Despite the fact that there are a great number of established etiologies for pleural effusion, there are grounds for believing that there are also causes from unusual pathophysiological mechanisms, seen in certain clinical contexts and from potential iatrogenic interventions. Urinothorax is such a rare type of pleural effusion as there are fewer than 70 cases reported worldwide.
Clinical caseA patient with a persistent left pleural effusion was admitted to the Urology ward for a lithiasic obstructive uropathy with hydronephrosis. A left percutaneous nephrostomy was performed. The effusion was unclassified at the initial workup and recurred after first drainage. A second approach confirmed a citrine fluid with borderline criteria for exudate, ammoniacal odor and an elusive pleural fluid-to-serum creatinine ratio. A retroperitoneal urinoma was recognized on CT, and the patient underwent a left nephrectomy with resolution of the pleural effusion.
ConclusionsUrinothorax most frequently develops in patients with excretory uropathy or blunt abdominal trauma, although other mechanisms have been reported. Traditionally, a pleural fluid to serum creatinine ratio higher than one is a hallmark of this condition. In certain settings, taking this diagnosis into account at an early stage might be crucial for a good outcome.
Apesar da multitude de etiologias de derrame pleural, algumas causas decorrentes de mecanismos patofisiológicos incomuns podem ser suspeitadas com base em determinados contextos clínicos sugestivos ou intervenções com potencial iatrogénico. O urinotórax é um tipo raro de derrame pleural com menos de 70 casos mundialmente reportados.
Caso clínicoUm doente que fora internado na Urologia por uropatia obstrutiva litiásica com hidronefrose, é diagnosticado com derrame pleural esquerdo persistente. Havia sido sujeito à colocação ipsilateral de nefrostomia percutânea. Após a primeira toracocentese diagnóstica a causa do derrame não era aparente. Uma segunda abordagem confirmou a presença de líquido citrino com critérios borderline para exsudato, odor amoniacal típico e um ratio evocativo entre creatinina pleural e sérica. A tomografia computorizada (TC) realizada diagnosticou presença de urinoma retroperitoneal, tendo o doente sido submetido a nefrectomia esquerda com resolução do derrame pleural.
ConclusõesO urinotórax encontra-se mais frequentemente em doentes com uropatia excretora ou trauma abdominal contuso, apesar de outros possíveis mecanismos já reportados. Tradicionalmente, um ratio de creatinina pleural/sérica superior a um é um traço distintivo desta condição. Em determinados contextos, a consideração desta possibilidade diagnóstica pode ser determinante para um melhor prognóstico final.
The study of pleural effusion is not often straightforward and a significant percentage of effusions remain unclassified after the initial fluid study. While there are a great variety of likely etiologies to consider initially, there are also some cases that come from rare pathophysiological mechanisms, in these cases we need to look for relevant clues from particular clinical contexts or potential iatrogenic interventions. Urinothorax, urine accumulation in the pleural space, is an unusual cause of pleural effusion that is often overlooked; fewer than 70 cases have been reported worldwide. Although various leading mechanisms have been reported, it most frequently develops in patients with kidney or excretory uropathy or blunt abdominal trauma.
Traditionally, a pleural fluid-to-serum creatinine ratio higher than one is a hallmark of this condition, and there are some other features that can assist in this diagnosis.1,2
Case reportA 77-year-old male patient, with a history of obstructive chronic renal failure, nephrolitiasis and chronic alcoholism but no previous respiratory disease, was treated in the emergency department for recurrent macroscopic haematuria. He had recently had a left ureteral catheter removed following a renal colic with evidence of radiolucent calculi and ipsilateral hydronephrosis. He was admitted to the Urology ward, and a right ureteral catheter was inserted and a percutaneous nephrostomy catheter positioned on the left side.
On the sixth day after admission he was found to have a moderate size left pleural effusion. Under clinical observation he was apyretic, eupneic, with SaO2 97%, blood pressure 108/60mmHg, normal heart sounds, 82bpm, with no murmurs; chest expansion was symmetric, with no breath sounds and vocal fremitus on the left lung base, and accompanying dullness to percussion; there were no peripheral edemas or adenopathies. He presented abdominal discomfort on the left iliac quadrant. The left percutaneous nephrostomy catheter presented serous residual drainage.
The patient did not present cough, chest pain or ortopnea, and was under standard thromboembolic prophylaxis. He was medicated with losartan, calcium, epoetin-alpha, alopurynol and tansulosin as an outpatient. He had not been put on any other medication apart from the antibiotic and there was no recent known respiratory infection. He had an occupational history of agriculture, without recognizable asbestos exposure.
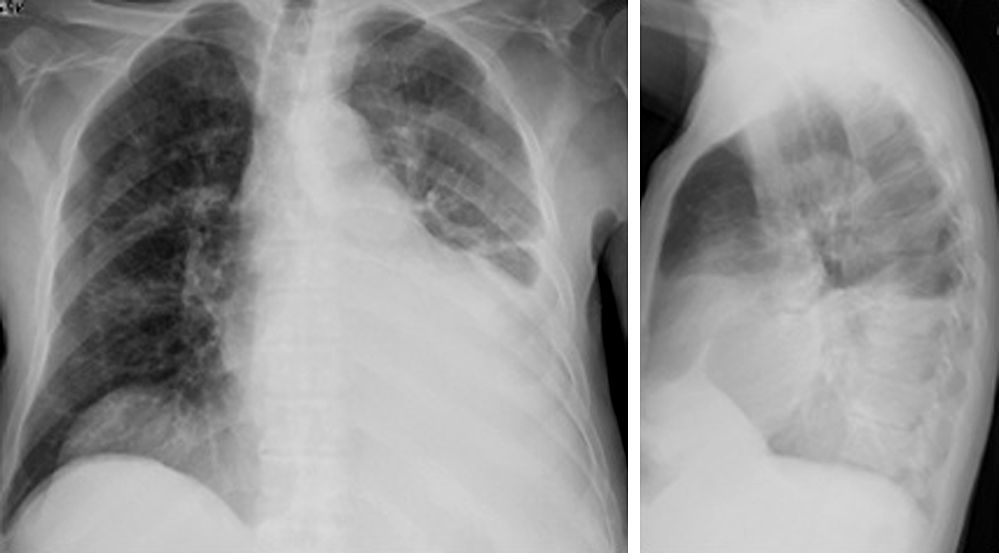
The first chest radiograph (Fig. 1) presented an increased homogeneous opacification on the left lower hemithorax, suggestive of a small to moderate-sized pleural effusion. A contralateral T-tent hemidiaphragm was present. Thoracic ultrasound showed a mobile effusion with no pleural nodules or thickening.
Blood test showed a creatinine of 2.4mg/dL (patient's normal base value of 1.7), hypoalbuminaemia of 2.0g/dL, DHL 322U/L, CRP 11.2mg/dL, procalcitonine 0.2mg/dL, hemoglobin 9.4g/dL, 5.1white cells/L, proteins 5.3g/dL, and normal serum amylase and amylasuria.
Prior to the pleural fluid study there had been several possible etiologies, such as cardiogenic effusion, parapneumonic or tuberculous effusion, malignancy, thromboembolic-related effusion, uremic pleurisy and urinothorax. A first diagnostic thoracocentesis collected 200mL of citrine-yellow transudative fluid for initial workup (pH 7.7, proteins 2.9g/dL, albumin 1.4g/dL, glucose 86mg/dL, LDH 200U/L, microbiologically and cytopathologically negative).
The following week the effusion progressed. A second thoracocentesis drained about 550mL of clear citrine fluid, this time with a noticeable ammonia odor, and a broader workup testing was arranged. Pleural fluid analysis presented a normal pH (although it had to be measured by strip due to the potentiometer malfunction), total proteins of 3.0g/dL, glucose 120mg/dL, albumin 1.4g/dL, DHL 197, creatinine 2.92mg/dL, triglycerides 36mg/dL, amylase 28U/L; ADA 9.0U/L; estimated protein gradient was 0.57, DHL ratio 0.61, and creatinine pleural-to-serum ratio of 1.21. Total cellularity was 300cells/μL, with 16% lymphocytes, 5% neutrophils and 78% mesothelial cells. Cytopathological and microbiological studies were, again, negative.
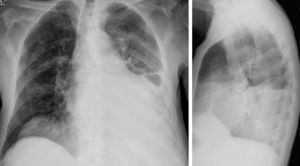
The CT undertaken (Fig. 2) presented: a left moderate free pleural effusion; normal pulmonary angiography and no mediastinal/hilar adenopathies; a left atrophic kidney with the percutaneous nephrostomy catheter and a retroperitoneal and perinephric collection, with some areas of low density while others were high, consistent with the presence of a retroperitoneal urinoma with some interspected areas of hematoma.
The patient underwent a left nephrectomy with progressive resolution of the pleural effusion in the early post-operative period.
DiscussionThe left pleural presence of urine was recognized in our patient. Urinothorax most commonly develops after obstructive uropathy with hydronephrosis or traumatic diaphragmatic disruption by blunt abdominal trauma.3,4 In the first case, it occurs either by thoracic urinary lymphatic ascension (through reabsorption and lymphatic drainage of extravasated urine from retroperitoneal urinomas), or by a mechanism of direct transdiaphragmatic passage from those collections to the pleural cavity. Other etiologies have been described such as: retroperitoneal inflammatory processes; percutaneous endoscopic renal procedures; polycystic renal disease; ureteral valves; extracorporeal lithotripsy; or intra-abdominal compression from gravid uterus or lymphomatous masses.5–9
In our case, there were two simultaneous etiological factors to consider: the well documented obstructive uropathy with retroperitoneal urinary leakage; and the percutaneous nephrostomy placement at the time of admission. Though, in the latter case, no traumatic misplacement was recognized.
This unusual type of pleural effusion is frequently unilateral, of small-to-moderate volume and ipsilateral to the urinary obstructed tract.10 Although classically known as a transudate, on rare occasions it can present as an exudate.2,11
The fluid is normally clear and yellow, with a distinctive ammonia odor, with low protein content and normal to high LDH. There have also been reports of Low pH and glucose levels, but these are unreliable markers and may not always be present.7,11,12
The patognomonic feature is a pleural fluid-to-serum creatinine ratio always above one, although some variability has been reported, depending on the stage of evolution. Microbiological and cytopathological studies must be negative. In less typical situations or where there is low clinical suspicion of urinothorax, patients with recurrent effusions of undetermined etiology might undergo medical thoracoscopy.
On CT imaging, perirenal urinomas, renal or other excretory tract pathology and extravasation of contrast-enhanced urine to the retroperitoneum or pleural space, are the most common features.13 Renal scans can also be valuable indicators of the presence of urinopleural fistula. Today, MAG-3 renal scans are preferred over the Tc-99m labeled diethylenetriamine pentaacetic acid (DTPA). Some authors suggest that, when a therapeutic intervention is possible, invasive studies like retrograde pyelogram and endoscopy of the renal collecting system, might be justified.13,14
Treatment is specifically directed to the correction of the primary cause and drainage of the fluid. In our case, as is normally the case, the relief of the urinary tract obstruction led to the progressive resolution of the effusion. The decision for nephrectomy was already being proposed by the Urology team as a better option than an ultrasound-guided drainage of the urinoma. The following elements were taken into consideration: the patient had had recurrent episodes of high tract lithiasic obstruction, with a strong tendency for sepsis; an only marginally functioning left kidney; and a recent confirmation of retroperitoneal leakage, even with nephrostomy, along with a persistent urinothorax as a new complication.
Simple tube thoracostomy is advised for large effusions and for patients where the symptoms are very clear. In case of asymptomatology or minor symptoms, it is reasonable to perform drainage by needle thoracocentesis because with most patients the urinothorax will clear-up after the primary obstruction is relieved.13
The recurrence of an urinothorax is a strong pointer toward an inadequately drained collecting system, which needs further study and to be treated aggressively. In a few cases, a persistent urinothorax may involve the surgical correction of concealed tears in the urinary system, renopleural fistulas or even nephrectomy, as described above. There have been no reports of persistent urinothorax requiring surgical management involving the diaphragm or thoracic cavity so, as recommended by Wey et al., the threshold for referring a patient for video-assisted thoracoscopic surgery (VATS) should therefore be high.13
This kind of etiology may easily go undiagnosed. In patients with pleural effusion and a current/recent urinary tract disorder it should be seriously considered.15 Ideally these patients are best managed by a multidisciplinary team including an urologist13 and a pulmonologist.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ferreira PG, et al. Urinotórax como causa rara de derrame pleural – Revisitação a propósito de caso clínico. Rev Port Pneumol. 2013. http://dx.doi.org/10.1016/j.rppneu.2012.10.001.