The aim of this study was to develop and validate the professional translation and cultural adaptation of the Portuguese Severe Respiratory Insufficiency (SRI) Questionnaire.
The sample was composed of 93 patients (50 male patients, 53.8%) with a mean age of 66.3 years. The most frequent diagnostic groups were chronic obstructive pulmonary disease, obesity hypoventilation syndrome and restrictive chest wall disorders.
The patients were asked to fill in both the SRI and SF-36 questionnaires. Factor analysis of the SRI questionnaire was performed leading to an explained variance of 73%, and resulted in 13 components. When analyzing the reliability, we obtained values for Cronbach's alpha above 0.70 for most subscales with the reliability of the summary scale being even higher (0.84).
This professional translation and cultural adaptation of the Portuguese SRI Questionnaire has good psychometric properties which are similar, not only to the original, but also to other translations. These characteristics make this questionnaire applicable to the Portuguese population receiving home mechanical ventilation for severe respiratory insufficiency.
Non-invasive ventilation (NIV) is indicated in patients with chronic severe respiratory insufficiency of different causes. Not only the underlying disease, but also the intervention can have a deep impact on the patients’ quality of life.
Health-related quality of life (HRQL) questionnaires are multidimensional tools that explore aspects of patients’ lives that are not covered by other diagnostic tools. Even though it is a complex task, they are an invaluable source of information on how disease affects a patient's life, and they should be sensitive to changes related to progression of disease or treatment interventions.1 HRQL questionnaires have gained increasing importance in recent years in both research and clinical settings.1
In general, specific HRQL questionnaires are designed and validated for specific and highly prevalent diseases such as asthma or chronic obstructive pulmonary disease. Until recently, there was no questionnaire for patients with severe respiratory insufficiency requiring home mechanical ventilation (HMV), regardless of the underlying disorder.
The Severe Respiratory Insufficiency (SRI) Questionnaire is a multidimensional instrument with high psychometric properties designed to measure specific HRQL in patients with respiratory insufficiency receiving HMV.2 It was originally developed in German, but has recently been professionally translated into several languages such as Spanish,3,4 English,5 Danish, Dutch, French, Japanese, Norwegian, Polish and Swedish6 and most of these translations have already been validated or are currently being validated. Moreover, it has also been validated and used in many recent studies on NIV.7–11
It is the aim of the international SRI project to stimulate research activities in the field of HRQL and home mechanical ventilation. For that purpose both the original version and the translated versions of the SRI are provided on the website of the German Respiratory Society free of charge for non-profit research activities.6
The objective of this study was to produce and validate the professional translation and cultural adaptation of the SRI into Portuguese. The results obtained were also compared with the Portuguese version of the SF-36 questionnaire.12–14 The SF-36 is a widely used and validated questionnaire to evaluate HRQL. Contrary to SRI questionnaire, which has been specifically developed for respiratory patients, SF-36 is a general HRQL measure that applies to the general population, as well as to patients suffering from different pathologies. Therefore, we found it useful, not only to compare both questionnaires in our sample population, but also to compare our results with reference values for SF-36 for the general Portuguese population.14
MethodsQuestionnairesThe SRI Questionnaire is a self-administered questionnaire containing 49 items that patients score on a 5-point Likert-scale (1: completely false; 2: quite false; 3: partly true/partly false; 4: quite true; 5: completely true) according to how true each statement has been for them in the preceding week. The questionnaire contains 7 HRQL domains, or subscales, and is designed in such a way that each item belongs to just 1 subscale. The 7 subscales are: respiratory complaints (SRI-RC) – 8 items, physical functioning (SRI-PF) – 6 items, attendant symptoms and sleep (SRI-AS) – 7 items, social relationships (SRI-SR) – 6 items, anxiety (SRI-AX) – 5 items, psychological well-being (SRI-WB) – 9 items and social functioning (SRI-SF) – 8 items. The final score for each subscale is calculated, after recoding certain items, by the corresponding percentage. The summary score (SRI-SS) is obtained by calculating the arithmetic mean of the subscale scores, in such a way that this calculation would not be possible if any of the scores were missing. A high overall score indicates a good HRQL, while a low overall score indicates a poor HRQL.2
The SF-36 consists of eight subscales (0–100) measuring different aspects of health status with lower scores indicating poorer health or higher disability: SF-36-PF (physical functioning); SF-36-RP (role-physical); SF-36-BP (bodily pain); SF-36-GH (general health); SF-36-VT (vitality); SF-36-SF (social functioning); SF-36-RE (role-emotional) and SF-36-MH (mental health).12,13
Portuguese translation and cultural adaptationThe Portuguese translation was obtained from the original German questionnaire, using the translation-back translation process by two independent professional translators.15
The equivalence of the back-translated items to the original items was evaluated and grouped into 3 categories according to previous recommendations3: category A: items that were fully equivalent; category B: items that were not fully equivalent or that contained different wording, but the content is similar; and category C: items that were not equivalent or that needed to be checked. Items rated A and B were left as they were and items rated C were reevaluated and rephrased accordingly with both of the independent translators being involved and the original questionnaire creator. The final version was written according to the New Portuguese Spelling Reform.
ValidationThis study was conducted in the Pneumology Department at Centro Hospitalar de Vila Nova de Gaia/Espinho (Portugal), a tertiary care teaching hospital. Ethical approval was obtained from the hospital Ethics Committee.
Patients with chronic hypercapnic respiratory failure, from a wide variety of causes, established on HMV for at least 30 days were eligible for the study. Exclusion criteria were refusal to participate and an exacerbation in the preceding 3 months.
The patients were asked to fill in both the SRI and SF-36 questionnaires. Patients were also asked to take home another SRI Questionnaire, to complete it 15 days later and to mail it back to the corresponding author.
Patients were categorized into six categories: chronic obstructive pulmonary disease (COPD), restrictive chest wall disorders (RCWD), obesity hypoventilation syndrome (OHS), combined COPD and obstructive sleep apnea (COPD+OSA), neuromuscular disorders (NMD), and other pathologies (miscellaneous).
Statistical analysisData are presented with mean and standard deviation or median and interquartile range. T-test was used to assess differences between two groups; comparisons between the different pathologies (with respect to age, BMI, FEV1% and FVC%) were performed using one-way analysis of variance (ANOVA). Normality was assessed with the Kolomogorov test. In the case of normality or homogeneity of variance assumptions were not verified, variables like BMI and FEV1% were log transformed; in the case of FVC%, the Kruskal–Wallis (KW) test was used. Post hoc comparisons were based on Tukey's HSD or on the Mann–Whitney (MW) test with a Bonferroni correction.
Statistical computations were performed with IBM SPSS Statistics for Windows, Version 23.0 (Armonk, NY: IBM Corp.). Two tailed significance assumed for p<0.05.
ResultsConsidering the translation-back translation process, there were 4 items originally listed as C: questions 13, 14, 18 and 33 – which after careful revision all of discrepancies were found to be related to the back translation from Portuguese to German and all the items were approved by all the parties involved.
The sample was composed of 93 patients, with a slight predominance of males (50 patients, 53.8%) and a mean age of 66.3 years. All patients were Portuguese native speakers.
The most common diagnostic groups were COPD, OHS and RCWD, corresponding to more than three quarters of the patients. The miscellaneous group included 2 patients with interstitial lung disease (1 idiopathic pulmonary fibrosis and 1 lymphangioleiomyomatosis) and 1 patient with bronchiectasis, COPD and kyphoscoliosis.
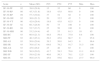
The clinical characteristics of the sample are summarized in Table 1. Pressure support ventilators were used in 87 cases (93.5%) and the most commonly used interface was nasal mask (78 patients; 83.9%). 57 patients (61.3%) required supplemental oxygen during ventilator use (mean flow rate: 1.1L/min). All patients had adapted well with no or just minor adverse effects.
Patients characteristics.
| Categories | COPD | OHS | RCWD | COPD+OSA | NMD | Miscellaneous | Total |
|---|---|---|---|---|---|---|---|
| Patients N (%) | 32 (34.4) | 23 (24.7) | 16 (17.2) | 11 (11.8) | 8 (8.6) | 3 (3.2) | 93 |
| Age (years) | 69.3 (11.5) | 64.7 (14.0) | 66.4 (10.4) | 69.9 (9.4) | 51.1 (13.4) | 73.7 (5.5) | 66.3 (12.6) |
| Sex (% male) | 71.9 | 17.4 | 50.0 | 72.7 | 87.5 | 0 | 53.8 |
| BMI (kg/m2) | 29.6 (6.8) | 47.2 (11.5) | 25.6 (5.0) | 33.8 (4.6) | 29.6 (7.9) | 28.6 (2.8) | 33.8 |
| HMV (h/d) | 7.4 (1.6) | 7.9 (1.8) | 7.7 (1.7) | 7.6 (1.3) | 7.1 (2.0) | 8.4 (1.4) | 7.6 (1.6) |
| HMV (months) | 43.0 (24.8–80.0) | 72.0 (26.0–103.0) | 44.0 (20.5–112.5) | 54.0 (24.0–78.0) | 23.5 (10.5–69.3) | 26.0a | 46.0 (23.5–90.5) |
| pH | 7.42 (0.03) | 7.42 (0.02) | 7.42 (0.04) | 7.40 (0.03) | 7.39 (0.03) | 7.43 (0.02) | 7.42 (0.03) |
| PaCO2 (mmHg) | 46.9 (6.9) | 41.5 (4.5) | 46.1 (4.5) | 47.7 (5.9) | 48.2 (7.5) | 47.7 (3.8) | 45.7 (6.2) |
| PaO2 (mmHg) | 71.9 (9.1) | 73.4 (11.6) | 73.8 (13.0) | 68.4 (8.0) | 75.8 (7.7) | 79.5 (7.4) | 72.8 (10.3) |
| HCO3 (mmol/L) | 29.4 (3.5) | 26.4 (2.4) | 28.9 (2.5) | 28.2 (3.4) | 27.6 (2.5) | 30.8 (0.3) | 28.4 (3.1) |
| FEV1 (% predicted) | 34.2 (26.0–48.8) | 65.0 (51.0–89-6) | 35.5 (21.7–45.8) | 51.6 (44.5–58.0) | 37.0 (32.0–55.0) | 26a | 44.5 (30.6–57.9) |
| FVC (% predicted) | 59.1 (49.6–72.3) | 76.0 (60.0–101.0) | 43.0 (24.0–54.8) | 70.2 (59.6–86.0) | 44.0 (30.0–55.0) | 42.2a | 59.0 (47.0–75.0) |
Abbreviations: COPD, chronic obstructive pulmonary disease; OHS, obesity-hypoventilation syndrome; RCWD, restrictive chest wall disorders; COPD+OSA, combined COPD and obstructive sleep apnea; NMD, neuromuscular disorders; BMI, body mass index; HMV, home mechanical ventilation; FVC, forced vital capacity; FEV1, forced expiratory volume in one second.
Note: values are presented as mean and standard deviation, with the exception of months with HMV, FEV1 and FVC, which are presented as median and 25–75 quartiles.
The vast majority of the questionnaires were self-administered. Thirty patients required help, because they were unable to read, did not bring their reading glasses or were physically too disabled to write. Patients took approximately 10–15min to complete each questionnaire.
Regarding the completion of the questionnaires, in the SRI the overall missing values for each item was below 3%, with the exception of question 31 (“My marriage/relationship is suffering because of my illness”), to which 9.7% patients did not reply, most of them stating they were not currently in a romantic relationship. In the SF-36 we observed that, with the exception of questions 4a, 4c, 7, 8 and 9d, all other questions had missing values below 5.5%. The remainder questions had missing values between 5.5 and 9.7%, with the highest missing responses being related to marriage (question 8) and work (4c and 4d).
Descriptive data of both the SRI and the SF-36 questionnaires are provided in Table 2. With the exception of SRI-SR, SRI-AX and SRI-SF, the other five subscales and the summary scale were normally distributed which means the SRI covered a broad range of the possible questionnaire's scaling range. The mean score of the SRI-SS (mean 56.6, SD 15.7) was roughly in the middle of the questionnaire's scaling range. In contrast, in the SF-36 questionnaire, only the SF-36-MH subscale was normally distributed.
SRI and SF36 questionnaires subscales’ results.
| Scale | n | Mean (SD) | P25 | P50 | P75 | Min. | Max. |
|---|---|---|---|---|---|---|---|
| SF-36-PF | 92 | 39.0 (28.6) | 15 | 35 | 60 | 0 | 100 |
| SF-36-RP | 86 | 45.3 (31.8) | 18.8 | 43.8 | 68.8 | 0 | 100 |
| SF-36-BP | 89 | 57.3 (30.4) | 37 | 52 | 92 | 0 | 100 |
| SF-36-GH | 92 | 36.6 (21.2) | 20 | 32.5 | 45 | 5 | 100 |
| SF-36-VT | 90 | 42.9 (26.4) | 18.8 | 43.8 | 62.5 | 0 | 100 |
| SF-36-SF | 92 | 66.3 (28.9) | 50 | 75 | 100 | 0 | 100 |
| SF-36-RE | 88 | 52.7 (33.7) | 25 | 50 | 100 | 0 | 100 |
| SF-36-MH | 90 | 53.2 (14.4) | 45 | 55 | 61.3 | 10 | 85 |
| SRI-RC | 93 | 60.9 (21.3) | 44.8 | 59.4 | 75.0 | 9.4 | 100 |
| SRI-PF | 93 | 46.3 (25.1) | 29.2 | 45.8 | 66.7 | 0 | 95.8 |
| SRI-AS | 93 | 50.6 (20.4) | 39.3 | 50.0 | 64.3 | 0 | 96.4 |
| SRI-SR | 93 | 76.6 (17.4) | 64.6 | 79.2 | 91.7 | 31.3 | 100 |
| SRI-AX | 93 | 45.6 (26.0 | 25 | 40 | 65 | 0 | 100 |
| SRI-WB | 93 | 56.9 (20.2) | 41.7 | 58.3 | 70.8 | 11.1 | 88.9 |
| SRI-SF | 93 | 58.9 (23.0) | 40.6 | 56.3 | 78.1 | 12.5 | 100 |
| SRI-SS | 93 | 56.6 (15.7) | 45.0 | 55.6 | 68.4 | 27.7 | 90.0 |
P25, P50 and P75: 25, 50 and 75th percentiles. SF-36 scales: SF-36-PF: physical functioning; SF-36-RP: role-physical; SF-36-BP: bodily pain; SF-36-GH: general health; SF-36-VT: vitality; SF-36-SF: social functioning; SF-36-RE: role-emotional; SF-36-MH: mental health.
SRI scales: SRI-RC: respiratory complaints; SRI-PF: physical functioning; SRI-AS: attendant symptoms and sleep; SRI-SR: social relationships; SRI-AX: anxiety; SRI-WB: psychological well-being; SRI-SF: social functioning; SRI-SS: summary scale.
Table 3 presents SRI subscale results distributed by pathology and Table 4 shows the correlations between SRI and SF-36 subscales.
SRI results according to pathology groups.
| Categories | COPD | OHS | RCWD | COPD+OSA | NMD | Miscellaneous | Total |
|---|---|---|---|---|---|---|---|
| SRI-RC | 59.4 (20.2) | 63.5 (20.5) | 61.8 (21.6) | 54.4 (21.4) | 68.0 (30.6) | 59.4 (17.4) | 61.0 (21.3) |
| SRI-PF | 49.0 (24.2) | 41.6 (21.1) | 58.3 (21.3) | 44.3 (26.2) | 35.4 (37.8) | 23.6 (21.4) | 46.3 (25.1) |
| SRI-AS | 54.7 (18.7) | 45.3 (18.8) | 54.5 (17.3) | 38.0 (27.3) | 63.4 (19.4) | 39.3 (7.1) | 50.6 (20.4) |
| SRI-SR | 76.8 (19.0) | 73.0 (17.5) | 82.8 (15.0) | 73.5 (18.2) | 79.7 (16.7) | 72.2 (2.4) | 76.6 (17.4) |
| SRI-AX | 44.0 (25.4) | 53.3 (21.5) | 46.3 (24.6) | 32.3 (31.3) | 52.5 (33.5) | 40.0 (27.8) | 45.9 (26.0) |
| SRI-WB | 57.4 (23.2) | 54.2 (17.0) | 64.1 (14.3) | 49.7 (20.5) | 61.5 (25.3) | 47.2 (20.5) | 56.9 (20.2) |
| SRI-SF | 57.9 (21.6) | 58.6 (26.7) | 66.4 (20.2) | 59.3 (19.0) | 55.5 (28.7) | 40.6 (21.9) | 58.9 (23.0) |
| SRI-SS | 57.0 (16.5) | 55.6 (15.1) | 62.0 (12.6) | 50.2 (16.2) | 59.4 (19.2) | 46.0 (13.3) | 56.6 (15.6) |
There were no statistically significant differences across the pathology groups with the exception for SRI-AS (ANOVA, F=2.9, p<0.05), with COPD+OSA patients with a statistical significant difference with NMD patients.
Correlation matrix between SRI and SF-36 subscales.
| SF-36-PF | SF-36-RP | SF-36-BP | SF-36-GH | SF-36-VT | SF-36-SF | SF-36-RE | SF-36-MH | SF-36-PHC | SF-36-MHC | |
|---|---|---|---|---|---|---|---|---|---|---|
| SRI-RC | 0.215* | 0.367** | 0.293** | 0.277** | 0.374** | 0.301** | 0.361** | 0.143 | 0.420** | 0.348** |
| SRI-PF | 0.584** | 0.665** | 0.406** | 0.452** | 0.692** | 0.580** | 0.641** | 0.248* | 0.800** | 0.610** |
| SRI-AS | 0.292** | 0.308** | 0.416** | 0.255* | 0.458** | 0.306** | 0.270* | 0.279** | 0.448** | 0.487** |
| SRI-SR | 0.258* | 0.328** | 0.302** | 0.285** | 0.349** | 0.543** | 0.345** | 0.248* | 0.441** | 0.460** |
| SRI-AX | 0.183 | 0.378** | 0.222* | 0.424** | 0.422** | 0.304** | 0.402** | 0.242* | 0.459** | 0.392** |
| SRI-WB | 0.424** | 0.425** | 0.356** | 0.501** | 0.689** | 0.542** | 0.483** | 0.349** | 0.624** | 0.599** |
| SRI-SF | 0.518** | 0.549** | 0.363** | 0.425** | 0.609** | 0.586** | 0.565** | 0.279** | 0.688** | 0.610** |
| SRI-SS | 0.505** | 0.594** | 0.468** | 0.515** | 0.712** | 0.621** | 0.606** | 0.351** | 0.759** | 0.690** |
All results were statistically significant with the exception of the correlation between SRI-RC with SF-36 MH.
When analyzing the reliability, we obtained values for Cronbach's alpha above 0.7 for most subscales, (SRI-RC 0.779; SRI-PF 0.713; SRI-AS 0.607; SRI-SR 0.441; SRI-AX 0.718; SRI-WB 0.748; SRI-SF 0.720) SRI-SR and SRI-AS being the exceptions. Compared to the reliability of the subscales, the reliability of the summary scale was even higher (0.838).
Test–retest reliability was assessed on 61 of the patients (65.6%) The time between test–retest was 15 days and answers were received between 16 and 25 days. The Intra Class Correlation coefficients presented a very good agreement (excellent >0.9, in the case of SRI-PF, SRI-SF and SRI-SS; very good >0.8, for SRI-RC, SRI-AS, SRI-SR, SRI-AX; good >0.7 for SRI-WB).
Structural validityIn this study, a factor analysis of the SRI questionnaire was performed leading to an explained variance of 73% and resulting in 13 components. In order to understand how these multidimensional components impact the different subscales, a separate factor analysis, for each subscale, was performed.
We found that the SRI subscales SRI-RS, SRI-PF, SRI-SR, SRI-AX, SRI-WB were divided into two components and the remaining subscales (SRI-AS and SRI-SF) were divided into three components. With respect to SRI-RC (explained variance – 56%), we found that one component included dyspnea related complaints and the other component cough and mucus production. Regarding SRI-PF (explained variance – 69%), the main component comprised self-care activities and other medium effort activities, such as climbing stairs. The SRI-SR (explained variance – 54%) is divided in a component that highlights isolation and loneliness symptoms and other regarding friendly relations. The two components of SRI-AX (explained variance – 69%) entailed stress and fear of disease progression/symptom exacerbation and questions related to shameful public situations. SRI-WB (explained variance – 57%) has one component that reflects negative feelings of irritation and sadness and the other that relates to happiness and optimistic attitudes. SRI-AS (explained variance – 66%) is divided in three components: attendant symptoms, other sleep-related complaints and sleepiness during the day. SRI-SF (63% of explained variance) presents one component that refers to social limitations, other to evening socializing and the third component to marital experience and hosting visitors. Lastly, applying factor analysis to the seven SRI subscales resulted in two components (67% of explained variance), one including anxiety, respiratory symptoms and sleep and attendant symptoms, and the other the remaining subscales.
Disease comparisonsOne way analysis of variance was used to compare pathologies (the miscellaneous group was excluded from the analysis due to its low number of patients). With respect to age, there are no significant differences between male and female patients. It is of notice that neuromuscular patients exhibit a statistically significant lower mean age with respect to the remaining pathologies.
Body mass index (BMI) was significantly (ANOVA, F=19.0, p<0.001) higher for SOH patients (HSD, p<0.01) when compared to the remaining pathologies; RCWD patients presented the lowest BMI, which was significantly different from COPD+OSA and OHS (HSD, p<0.05).
There were statistically significant differences with respect to FEV1% predicted (ANOVA, F=8.7, p<0.001), with COPD and RCWD patients with the lowest value and OHS with the highest one (significantly different from RCWD, COPD and NMD, HSD, p<0.05).
Concerning FVC% predicted, the Kruskal–Wallis test revealed the existence of statistically significant differences (Chi-sq=30.4, p<0.001), with RCWD patients presenting the lowest mean value and COPD+OSA and OHS the highest values (MW, p<0.01); there were no significant differences between COPD, COPD+OSA and OHS; between NMD, COPD and other pathologies and between RCWD, NMD and other pathologies. We found that there was no statistically significant difference in duration of NIV (in months) and average NIV use per night between pathology groups.
The SRI subscale that had the highest score for every pathology was SRI-SR, while the lowest scores were found for SRI-AX for COPD, RCWD and COPD+OSA and for SRI-PF for OHS, NMD and miscellaneous. We observed that COPD−OSA patients have a greater impact on the SRI-AS (p<0.05) and, although not statistically significant, COPD and COPD−OSA patients have lower SRI-RC scores, NMD patients have greater impact on SRI-PF and COPD+OSA patients have lower values for SRI-AX.
DiscussionThe SRI questionnaire is a disease-specific questionnaire with high psychometric properties, and is currently and progressively becoming the international standard tool to assess HRQL in patients with severe chronic respiratory failure.7–11 Our study shows that the Portuguese version of the SRI, which resulted from professional translation and back-translation of the original German version, has good psychometric properties and can be used in clinical studies assessing HRQL in patients with severe chronic respiratory failure receiving HMV.
It is worth noting that, even though the New Portuguese Spelling Reform has been implemented in order to unify the writing of Portuguese between different countries, not all the countries with Portuguese as the official language have accepted it. Also, some expressions are culture-dependent and may vary significantly between countries. Therefore, this translation is essentially valid only for Portugal.
The sample included patients with the most common diagnosis for starting HMV. Our study included a much higher percentage of COPD ventilated patients (46.2%) compared to the German (34.2%),2 Spanish (13.3%)4 and English (17%)5 validation studies. This reflects the data from the Eurovent study,16 in which Portugal has one of the highest percentages of lung/airway disease patients receiving HMV in Europe.
Two factors were extracted out of the subscales accounting for 72% of the total variance. These results are similar to the English validation – 70%5 and higher than the original German study – 59.8%.2
The questionnaire has good internal validity, since 5 out of 7 subscales had a Cronbach's alpha greater than 0.7 and the summary scale had an alpha greater than 0.8. These values are similar to the original and other language validation studies. The notable exception is the SRI-SR with a Cronbach's alpha of 0.441. As stated before, we found in the factor analysis that this subscale has 2 components – one that highlights isolation and loneliness symptoms and other that enhances friendly relations. In our study, we think patients might have considered that these 2 components do not necessarily measure the same concept and, thus, the low internal consistency of this subscale. As in previous studies, we found in our factor analysis, that more subscales in addition to the original seven could theoretically have been incorporated and this relates to the complexity of HRQL measuring in respiratory patients.4,5,17
This study found that HRQL is significantly impaired in home mechanically ventilated patients. The mean score of the SRI-SS (56.6) was approximately in the middle of the questionnaire's scaling range.
Comparing our SF-36 results with the general Portuguese population14 we observed that our patients have significantly lower mean scores, with approximately 20 points fewer in almost every subscale, with SF-36-PF showing the biggest difference (39.0 versus 80.2).
When compared to other language validations, we observed that the mean SRI-SS score 56.6 (SD=15.7) obtained was very similar to the Spanish 57.8 (SD=18.5)18 and English groups 55.9 (SD=18.9).5 This is quite interesting, considering the different pathology group distribution.
A significant concurrent validity was confirmed by the correlation analysis between scales of the SRI and scales of the SF-36 (Table 4). The major observed correlations are between SF-36 vitality, physical health component (PHC) and mental health component (MHC) subscales and the following SRI subscales: SRI-PF, SRI-SF and SRI-SS. It is worth noting that the composite or summary scales of both questionnaires have a good correlation. There might be some potential limitations to this study. Firstly, we studied a smaller sample than the previous validation studies. Secondly, the distribution of patients by pathology is different from other studies with a high predominance of COPD. Nonetheless, this study has the most common pathologies for HMV and this questionnaire is validated for ventilated patients independently of the causing disease. Therefore the authors feel that the global results are reliable.
ConclusionThis professional translation and cultural adaptation of the Portuguese SRI questionnaire has good psychometric properties and is similar, not only to the original, but also to other translations. These characteristics make this questionnaire applicable to the Portuguese population receiving home mechanical ventilation.
The Portuguese version of the SRI questionnaire and guidance for scoring can be downloaded, free of charge for research purposes, from the website of the German Respiratory Society.6
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical responsibilitiesNone.