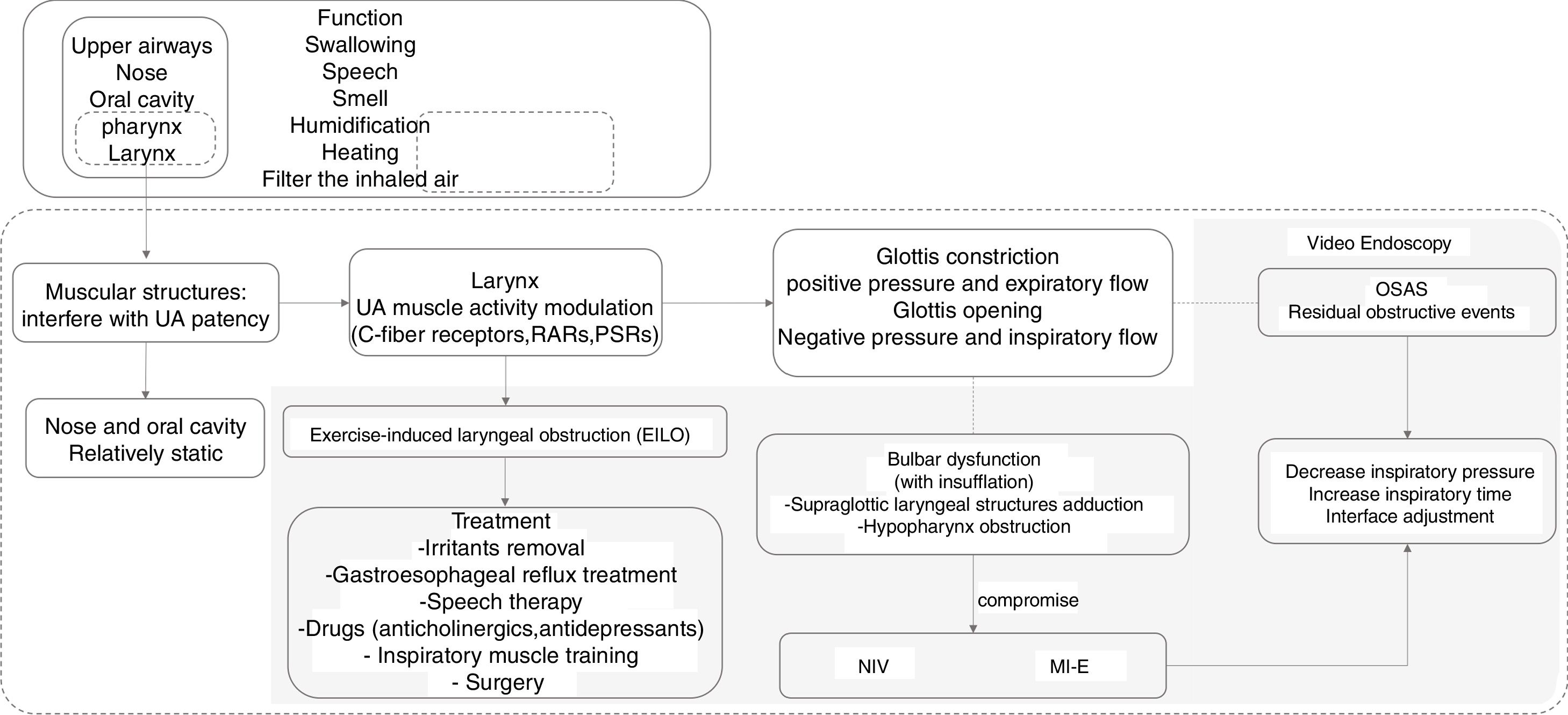
Upper airways (UA) include the nasal cavities, pharynx, and larynx, and its main function is to warm and filter the inspired air. UA dysfunction is in the pathogenesis of various disorders, such as obstructive sleep apnea syndrome (OSAS) and vocal cord dysfunction. In addition, in some neurodegenerative diseases (e.g. Amyotrophic Lateral Sclerosis – ALS), UA dysfunction may also compromise the effective use of ventilatory support (VS). In this context, the endoscopic evaluation of UA may be useful in understanding the OSAS mechanisms, in determining the causes for treatment-induced airway obstruction and even in helping to titrate noninvasive ventilation (NIV) in ALS patients with bulbar or pseudo-bulbar (spastic) dysfunction. Specifically, in OSAS patients, when residual obstructive events persist, although an optimal ventilatory mode has been apparently achieved, along with interface and equipment, the endoscopic evaluation of UA seems to be a valuable tool in understanding its mechanisms, even assisting adjustments to NIV parameters. In addition, it has also been described as being useful in laryngeal response to mechanical in-exsufflation (MI-E) and Exercise-Induced Laryngeal Obstruction (EILO). However, no protocol has yet been published or validated for this.
For this reason, a literature review was conducted on UA function and its response to positive pressure and MI-E. Special emphasis has also been given to the current indication for video endoscopy in chronically ventilated patients.
Noninvasive ventilation (NIV) is the application of ventilatory support (VS) using the natural airway. However, the efficacy of NIV delivered can be greatly compromised by alterations in the upper airway (UA) patency or spasticity. To achieve optimal management of ventilated patients, it is of utmost importance to understand the normal anatomy and physiology of UA, as well as the changes induced by exercise, positive pressure, sedation, body position or obesity.1–5 In addition, soft tissue collapse of UA can significantly decrease its diameter and increase airflow resistance, particularly in the supine position. These phenomena underlie pathological conditions, such as OSAS and obesity hypoventilation syndrome (OHS).1,2 Therefore, the endoscopic evaluation of UA under pharmacological sedation may contribute to the deep study of these patients. In fact, it helps to identify the collapse location, the role of the body position, and select the most appropriate interface.6–9
Recently, classification systems have been developed to standardize descriptions of endoscopic findings.3,10 For example, in patients with persistent obstructive events, even after optimizing ventilatory modes, pressures, and interfaces, the endoscopic evaluation of UA may help to understand and correct the mechanisms underlying residual events, which are recognized as having a negative prognostic impact.4,11,12 In addition, although UA evaluation is clinically relevant to chronically ventilated patients with obstructive or restrictive respiratory diseases, leading to hypoventilation or respiratory failure, the published evidence on these topics is still scarce.11
An important study by Andersen et al.,13 with the objective of evaluating the impact of high pressures provided by Mechanical In-Exsufflator (MI-E) in laryngeal movement patterns of ALS patients with different levels of bulbar involvement, found that some ALS patients with pseudo-bulbar dysfunction were unable to tolerate high pressures during the use of MI-E, even after slight adjustments to inspiratory time and triggers. In fact, the endoscopic evaluation of UA is not routinely indicated to monitor and follow-up patients under NIV and MI-E.11,13–15 Nonetheless, according to current knowledge, UA evaluation may be considered in patients with bulbar dysfunction or residual obstructive events, which are associated with a worse prognosis.12
For these reasons, a literature review was conducted on UA function and its response to positive pressure and MI-E. Special emphasis was also placed on the actual indication for video endoscopy in chronically ventilated patients.
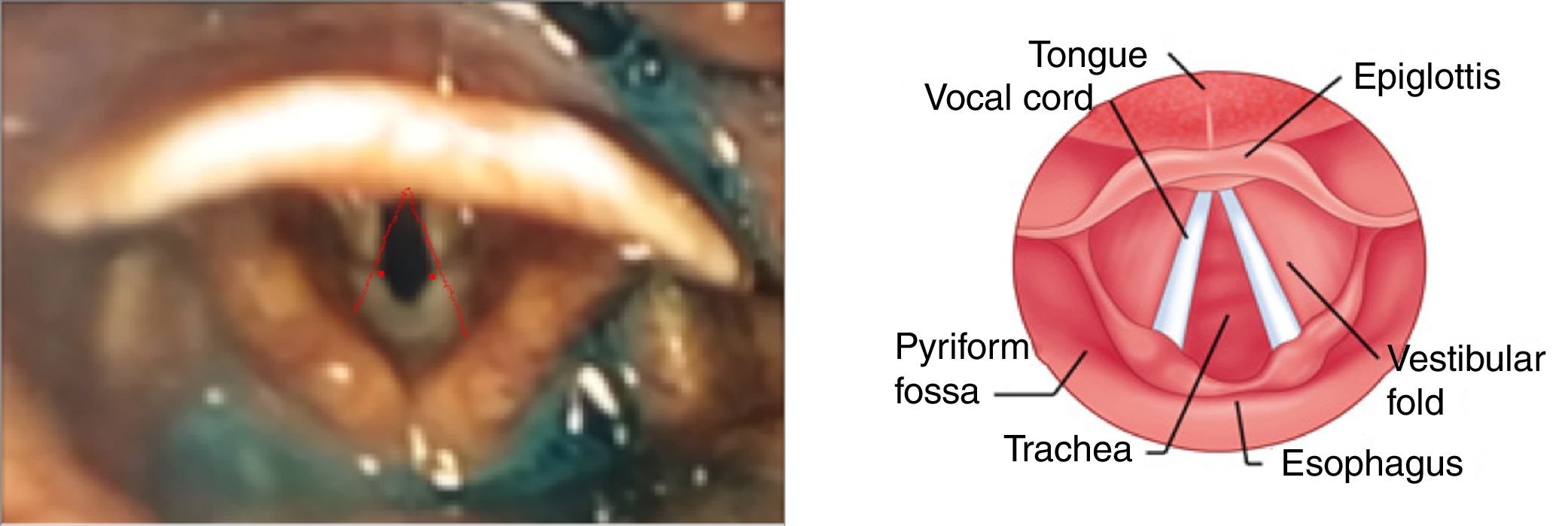
Upper airway structureUpper airways (UA) include the nose, oral cavity, pharynx, and larynx (Fig. 1). These structures allow us to swallow, speak, and smell, as well as filter, warming and moistening the inspired air, until it reaches the tracheobronchial Tree.4 Nose and oral cavity are relatively static in their driving function, while the pharynx and larynx (Fig. 2) are muscle structures that interfere with the patency of UA.4
Laryngeal afferents (i.e. pressure and flow receptors) play an important role in modulating UA muscle activity during ventilation and have a wide impact on glottal adduction rather than oscillatory stimulation.4 In fact, it has been reported that the application of negative pressure and inspiratory flow in UA resulted in an increase in the posterior cricoarytenoid electromyographic activity (glottis opening), whereas positive pressure and expiratory flow increased the thyroarytenoid electromyographic activity (glottis constriction).4
UA afferent are bronchopulmonary C-fiber receptors, rapidly adapting receptors (RARs) and slowly adapting pulmonary stretch receptors (PSRs). C-fiber receptors are excited by mechanical, chemical or thermic stimuli that evoke inhibitory effects (apnea or bradypnea; hypotension and bradycardia) resulting in glottis narrowing, by activating the laryngeal muscles.4
Exercise-induced laryngeal obstructionExercise-induced laryngeal obstruction (EILO) is a condition in which an inappropriate closure of the vocal cord or glottis occurs during exercise.5 Larynx’ dynamic adaptation during exercise, through vocal folds and aryepiglottic folds’ abduction, may occasionally cause laryngeal obstruction at the supraglottic or glottic levels (Fig. 1). Several expressions have been used to describe this phenomenon, including exercise-induced vocal cord dysfunction (EIVCD), exercise-induced laryngomalacia (EIL) and exercise-induced paradoxical vocal fold motion (EIPVFM).5
EILO prevalence in adolescents and young adults in northern Europe is reported at about 5–7%. It is believed that this number increases to 7.1–35.2% among adolescent athletes, with a similar prevalence in pre-pubertal men and women and higher prevalence in post-pubertal women (odds ratio of females/males of 3.41).5,16
Dynamic laryngeal narrowing during expiration is prevalent in patients with COPD and directly relates to disease severity and exercise capacity.17
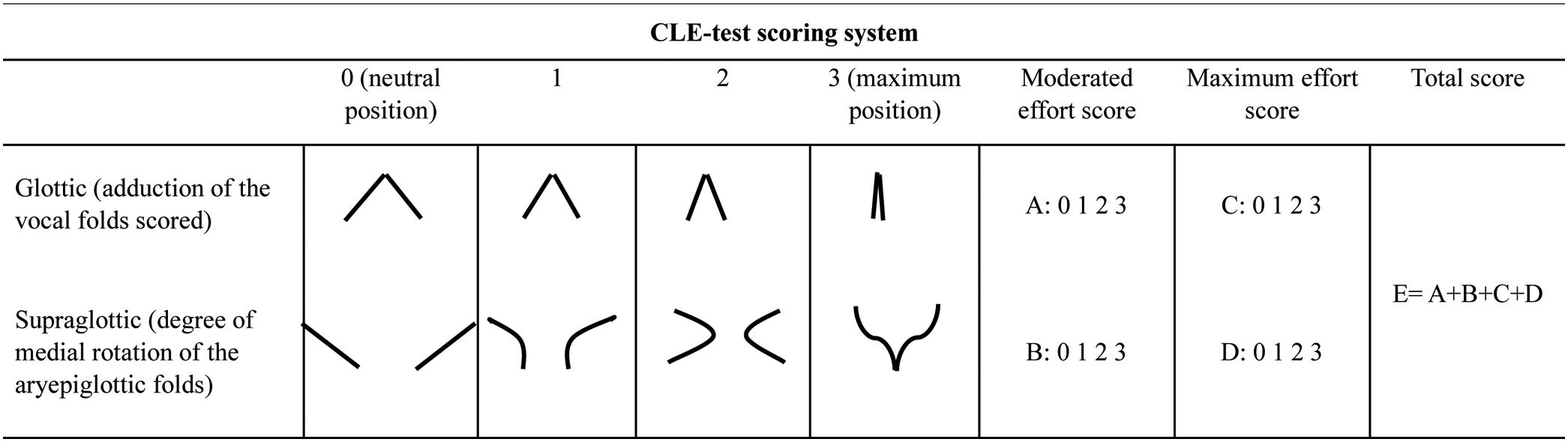
Continuous laryngoscopy during exercise testing (CLE test) is currently the gold standard for EILO.5,16,18 This test includes symptom replication, with an exercise protocol, when the patient is connected to a cardiopulmonary exercise unit and a 12-lead ECG with a facemask. Simultaneously, a flexible nasal laryngoscopy is performed and a microphone records breathing sounds. The test is positive if the patient reproduces their laryngeal symptoms, ideally supported by a threshold in oxygen consumption and/or heart rate response.5,16,18
CLE test provocation is any form of physical exercise that may potentially reproduce the clinical symptoms of EILO. For example, the exercise challenge using the maximum exercise stress (MES) testing is widely used and shows high sensitivity (89% versus 52% without provocation).5 The stationary bike and treadmill are also provocation methods for CLE tests with good diagnostic accuracy.5
The objective analysis of the laryngoscope images obtained from CLE includes the CLE test scoring system, as seen in Table 1, and the EILOMEA (audiovisual) software.17 CLE test score system evaluates the degree of medial rotation of the aryepiglottic folds and the abduction of scored vocal folds with moderate exertion (when running on the treadmill) and maximum effort (shortly before exhaustion.5
Asthma or rhinitis should be excluded as a differential diagnosis, and gastroesophageal reflux (GER) should be treated as it may be a trigger for EIL.16 So, the EILO treatment should include removal of irritants and treatment of GER (Fig. 1). Speech therapy has been highly effective, with 89% of patients presenting symptoms’ resolution or improvement.5 In addition, some drugs (e.g. anticholinergics or antidepressants) and inspiratory muscle training could also be helpful.16 However, when the approaches described are ineffective and occlusion occurs at the supraglottic level, surgical treatment with supraglottoplasty is the preferred therapeutic option.5,13
Upper airways endoscopic findings during sleep/sedation and collapse scalesPharyngeal airway patency depends on the skeletal and soft structures. Obesity, a major risk factor for obstructive sleep apnea (OSA), can lead to narrowing of UA, mainly due to increased adiposity and enlargement of the tongue and soft tissues surrounding.1
OSA is characterized by recurrent collapse of the UA and worsens frequently when sleeping in the supine position.1,2 However, there is great variability among patients in responding to positional changes, and the reason for this variability is still poorly understood. The severity of OSA assessed by AHI may be influenced by factors other than anatomy, such as instability of the respiratory control, variations in the threshold of arousal, and poor responsiveness of the UA dilator muscle during sleep.1 Endoscopic evaluation of UA during sleep, with or without sedation, is important, since the static image of UA during wakefulness does not always capture the reduction in UA diameter, characteristic of OSA.1
Drug-induced sleep endoscopy (DISE) was developed for the evaluation of the UA under pharmacologic sedation using fiber optic endoscopy. To characterize the findings, some classifications scales, such as VOTE, have been created, that describe the degree and configuration of the obstruction at velum, oropharynx lateral walls, tongue base, and epiglottis.10
Studies of drug-induced sleep endoscopy (DISE) in OSA patients have shown that UA obstruction results from the collapse of one or more pharyngeal structures: soft palate, lateral walls of the pharynx, base of the tongue, and epiglottis.2 In fact, using DISE to assess UA obstruction, the prevalence of epiglottis collapse has been reported as 12–30%, and epiglottis collapse seems to respond well to positional therapy, in contrast to tongue-related obstruction, which seems to persist in the non-supine position. Thus, continuous positive airway pressure (CPAP) therapy may be considered an alternative for these patients.2 In relation to the treatment with positive pressure, the use of nasal interface is considered more physiological and efficient for correction of obstructive events, since it allows greater airway patency, as demonstrated by endoscopy.6–8 DISE could be used simultaneously to the polygraphic monitoring of cardiorespiratory parameters, which is safe, feasible and more sensitive in the detection of obstructive breathing events.3
Upper airways response to positive pressure ventilation in healthy subjectsPrevious studies have tested the impact of NIV-derived positive pressure with a nasal interface in the UA of healthy subjects. The protocol included the delivery of 3 different levels of Inspiratory Positive Airways Pressures (IPAP: 10, 15 and 20cmH2O), in the presence of 5cmH2O of Expiratory Positive Airway Pressure (EPAP), using controlled and spontaneous modes.19,20 The authors concluded that incremental IPAP did not always lead to improvements in lung ventilation, so they suggested that the use of a two-level positive-pressure ventilator in controlled mode is less predictable and less stable compared to volumetric ventilators.19 This observation may be explained by the significant narrowing of the glottis caused by adduction of the vocal cords for all patients undergoing positive pressure.19
In spontaneous mode and wakefulness, the efficacy of positive pressure ventilation is better for IPAP of 20cmH2O compared to 10 and 15cmH2O, since the glottis does not appear to play a significant role in the spontaneous mode of ventilation efficacy.20 This aspect is different for sleeping and wakefulness periods. Thus, the effectiveness of pressure ventilation is shorter in sleep time and may allow periodic breathing,19,20 which justifies the recommendation for suitable titration of ventilatory parameters, based on polysomnography and, eventually, capnography data.14,15
A recent study evaluating glottis patency in the acute exacerbation of COPD with NIV found that, high pressures using different ventilatory modes did not cause UA obstruction, but increased respiratory volume, perhaps because the protective and normal reflex response at high pressures did not occur in COPD patients. The main reason invoked was the alteration of the C-fiber receptors response to chemical stimulus with narrowing of the glottis, due to chronic inhalation of carbon dioxide. Therefore, this may be the reason for the high-intensity ventilation effectiveness in COPD patients.21
Upper airway endoscopic evaluation during NIVThere is little published data about the study of UA in patients with NIV support. Although not proven, there are several approaches which might explain the mechanism of residual obstructive events or persistent hypoventilation, even with elevated EPAPs (>12cmH2O), such as collapse of the soft-palate in patients with oronasal mask, the backward movement of epiglottis or tongue-base obstruction, with consequent reduction in retroglossal space. UA video endoscopy may be useful in detecting such problems and in guiding therapeutic decisions, such as the replacement of the nasal mask interface or the indication for uvulopalatopharyngoplasty.11 As previously stated, residual events are associated with worsening prognosis, such as in ALS patients; so, it is important to correct them.12 In ALS patients, upper motor neuron involvement and impairment of bulbar function are associated with UA spasticity and sometimes preclude NIV support. For other pathologies, the UA collapse, as demonstrated by endoscopic evaluation, is not predictable and, therefore, it is essential to improve selection of patients for endoscopic evaluation of UA. This would make it possible to extend the use of NIV, correcting the observed collapse and selecting the best time and patients to do the tracheostomy.
MI-E impact on upper airwaysThe intrinsic larynx muscles interact in complex ways during cough, speech, and swallowing, but they always act in a well-coordinated fashion.13 However, this reflex circuit may be hyper-responsive or dysregulated in ALS patients, leading to an inappropriate closure of the larynx.13 For example, early dysfunction of the vagus nerve may be observed prior to any clinical signs of bulbar dysfunction in ALS patients with spinal onset.13
There are two different subtypes of bulbar ALS currently described: progressive (hypotonic) and pseudobulbar (spastic) ALS, which may influence laryngeal response patterns to MI-E. In pseudobulbar ALS, laryngeal adduction occurs mainly at the glottis level, when relatively high insufflation pressures are applied. Thus, in a predominantly spastic disease, it seems reasonable to suggest that positive pressures trigger laryngeal adductor reflexes more easily. On the other hand, in bulbar hypotonic ALS patients, adduction occurs at the supraglottic level, where increased airflow initiates negative intraluminal pressures that eventually cause medial collapse. In this case, positive pressures may compromise laryngeal inlet during insufflation due to a retroflex movement.13
Andersen et al.13 showed that hypopharynx constriction during exsufflation is present in healthy controls as in ALS patients (even with bulbar symptoms), but was more pronounced in those with progressive bulbar paresis. However, the differences observed in laryngeal movements between patients with pseudobulbar and progressive bulbar ALS were not significant.13
These results indicate that MI-E in bulbar ALS patients was related to adduction of supraglottic laryngeal structures during insufflation, which appeared to compromise airflow, occurring in association with the backward movement of the base of the tongue during insufflation, which increases hypopharynx obstruction. This phenomenon does not occur in ALS patients without bulbar involvement or in healthy controls.13 Therefore, to correct this, researchers have suggested lower positive pressures combined with longer inspiratory times, which could ensure laryngeal stability during insufflation.13 Another study by Andersen et al.,22 evaluating the follow-up of ALS patients and the changes occurred in UA as the disease progresses, verified that, during insufflation, true adduction of vocal folds occurs in 8 of the 9 spinal-onset patients, while adduction of the aryepiglottic folds occurs in all patients, initially at the highest positive pressure, even without bulbar symptoms. With disease progression, laryngeal adduction occurred at lower insufflation pressures, while exsufflation hampered hypopharynx constriction in all patients.22 This suggests that, MI-E should be used with caution in bulbar ALS patients, and closer monitoring and repeated evaluation of efficacy is recommended.
Residual obstructive events, prognostic impact, and correctionEven in bulbar-onset ALS patients, especially in the early stages of the disease, NIV support has a huge impact on survival.23,24 In fact, obstructive events often cause episodes of repetitive desaturation and activation of the sympathetic nervous system.25 Obstructive residual events, defined as abnormalities over 5/h, were associated with an increase in mortality and cardiovascular events in some diseases, such as COPD, neuromuscular or cardiovascular diseases.12,25,26 Thus, correction of obstructive events is crucial, as is the correction of nocturnal desaturation. Multiple monitoring methods have been developed for adequate ventilation titration, and polysomnography with transcutaneous capnography is considered the gold standard in the most difficult cases, according to most of the literature.14,15 Nonetheless, in some situations, such methods may be insufficient and, thus, videoendoscopic evaluation of UA during ventilation titration may be useful. To date, there are no validated or standardized protocols for video endoscopy during ventilation titration. However, some authors have suggested performing endoscopic evaluation during NIV where there are persistent residual obstructive events, despite EPAP >12cmH2O and signs of significant bulbar dysfunction associated with spasticity. This may lead to ineffective MI-E, despite attempts to reduce inspiratory pressure to increase inflation time or define the trigger.11,13
ConclusionThe UA endoscopic approach, while implying some degrees of invasiveness, may add benefits to some patients or diseases, such as resolving obstructive events (e.g. ventilated OSAS and neuromuscular patients, EILO, and bulbar dysfunction compromising cough assistance).
Some authors have suggested the use of specific protocols in the endoscopic evaluation of UA, specifically for patients with uncorrected obstructive events, with high EPAP (>12cmH2O), and with asynchronous or ineffective ventilation, despite adjustments of appropriate parameters under complete monitoring (oxy-capnography and level 1 polysomnography). In addition, suspected UA occlusion with assisted cough also suggests the need for UA inspection.
In summary, although effort is still needed in this area, it is expected that the development of standardized protocols, in specialized centers and including patients with specific diseases, will allow a more complete understanding of the pathophysiology of UA and, consequently, will provide more accurate patient identification, selecting those most likely to benefit from the endoscopic evaluation of UA. This aspect will ultimately trigger a marked improvement in VS efficacy or cough assistance, correcting residual obstructive events and improving patient outcomes. So, we believe that this strategy could extend NIV support to another level.
Conflict of interestsThe authors declare that they have no conflict of interests.
Martins N. would like to thank the Portuguese Foundation for Science and Technology (FCT – Portugal) for the Strategic project ref. UID/BIM/04293/2013 and “NORTE2020—Programa Operacional Regional do Norte” (NORTE-01-0145-FEDER-000012).