Helmet CPAP (H-CPAP) has been recommended in many guidelines as a noninvasive respiratory support during COVID-19 pandemic in many countries around the world. It has the least amount of particle dispersion and air contamination among all noninvasive devices and may mitigate the ICU bed shortage during a COVID surge as well as a decreased need for intubation/mechanical ventilation. It can be attached to many oxygen delivery sources. The MaxVenturi setup is preferred as it allows for natural humidification, low noise burden, and easy transition to HFNC during breaks and it is the recommended transport set-up. The patients can safely be proned with the helmet. It can also be used to wean the patients from invasive mechanical ventilation. Our article reviews in depth the pathophysiology of COVID-19 ARDS, provides rationale of using H-CPAP, suggests a respiratory failure algorithm, guides through its setup and discusses the issues and concerns around using it.
In 2019, a cluster of a novel acute atypical respiratory disease was described in Wuhan, China. A novel coronavirus was responsible for the outbreak and was named severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) due to its high homology with SARS-CoV, which also caused severe pulmonary involvement with a high mortality in 2002−03. The new disease was named Coronavirus disease 19 (COVID-19) and in 2020 the World Health Organization (WHO) declared a pandemic impacting nearly the entire world.1
SARS-CoV2 primarily affects the respiratory system, but many additional organ systems can also be severely affected. A high percentage of COVID-19 patients admitted to an Intensive Care Unit (ICU) develop severe acute hypoxemic respiratory failure (AHRF) and fulfill criteria for COVID-19 acute respiratory distress syndrome (CARDS), requiring mechanical ventilation.2–4
For patients with COVID-19, use of noninvasive mechanical ventilation with face masks (FM) or high flow nasal therapy (HFNT) has been either reduced or restricted to airborne infection isolation rooms, due to the viral aerosolization potential with these techniques.5,6 Therefore, across the Unites States (US), in hypoxemic patients who can no longer be sustained on conventional oxygen supplementation, the rate of intubation and mechanical ventilation remains high.2,4,7
In China and many European countries, noninvasive respiratory support (NRS) has been employed in up to 32.4% of COVID-19 patients requiring intensive care1,3 and includes helmet-based methods as part of a respiratory failure management strategy.8–11 Helmet Continuous Positive Airway Pressure (H-CPAP) was initially introduced in the 1990s using modifications of existing hyperbaric oxygen treatment devices, and thereafter the use expanded to NRS for additional indications.12,13 H-CPAP has recently been reported to significantly reduce SARS-CoV-2 aerosolization and exposure risk for healthcare personnel compared to HFNT or FM.6,9,10 When facility ICU bed and ventilator capacity has been temporarily expended, H-CPAP could be a lifesaving, easy to perform respiratory management tool for appropriate COVID-19 patients with respiratory failure and subsequently may not necessarily require an ICU stay. H-CPAP may avoid the need for intubation and ventilator associated problems in patients with CARDS altogether.14,15
This practical review summarizes the COVID-19 respiratory physiology, the evidence to date for helmet use as well as step-by-step instructions for clinicians to deliver CPAP with a helmet for patients requiring noninvasive respiratory support during a respiratory pandemic such as COVID-19.
Pathophysiology and respiratory mechanics of COVID-19 dyspneaThe pathophysiology of COVID-19 respiratory distress may best be described as an inflammatory induced pulmonary vasculitis, leading to varying degrees of lung collapse secondary to edema and microthrombosis,16 characterized by bilateral ground glass opacities on CT-scan, resulting in ventilation perfusion ratio (V̇/Q̇) mismatching and a significant shunt fraction.17,18
Elevated clot waveform analysis parameters are consistent with hypercoagulability in critically ill COVID-19 patients.19 CARDS is an “atypical” form of ARDS, leading to severe hypoxemia, dyspnea, impaired lung diffusion, formation of intravascular microthrombi hypoxic vasoconstriction, and intrapulmonary shunting.19,20 As in the first days of the disease, the lung mechanics are well-preserved and there is usually no increased airway resistance or dead space ventilation, a disparity may be seen between the degree of hypoxemia and a clinically otherwise relatively unimpaired, “happy” patient.21
To better distinguish CARDS from classic ARDS, a continuum between 2 phenotypes of CARDS has been proposed to describe the pathophysiology, although not supported by any controlled trial and still in need of more precisely defined mechanisms. The early Type L is characterized by low elastance, (relatively high compliance, 50.2 ± 14.3 mL/cmH2O), low ventilation to perfusion ratio, limited PEEP response and low alveolar recruitability. The late type H is characterized by high elastance, high right-to-left shunt, high lung weight, better PEEP responsiveness, and high alveolar recruitability.20,22 The two types are not mutually exclusive and overlap occurs during the course of the disease.
Improved arterial partial pressure of oxygen (PaO2) by positive end-expiratory pressure (PEEP) may be explained not only by lung recruitment, but also by more even distribution of perfusion, diverting flow toward the high Va/Q areas.23 The optimum level of PEEP to improve oxygenation still remains controversial and may depend upon presenting phenotype.
Rationale for Helmet CPAP in patients with hypoxemic respiratory failureIn a recent meta-analysis of trials of adults with AHRF, treatment with NRS including H-CPAP was associated with lower risk of death compared with standard oxygen therapy.24
In addition to the relative ease of use, H-CPAP may have physiological and biological advantages over the alternative strategies. H-CPAP decreases air leaks compared to face mask interfaces, potentially reducing viral transmission when used to treat patients with AHRF from COVID-19. In different forms of acute hypoxic respiratory failure, H-CPAP may increase recruitment of non-aerated alveoli in dependent pulmonary regions,25,26 thereby increasing lung functional residual capacity and decreasing shunt. In theory, the tidal volume is shifted with H-CPAP to a more compliant part of the pressure-volume curve, thus reducing the patient’s effort and work of breathing (WOB) and oxygen consumption27,28 despite absence of ventilatory assistance. In the less severe forms of ARDS when spontaneous effort remains modest, there is an improved gas exchange and better lung aeration in CT analysis in experimental and clinical studies.29 By decreasing alveolar collapse and inhomogeneity of pulmonary gas distribution without imposing a higher tidal volume, CPAP may decrease lung injury induced by vigorous diaphragmatic contraction in dorsal regions.30 The presumed mechanism of diaphragmatic injury to the lungs is thought to be due to strong inspiratory efforts and large transpulmonary pressure swings that should be avoided to prevent an adverse effect of Pendelluft and large local tidal volume on baby lungs.31 Comparative physiological studies have demonstrated the equal performance of helmet and mask CPAP for reducing the inspiratory effort and WOB32; however, H-CPAP may increase the duration of positive pressure application because of improved tolerability by patients.33
Currently, both noninvasive CPAP and HFNT are first-line treatments for AHRF in immunocompromised patients.26 In several recent meta-analysis of trials in adults with AHRF, treatment with NRS including H-CPAP was associated with a lower risk of death, decreased intubation compared with standard oxygen therapy.24,34
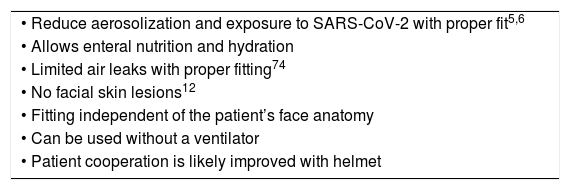
The different considerations for H-CPAP use are summarized in Table 1.
Major benefits and challenges of H-CPAP compared to face mask.
| • Reduce aerosolization and exposure to SARS-CoV-2 with proper fit5,6 |
| • Allows enteral nutrition and hydration |
| • Limited air leaks with proper fitting74 |
| • No facial skin lesions12 |
| • Fitting independent of the patient’s face anatomy |
| • Can be used without a ventilator |
| • Patient cooperation is likely improved with helmet |
| Challenges |
|---|
| • Large dead space needing fresh high flows |
| • Noise |
| • Possible Claustrophobia |
| • Armpits and neck skin breakdown |
| • Eye irritation |
| • Possible Claustrophobia |
| • Clinician team learning curve |
| • Achieving clinician education, engagement and acceptance of H-CPAP as a treatment option that improves outcomes |
In 2016, a major American academic medical center showed helmet NRS (pressure support ventilation) to decrease intubation rates and ICU length of stay in patients with mild to moderate ARDS when compared to mask NRS.33
Patients with COVID-19 and shunt-related hypoxemia may have a variable WOB and may respond favorably to CPAP, especially during type L CARDS and severe hypoxemia.20 A successful response to CPAP can most likely be expected when lung elastance and congestion are still low and clinical signs of excessive inspiratory efforts (i.e. use of accessory muscles) are still absent.20 Currently available data regarding the safety profile of H-CPAP mostly from Europe15,35,36 suggests that H-CPAP is a helpful tool for NRS in mild to moderate CARDS and may mitigate the ICU bed shortage during a COVID surge as well as a decreased need for intubation/mechanical ventilation. Recently, Franco et al. reported using H-CPAP as a first line NRS in 49% of CARDS patients and only 25% of them required invasive mechanical ventilation after their initial treatment.37
Within the US, Gaulton et al. found that H-CPAP decreased the odds of intubation by over 80% compared to HFNT in obese and overweight patients with AHRF from COVID-19.38 Additionally, H-CPAP as part of a ventilation strategy for COVID-19 patients has been supported by the Society for Critical Care Medicine and was integrated in their guidelines as early as March 2020.39
H-CPAP respiratory failure management for COVID-19 patientsThe construction of the helmet typically includes a transparent, latex free, polyvinylchloride hood joined to a metal or plastic ring that incorporates a soft polyvinylchloride collar adjustable to different neck circumferences. Underarm straps may be attached to the front and back of the durable ring to prevent upward displacement of the helmet when gas flow is initiated.32 Prior to the COVID-19 pandemic in the US, Food and Drug Administration (FDA) approval for helmets was limited to the use for gas delivery in a hyperbaric chamber. In response to the pandemic, the FDA has issued Emergency Use Authorizations (EUAs) to several manufacturers for helmet use in the treatment of AHRF from COVID-19. At the time of this publication, helmet EUAs have been granted to the StarMed CaStar R Hood (Intersurgical, Berkshire, UK) and the Subsalve Oxygen Treatment Hood (Lombardi Undersea LLC, Middletown, RI).40 Additional US helmet manufacturers include Sea-Long Medical Systems, (Waxahachie, TX), and Amron International Inc., (Vista, CA) and non-US based H-CPAP options are also available.41
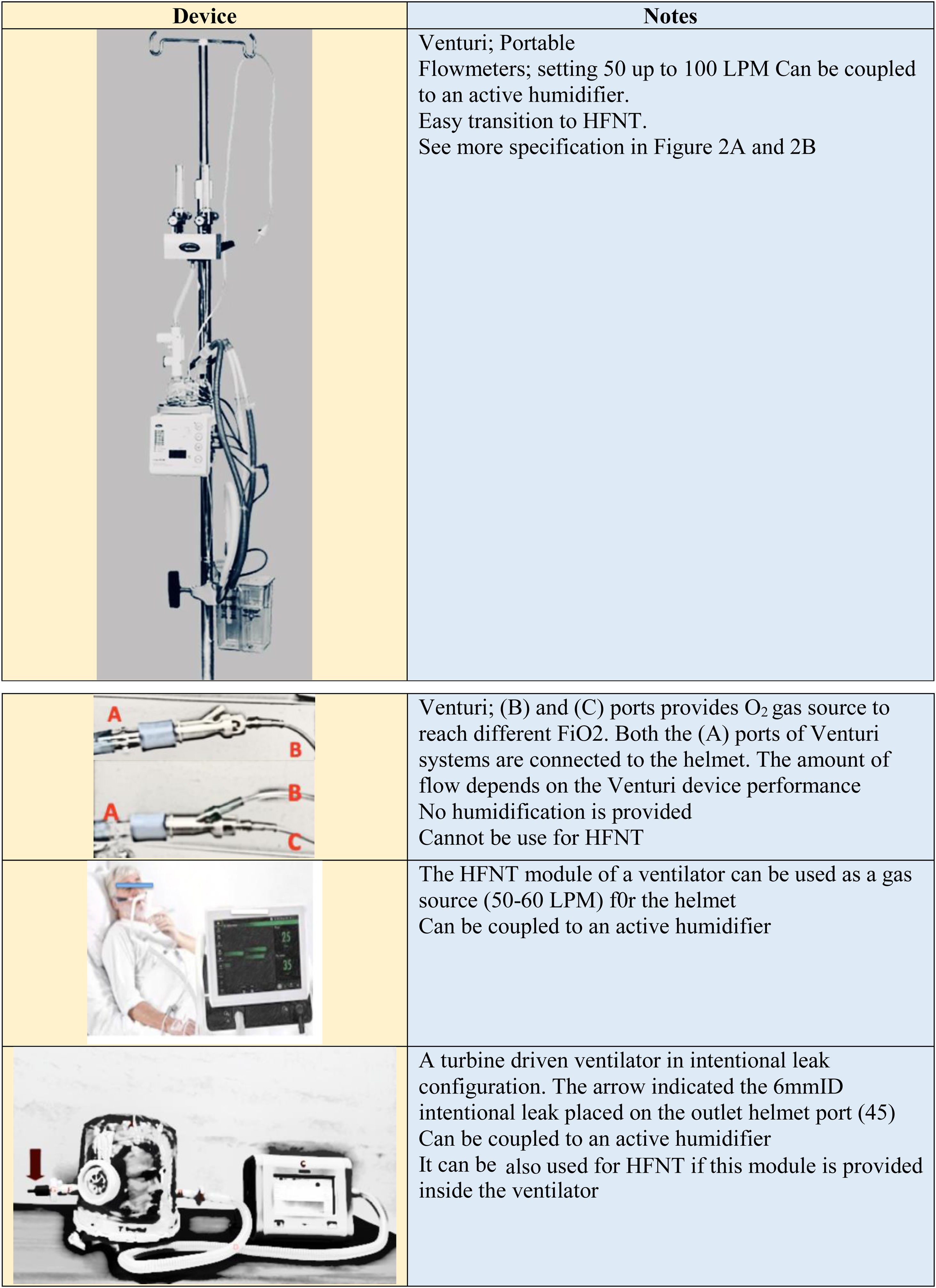
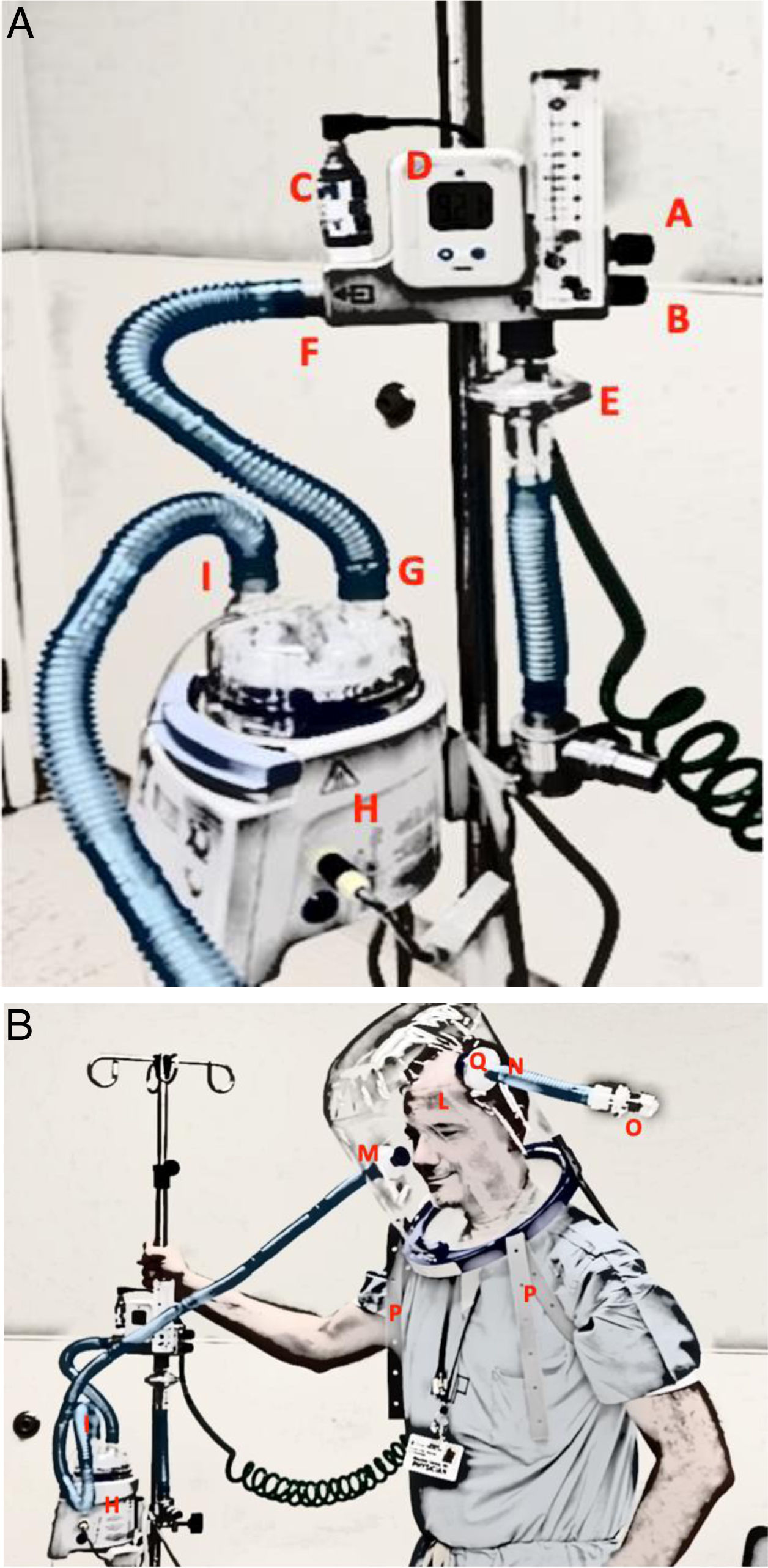
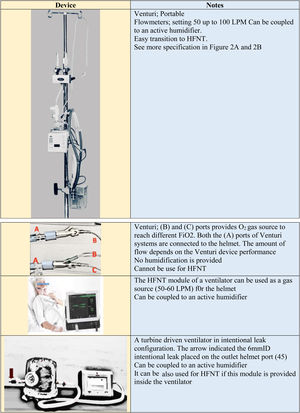
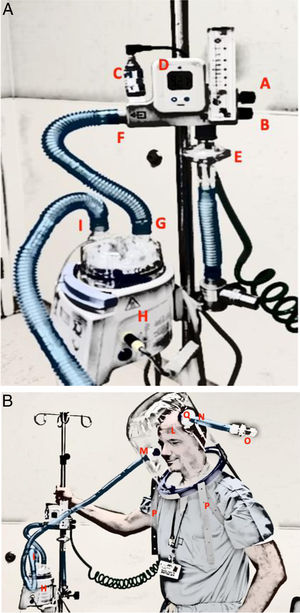
Setup and gas sourceSeveral configurations are possible based on equipment availability (Fig. 1). The MaxVenturi setup (Fig. 2) is preferred as it allows for natural humidification, low noise burden, easy transition to HFNT during breaks and is a simple and safe set-up for patient movement and transport. PEEP may be selected to start at 5 cm H20 and can be titrated to a maximum of 15. For use in cases of COVID-19, a viral filter can be placed on the inspiratory and expiratory limbs to reduce viral transmission. An arterial blood gas analysis (ABG) prior to and after start of H-CPAP is desirable, but scheduled ABGs might not be necessary. Carbon dioxide rebreathing is common but can easily be mitigated by keeping continuous inspiratory flow >50 L per minute using the oxygen delivery systems shown in Fig. 1.42 PEEP valve features may also affect CPAP performance. Precalibrated and water seal valves exhibit the best performance.43
Flow delivery system configuration: MAX VENTURI System connected to a helmet.
A: A MAX VENTURI system is provided with 2 knobs to independently set oxygen and air. Knob (A) regulates oxygen percentage, Knob (B) regulates air, (C) oxygen cell and read on the display (D). protected by a HEPA filter (E). The outlet of the venturi system is connected to the inlet port (G) of the water chamber of an active humidifier (H) through an insulated circuit (F) From the outlet port of the water chamber another insulated circuit (I) connects the helmet inlet port as shown in B. B: A MAX VENTURI system is connected to the helmet (L) inlet port (M) through an insulated circuit (I) coming from the water chamber of the humidifier (H). The expiratory helmet port (N), protected with a HEPA filter (Q), is provided with a PEEP valve (O). Two armpit braces (P) keep the helmet in place. MAX VENTURI can be coupled to an active humidifier.
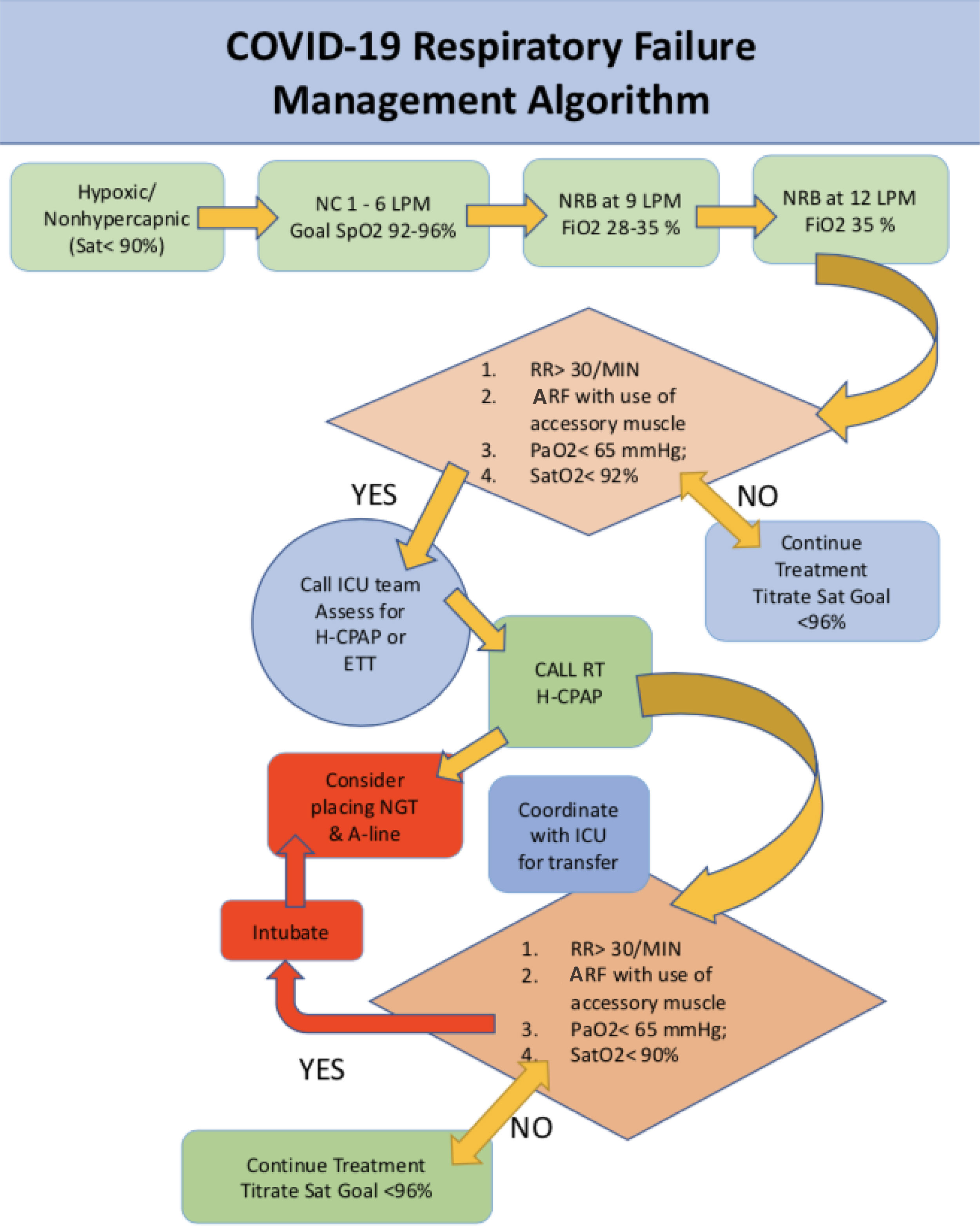
H-CPAP management is most practically targeted to achieve peripheral oxygen saturation (SpO2) > 92%. Initiating CPAP treatment should depend on the assessment of the PaO2/FiO2 ratio rather than on SpO2 alone.9 HCPAP treatment may be initiated and maintained based on the PaO2/FiO2 ratio, when there is a concern about falsely elevated SpO2 from an early COVID-19 stage induced respiratory alkalosis and an associated left shift of the oxygen–hemoglobin dissociation curve.11 A Respiratory Failure Management Algorithm for COVID-19 Patients that integrates H-CPAP is presented in Fig. 3.
Considerations specific to H-CPAPCarbon dioxide rebreathing and tidal volume measurementThe degree of CO2 rebreathing influencing the inspired partial pressure of CO2 (PiCO2) depends on the CO2 produced by the patient and the total fresh gas flow that clears the helmet. There are some data suggesting that reducing the internal volume of the helmet does not automatically prevent rebreathing but the increase in gas flow and the rate of CO2 production will affect CO2 rebreathing.44,45
Patroniti et al45 found that with an increase of gas flow from 20 to 60 L/min and of 0 PEEP to 15 cmH2O during H-CPAP, the inspiratory CO2 concentration was around 2.3 mmHg higher with helmet than with mask NRS. Increasing the gas flow rate significantly lowered the inspiratory CO2 concentration in patients with H-CPAP.
So far, H-CPAP does not allow tidal volume measurement during use due to its mechanical properties. However, in the setting of H-CPAP with a turbine driven ventilator, an intentional leak, and dedicated software, tidal volume can be estimated.46–48
HumidificationAlthough the optimal level of humidification of inspired gases during NRS is unknown, inadequate humidification can cause patient distress and NRS intolerance.49,50 Adding active humidification set at body temperature may result in fogging of the helmet visor, which can also cause discomfort. When using a Venturi system, like the one shown in Fig. 2, to supply fresh gas, the entrained room air increases humidity compared to dry medical gas alone, depending on the chosen fraction of oxygen. Furthermore, the humidity and temperature of expired gas can mix with the dryer and cooler fresh gas, enhancing its temperature and humidity and reducing the need for active humidification. Chiumello et al.,51 reported that during continuous flow H-CPAP and spontaneous breathing without active humidification, the temperature and humidity of the inspired gas was significantly higher compared to non-humidified medical gas alone. The magnitude of this effect was directly dependent on the gas flow passing through the helmet. Hence, in the absence of active humidification during high flow H-CPAP, insufficient humidification of gas may develop depending on the gas flow and oxygen fraction.51,52 If humidification is chosen (e.g. when patients require more oxygen), the modern actively heated humidifiers are able to deliver an absolute humidity above 10 mgH2O/L. The use of an active humidifier set at room temperature improves absolute and relative humidity inside the helmet and prevents insufficient humidification while reducing fogging.
ProningProne positioning in spontaneously breathing patients with AHRF may improve oxygenation and prevent intubation and has demonstrated utility in COVID-19.53–56 Switching to prone position changes pulmonary perfusion, diverting blood flow toward the high Va/Q areas, and increases ventilation in the dorsal, now nondependent areas of the lung.54 A redistribution of aerated and non-aerated areas of the lung occurs with proning. This maneuver improves oxygenation at a lower level of PEEP with more homogeneous distribution of ventilation and a decreased risk of ventilator–induced lung injury.29,35 Anatomically, dorsal lung regions have a higher density of pulmonary vessels independent of gravity.57,58
Prone positioning in patients with COVID-19 who are receiving H-CPAP is safe, feasible, and may improve oxygenation and reduce work of breathing. In a study of 15 CARDS patients receiving H-CPAP in the prone position outside the ICU, a reduced respiratory rate compared to their baseline that was maintained after the end of pronation was observed.36 All patients exhibited an improved PaO2/FIO2 ratio in the prone position and 12 patients (80%) had an enhanced PaO2/FIO2 ratio after the end of proning; 11 (73.3%) patients reported an improved level of comfort during proning in a very recent prospective study where H-CPAP was used in 79% of the patients. Moreover, Coppo et al. found that prone positioning with H-CPAP was feasible and effective in rapidly improving blood oxygenation in awake patients with COVID-19-related pneumonia requiring oxygen supplementation.59
Care should be taken to prevent inspiratory flow disconnection during positioning. A soft chest support may be placed under the patient so as to better align the head position with the body axis when in a helmet. A towel may be placed inside the helmet to prevent head skin contact with the plastic neck rim for instances when the patient’s head may rest against the mattress.
Like any other noninvasive ventilation technique, use of sedatives during H-CPAP application may trigger safety concerns of potential aspiration and hypoventilation.
NoiseOperating noise of helmets compared to masks has been reported as a barrier to helmet use.60,61 Noise contributes to patient discomfort during the ICU stay,62,63 and noise exposure during H-CPAP can be underestimated among the factors that influence the patient’s well-being. The magnitude of gas flow is the origin of the noise generation for the different CPAP gas sources. High efficiency particulate air filters on the inspiratory limb of the gas circuit can help to reduce noise provided that active humidification is not used. Filters are recommended to reduce viral transmission. Ear plugs can be worn by patients during helmet use if so desired.
Nursing care and patient comfortA well seated and maintained helmet is generally better tolerated than the mask NRS, especially for extended CPAP therapy over several days.64–67 Use of H-CPAP compared to a face-mask interface may also reduce air leaks and thus potential health-care worker COVID-19 particle exposure and alleviate related anxiety triggered by the use of positive pressure NRS devices.68 Helmet technology improves patients’ comfort, allows patients’ communication, interaction, coughing and oral feeding.63 Rare problems of H-CPAP include dermal decubiti or even skin necrosis at the neck, gastric distension or eye irritation.64,65 The helmet often features an anti-suffocation valve to allow air entry during any fresh gas flow interruption.41 This feature is of utmost importance when helmet is used outside the ICU in the case gas source failure to prevent severe rebreathing.45
Appropriate patient selection and education of a cooperative patient and careful H-CPAP management are fundamental to minimize claustrophobia and preserve the patient’s full visual contact and communication with health care providers and relatives.45,52,69,70 H-CPAP is thought to also improve sleep possibly reducing the rate of delirium compared to intubation.71 An H-CPAP bundle has been proposed by Lucchini et al. including noise reduction measures, a counter- weight fixation method and a heated wire active humidification system to further improve the patient’s comfort.72 H-CPAP should be maintained around the clock whenever possible. However, brief interruptions to improve the ease of feeding and provide a short H-CPAP holiday can be considered. A simple transition to HFNT is feasible with the MaxVenturi setup. This may reduce the amount of time a provider spends in a contaminated environment.
Typically, H-CPAP sessions last at least 6 h continuously followed by a break for meals (Table 2). Discomfort is a major cause of NRS failure.69 Similar to invasive mechanical ventilation, sedation has been advocated to improve NRS success. However, patients undergoing CPAP therapy cannot be heavily sedated.69 Dexmedetomidine is a preferred agent for sedating patients receiving H-CPAP in the ICU when necessary.73
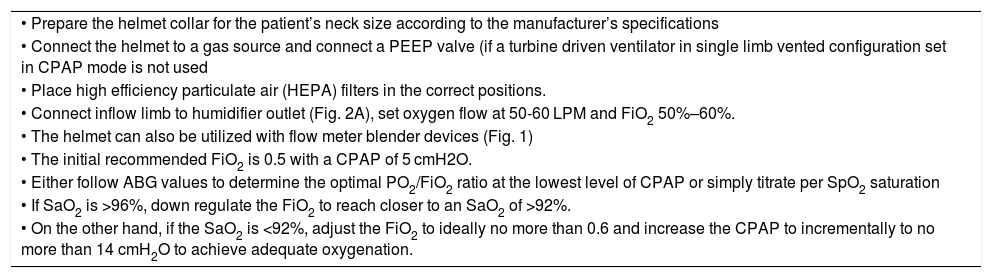
Setup helmet and O2 delivery.
| • Prepare the helmet collar for the patient’s neck size according to the manufacturer’s specifications |
| • Connect the helmet to a gas source and connect a PEEP valve (if a turbine driven ventilator in single limb vented configuration set in CPAP mode is not used |
| • Place high efficiency particulate air (HEPA) filters in the correct positions. |
| • Connect inflow limb to humidifier outlet (Fig. 2A), set oxygen flow at 50-60 LPM and FiO2 50%–60%. |
| • The helmet can also be utilized with flow meter blender devices (Fig. 1) |
| • The initial recommended FiO2 is 0.5 with a CPAP of 5 cmH2O. |
| • Either follow ABG values to determine the optimal PO2/FiO2 ratio at the lowest level of CPAP or simply titrate per SpO2 saturation |
| • If SaO2 is >96%, down regulate the FiO2 to reach closer to an SaO2 of >92%. |
| • On the other hand, if the SaO2 is <92%, adjust the FiO2 to ideally no more than 0.6 and increase the CPAP to incrementally to no more than 14 cmH2O to achieve adequate oxygenation. |
Special straps loop around the axilla to secure the helmet in a comfortable position on the patient’s head. This configuration may cause dermal lesions despite padding and may result in H-CPAP discontinuation.72 An alternative design is an opening ring deployed underneath an inflatable cushion to prevent leaks and secure the helmet without the need for axillary straps. This design also reduces the ventilation pressure swings during H-CPAP74 and aerosolization.5,9
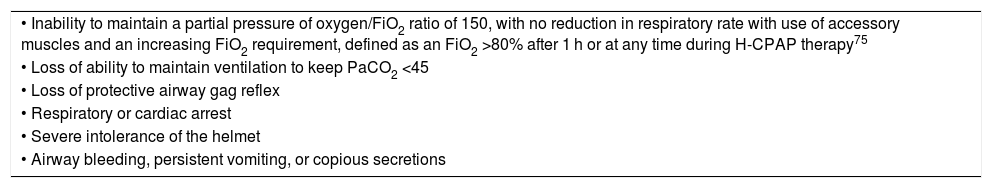
When to intubateIntubation should not be delayed in patients with AHRF from COVID-19 if H-CPAP does not improve Arterial Blood Gas parameters or the clinical status (Fig. 3), and the indication is no different from AHRF from non-COVID-19 etiologies. (Table 3). When increased respiratory drive, WOB, persistent dyspnea, and use of accessory muscles are present in combination, invasive mechanical ventilation should be instituted.75 Delayed intubation may increase the risk of clinical deterioration.28
Indications for intubation.
| • Inability to maintain a partial pressure of oxygen/FiO2 ratio of 150, with no reduction in respiratory rate with use of accessory muscles and an increasing FiO2 requirement, defined as an FiO2 >80% after 1 h or at any time during H-CPAP therapy75 |
| • Loss of ability to maintain ventilation to keep PaCO2 <45 |
| • Loss of protective airway gag reflex |
| • Respiratory or cardiac arrest |
| • Severe intolerance of the helmet |
| • Airway bleeding, persistent vomiting, or copious secretions |
Camporota et al.76 suggest that as dead-space ventilation increases, a greater respiratory drive generates a greater minute ventilation and WOB. This in turn results in a higher transpulmonary pressure as in other forms of AHRF.77 A greater contribution of viral aerosolization in this circumstance is also likely. These patients may be at higher risk of self-induced lung injury, which is thought to be caused by large diaphragmatic swings and increased WOB in patients receiving non-invasive mechanical ventilation.31 Such a situation worsens their clinical status by prolonging H-CPAP and eventually leads to unfavorable outcomes.76,78
Specific to COVID-19, the airway team should be activated as soon as the need for mechanical ventilation is anticipated, to allow for the appropriate donning of personal protective equipment, optimize procedural control and avoid an emergency airway management scenario. Fi02 can be increased to 1, if using a MaxVenturi or ventilator setup, for pre-oxygenation. The helmet can be removed prior to or after induction ensuring that there are two providers available to assist in helmet removal.
WeaningCurrently, no general consensus exists regarding H-CPAP weaning process in COVID-19. Therefore, we propose a sound clinical approach with individualized care for patients with AHRF due to CARDS based on comorbidities and the resolution of the respiratory impairment.
In our clinical experience, the patient can be gradually weaned from H-CPAP first by decreasing the PEEP, and FiO2, followed by incrementally increasing the H-CPAP free time. H-CPAP can be discontinued by achieving respiratory distress improvement and an ability to maintain a SpO2 > 96% on Fi022 ≤ 40% and CPAP 0−5 cmH20. When a PEEP of 5 cmH2O has been achieved, the H-CPAP may be replaced by an oxygen Venturi mask or HFNT if allowed (a surgical mask can decrease aerosol dispersion).79
ConclusionsH-CPAP is not intended to replace endotracheal intubation and mechanical ventilation in AHRF from COVID-19. Instead, as an option for respiratory support with evidence of effective and safe use in many parts of the world, it deserves consideration for more widespread use during a pandemic.76
H-CPAP, when properly fitted, is associated with minimal particle dispersion and air contamination,5,6,9 reducing the risk of transmission to healthcare workers.
Clinician concerns with H-CPAP regarding the risk of viral contamination during use, the possibility of device malfunction, and patient decompensation can be alleviated with education, scientific evidence, and mentored experience.
Life-long learning, an open mind, and a positive attitude to new, life-saving treatments remain cornerstones for successful new program implementation. We must accept a learning curve for the benefit of many patients.
FundingSupport was provided solely from institutional and/or department resources. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.