Although non-invasive forms of ventilation have recently spread in neonatology, invasive ventilation still plays a key role in the support of extremely low birth weight (ELBW) infants. The purpose of this study was to assess changes in neonatal ventilation practices for ELBW infants and compare outcomes between two epochs (2005–2009 vs. 2010–2015) to analyze progression stemming from the implementation of newer clinical guidelines.
Materials and methodsWe conducted a retrospective study with data collection from all ELBW infants born between 2005 and 2015 in our center through their individual clinical records. The main outcome was the prevalence of bronchopulmonary dysplasia (BPD) in both periods. Assessment of other morbidities and survival were secondary outcomes.
ResultsA hundred and thirty-one infants were included; median gestational age of 27 weeks (23–33) and mean birth weight of 794.58g (±149.37). Invasive mechanical ventilation (IMV) was performed on 103 (78.6%) infants. Non-significant increases in the use of non-invasive mechanical ventilation (NIMV) were observed between epochs both exclusively and following IMV. In conventional ventilation there were significant variations between epochs, namely a decrease in synchronized intermittent mandatory ventilation (SIMV) and a major growth in the addition of volume guarantee (VG). Significant decreases in BPD (from 50.9% to 32.0%) and cystic periventricular leukomalacia (cPVL) (from 27.5% to 10.7%) were observed between epochs, with no major changes in other morbidities and survival.
ConclusionChanges in our neonatal intensive care unit's ventilatory practices according to the most up-to-date guidelines, have led to a decrease in BPD and cPVL, over an 11-year period.
Prematurity is associated with short- and long-term outcomes that account for higher rates of morbidity and mortality among infants.1 Concerning short-term complications, respiratory distress syndrome (RDS), also referred to as surfactant deficiency disease or hyaline membrane disease, is a common cause of death in the premature infant.2 This is a disorder primarily caused by deficiency of pulmonary surfactant in an immature lung. Its incidence and severity relate inversely to gestational age, making extremely low birth weight (ELBW) infants those at greatest risk.3
Over the last decades, changes in prenatal and neonatal care, such as the use of antenatal steroid therapy, early administration of positive airway pressure and exogenous surfactant therapy, have led to an improvement in morbidity and mortality rates.4 The role of mechanical ventilation in the neonatal intensive care unit (NICU) has also evolved markedly. Invasive ventilation has been implicated as a cause of lung injury and considered a major risk factor for bronchopulmonary dysplasia (BPD).5,6 These concerns have prompted neonatologists to take a different approach, preferring non-invasive forms of respiratory support as initial method of ventilation. These strategies have gained acceptance amongst neonatal units which now focus on quickly liberating patients from invasive support.7,8 Despite this trending approach, there continues to be an important place for invasive ventilation.9 In recent years, several ventilation modalities and strategies have been studied.10 Nonetheless, data concerning ventilation practices in neonatal units is scarce and it is not known whether results of studies have been translated to daily clinical practice.
Our study aimed to assess changes in neonatal ventilation practices for ELBW preterm infants admitted to a level III NICU over an 11-year period and compare outcomes between two epochs (2005–2009 vs. 2010–2015) in order to analyze progression stemming from the implementation of newer clinical guidelines.11
Materials and methodsA retrospective study was conducted with data collection of all ELBW (≤1000g) infants born between 2005 and 2015 in our center, a tertiary level reference center in the north of Portugal, through their individual clinical records. All newborns with major malformations or chromosomal anomalies, as well as those transferred to another hospital or deceased in the first 24h of admission were excluded.
Demographic, prenatal and delivery room data were collected. We registered ventilatory support and the need for supplementary oxygen, the prevalence of RDS, BPD and other major morbidities (namely pneumonia, neonatal sepsis, meningitis, patent ductus arteriosus (PDA), necrotizing enterocolitis (NEC), retinopathy of prematurity (ROP) (≥grade 2), periventricular venous infarction (PVI), hydrocephalus and cystic periventricular leukomalacia (cPVL)) and the need for and duration of parenteral nutrition, length of NICU stay and survival.
Gestational age (GA), contemplated as completed weeks of gestation, was determined as the best obstetric estimate considering the last menstrual period and fetal ultrasonography or, in the absence of obstetrical indexes, the New Ballard Score.12
Small for gestational age (SGA) was defined as a birthweight below the 10th percentile for gestational age and sex relative to the population standard.13,14
A full cycle of antenatal steroids was considered if either two doses of betamethasone or four doses of dexamethasone were administered before birth. We defined medication as any drug taken during pregnancy, with the exclusion of antibiotics, vitamins and supplements.
Clinical chorioamnionitis was diagnosed if maternal fever and two other suggestive signs (uterine tenderness, maternal or fetal tachycardia and foul/purulent amniotic fluid) were present.15 Histological chorioamnionitis was classified in agreement with Blanc's classification.16
Anemia of prematurity was defined according to reference ranges for blood hemoglobin concentration, considering gestational age.17
Early CPAP was defined by the application of continuous positive airway pressure through the nose during the initial resuscitation performed immediately after birth. Early surfactant was assumed when surfactant was administered to the infant in the initial resuscitation or as part of the stabilization immediately after birth.
Routine conventional ventilation included synchronized intermittent mandatory ventilation (SIMV), synchronized intermittent positive pressure ventilation (SIPPV) and pressure support ventilation (PSV), either with or without volume guarantee (VG), and was provided using the Babylog®8000 plus (Dräger, Lübeck, Germany) and, in recent years, by Fabian HFO (ACUTRONIC Medical Systems, Hirzel, Switzerland) in recent years. High frequency oscillatory ventilation (HFOV) was used as a rescue ventilation mode using the SensorMedics 3100A High Frequency Oscillatory Ventilator (SensorMedics Corporation, Yorba Linda, California, USA).
Infants who did not need to be invasively ventilated, or those whose general condition improved sufficiently for them to be extubated, were placed on nasal continuous positive airway pressure (nCPAP) or Bilevel nCPAP, consonant with their clinical status, using the Infant Flow®SiPAP system (CareFusion, Yorba Linda, California, USA).
Respiratory distress syndrome (RDS) was diagnosed according to clinical and radiographic features defined by the Vermont Oxford Network (VON).18 We used the classification I–III (I, mild; II, moderate; III severe) in line with the X-ray presentation, ranging from a light reticulogranular pattern with air bronchograms to white lungs, adapted from the Couchard's classification.19 BPD diagnose followed the severity-based consensus of the 2000 NICHD Neonatal Research report.20 The categories considered were mild and moderate/severe. The latter were grouped together for this study due to insufficient information concerning percentage of oxygen treatment at 36 weeks.
Neonatal sepsis was defined as any systemic bacterial or fungal infection documented by a positive blood culture. Neonatal sepsis was divided into early onset if infection occurred in the first 72h, or late onset if infection occurred after 1 week.21
The diagnosis of meningitis was assumed based on the criteria defined by VON. Meningitis was assumed when clinical suspicion was high and/or blood cultures were positive. When performed, a suggestive lumbar puncture with positive CSF growth gave the definite diagnosis.18 Hemodynamically significant PDA's diagnosis rested on echocardiographic findings (within the first 72h of life), being followed by serial evaluations until its closure.22 PDA medical treatment included indomethacin or ibuprofen. Surgical closure was performed if medical treatment was contraindicated or not successful.
NEC was classified conforming to modified Bell's criteria.23 Staging of ROP followed the International Classification.24 Only ROP grade 2 or higher was considered in this study. PVI was classified according to the modified Papile grading system.25 cPVL was determined accordingly to de Vries.26 The measures of Levene were used to classify hydrocephalus.27
Acidemia was defined as a pH<7.20.
The primary outcome of the study was to assess the incidence of BPD in both periods. Assessment of other morbidities and survival were secondary outcomes.
The study protocol was approved by our institution's ethics committee.
Statistical analysisCategorical variables were presented by absolute and relative frequencies, and continuous variables according to their distribution: we used mean (±standard deviation) for symmetrical and median (minimum–maximum) for asymmetrical distribution.
The statistical analysis was performed using IBM®SPSS®Statistics v.23 for Windows and a p value of <0.05 was considered significant. Chi-Square or Fisher tests were used to compare categorical variables, the latter for expected values below 5, while to study continuous variables, independent t test (symmetrical distribution) or Mann–Whitney U test (asymmetrical distribution) were used. For further analysis of the primary outcome, a multivariate analysis by logistic regression was executed, with the results displayed by odds ratio (OR), 95% confidence interval (CI), and p value.
ResultsPopulation characteristicsA total of 280 ELBW infants were born at our center during the study period. We excluded 149 infants that were born with major malformations or chromosomal anomalies, transferred to another hospital or deceased in the first 24h of admission, as per exclusion criteria. Hence, data on 131 preterm newborns was collected and analyzed; 44.3% were male, at a median 27 (23–33) weeks’ gestation, with a mean birthweight of 794.58 (±149.37) g, of which 23.7% were SGA. The overall demographic, prenatal and delivery room data are synthesized in Table 1.
Demographic, prenatal and delivery room data of the study population.
| 2005–2009 (n=56) | 2010–2015 (n=75) | p | |
|---|---|---|---|
| Gender, % | |||
| Male | 37.5 | 49.3 | 0.177a |
| Female | 62.5 | 50.7 | |
| Gestational age (weeks), median (min-max) | 28 (23–33) | 27 (24–31) | 0.052c |
| Birth weight (g), mean (±SD) | 782.86 (±143.71) | 803.33 (±153.84) | 0.440d |
| Small for gestational age, % | 32.1 | 17.3 | <0.05a |
| Maternal characteristics | |||
| Age (years), mean (±SD) | 29.79 (±5.752) | 32.09 (±5.926) | <0.05d |
| Higher education, %e | 39.2 | 63.8 | <0.05a |
| Employed, %e | 76.4 | 84.5 | 0.248a |
| Body mass index, % | |||
| Underweight | 2.2 | 0.0 | 0.096b |
| Normal | 17.8 | 12.2 | |
| Overweight | 26.7 | 49.0 | |
| Obese | 53.3 | 38.8 | |
| Pregnancy | |||
| Previous pregnancies, % | 42.9 | 44.0 | 0.896a |
| Previous births, % | 66.7 | 60.6 | 0.640a |
| Multiple births, % | 35.7 | 26.7 | 0.266a |
| Corticotherapy, % | 87.5 | 96.0 | 0.097b |
| Full cyclee | 72.9 | 66.2 | 0.440a |
| Toxic agents’ consumptionf, % | 10 | 12.0 | 0.346a |
| Infection, %e | 14.3 | 27.0 | 0.080a |
| Clinical chorioamnionitise | 0.0 | 50.0 | 0.999b |
| Medication, % | 57.1 | 52.0 | 0.559a |
| Maternal diabetes, % | 1.8 | 0.0 | 0.431b |
| Gestational diabetes, %e | 30.4 | 16.2 | 0.055a |
| Maternal hypertension, %e | 12.5 | 9.6 | 0.598a |
| Pre-eclampsia, %e | 21.4 | 25.0 | 0.636a |
| Eclampsia, % | 1.8 | 0.0 | 0.431b |
| HELLP syndrome, %e | 3.6 | 6.8 | 0.698b |
| Placental abruption, %e | 7.1 | 9.6 | 0.622b |
| Feto-fetal transfusion, %e | 9.1 | 2.7 | 0.133b |
| Abnormal ultrassonographic umbilical flow, %e | 33.3 | 39.2 | 0.505a |
| Placental evaluation, % | |||
| Histological chorioamnionitise | 35.2 | 53.3 | <0.05a |
| Grade 1e | 31.6 | 23.7 | 0.760a |
| Grade 2e | 42.1 | 42.1 | |
| Grade 3e | 26.3 | 34.2 | |
| Funisitis and/or vasculitise | 61.1 | 54.7 | 0.465a |
| Hemorrhagee | 25.9 | 26.7 | 0.925a |
| Type of delivery, % | |||
| Vaginal | 26.8 | 24.0 | 0.716a |
| Cesarean-section | 73.2 | 76.0 | |
| Cesarean with labore | 62.5 | 49.2 | 0.341a |
| Prolonged rupture of membranes (≥18h), %e | 7.8 | 8.3 | 0.999b |
| Antibiotics, %e | 22.2 | 53.2 | <0.05b |
| Apgar (<7), % | |||
| 1st minute | 64.3 | 64.0 | 0.973a |
| 5th minute | 33.9 | 25.3 | 0.284a |
| Anemia, % | 10.7 | 4.0 | 0.170b |
| Acidosis (pH≤7,20), %e | 34.6 | 13.9 | <0.05a |
| Early surfactant (≤30min)e | 36.8 | 50.0 | 0.205a |
| Resuscitation, n% | 100.0 | 89.3 | <0.05b |
| Oxygen, %e | 57.1 | 70.4 | 0.120a |
| FiO2, median (min–max) | 0.55 (0.29–1.00) | 0.40 (0.25–1.00) | 0.197c |
| Endotracheal tube, %e | 69.6 | 67.2 | 0.769a |
| Facial mask, %e | 17.9 | 41.8 | <0.05a |
| Adrenalin, %e | 1.8 | 4.5 | 0.625a |
| Cardiac compressions, %e | 1.8 | 1.5 | 0.999b |
| Early CPAP, %e | 23.2 | 32.9 | 0.234a |
When both epochs are considered together, trends in maternal data reflect, since 2010, a predominance of both older age (32.09 years old [±5.926], p<0.05) and higher education (63.8%, p<0.05), with no significant variation concerning employment or weight. Trends in other variables regarding pregnancy were not statistically significant. Antenatal steroids were administered to most women (92.4%), 69.0% of which with a full cycle. Histological chorioamnionitis’ incidence doubled in the second epoch reaching 40 cases (53.3%, p<0.05). However, no significant variations were documented in the incidence of funisitis and/or vasculitis and placental hemorrhage.
Delivery roomThe most prevalent type of delivery was cesarean-section (74.8%). A significant rise in antibiotics’ use during delivery was noted from 4 (22.2%) until 2009, to 33 (53.2%) after 2010 (p<0.05). There were no significant trends in Apgar score, anemia and early surfactant administration in the two time frames. Acidosis dropped to 13.9%, (p<0.05) and the need for resuscitation dropped from 100% to 89.3% (p<0.05) in the second period. Oxygen therapy (64.6%) and ventilation with endotracheal tube (ETT) (68.3%) were the most prevalent practices in resuscitation without a significant difference between both epochs. The use of facial mask with T rose from 17.9% to 41.8%, p<0.05. No significant variations were observed in the use of adrenaline and early CPAP or the rate of cardiac compressions.
VentilationTable 2 illustrates overall ventilation data.
Ventilation data of the study population.
| 2005–2009 (n=56) | 2010–2015 (n=75) | p | |
|---|---|---|---|
| Oxygen (days), median (min–max) | 26 (1–145) | 13.5 (1–191) | 0.243c |
| Maximum FiO2, median (min–max) | 0.7 (0.24–1) | 0.6 (0.25–1) | 0.185c |
| NIMV exclusive, % | 19.6 | 22.7 | 0.501a |
| nCPAP, %e | 100 | 100 | 0.999a |
| Days, median (min–max) | 9 (2–73) | 26 (1–49) | 0.824c |
| Bilevel CPAP, %e | 0.0 | 70.6 | <0.05b |
| Days, median (min–max) | NA | 7 (1–24) | – |
| NIMV after IMV, % | 73.2 | 84.0 | 0.131a |
| nCPAP, % | 75.6 | 69.8 | 0.521a |
| Days, mean (±SD) | 26.39 (±17.291) | 31.75 (±16.805) | 0.183d |
| Bilevel CPAP, % | 14.6 | 57.1 | <0.05a |
| Days, median (min–max) | 2 (1–13) | 8.5 (1–30) | <0.05c |
| IMV, % | 80.4 | 77.3 | 0.676a |
| Days, median (min–max) | 9 (1–140) | 9 (1–90) | 0.661c |
| Conventional ventilation, % | 100.0 | 98.3 | 0.999b |
| Days, median (min–max) | 8 (1–140) | 9 (1–90) | 0.414c |
| SIMV, %e | 78.8 | 12.3 | <0.05a |
| Days, median (min–max) | 3 (1–34) | 2 (1–10) | 0.083c |
| SIPPV, %e | 60.0 | 98.2 | <0.05b |
| Days, median (min–max) | 4.5 (1–38) | 9.5 (1–90) | 0.094c |
| PSV, %e | 12.8 | 17.2 | 0.555a |
| Days, median (min–max) | 6 (4–7) | 2.5 (1–14) | 0.112c |
| IMV with VG, % | 17.8 | 86.2 | <0.05a |
| Days, median (min–max) | 13.5 (3–23) | 8.5 (1–88) | 0.846c |
| HFOV, % | 13.3 | 10.3 | 0.639a |
| Days, median (min–max) | 14 (3–20) | 6.5 (1–23) | 0.792c |
Missing values present affecting percentage calculations.
NIMV, non-invasive mechanical ventilation; nCPAP, nasal continuous positive airway pressure; IMV, invasive mechanical ventilation; SIMV, synchronized intermittent mandatory ventilation; SIPPV, synchronized intermittent positive pressure ventilation; PSV, pressure support ventilation; VG, volume guarantee; HFOV, high frequency oscillatory ventilation.
There were no significant tendencies toward oxygen supply, in either number of days or regarding maximum FiO2.
Non-invasive mechanical ventilation (NIMV) was performed exclusively in a minority (21.4%) of patients, most frequently following invasive mechanical ventilation (IMV) (79.4%). The use of bilevel CPAP in both these situations (NIMV exclusively or following IMV) was significant, reaching 70.6% (p<0.05) in the former and 57.1% (p<0.05) in the latter, after 2010.
A total of 78.6% patients were subject to IMV, 99.0% of which underwent conventional ventilation. Even though trends in conventional ventilation (SIMV+SIPPV+PSV) have not changed significantly, the use of SIMV had a major reduction to 12.3% (p<0.05) while SIPPV became the mode of ventilation in 98.2% (p<0.05) of cases. The addition of VG to conventional ventilation experienced a major escalation (p<0.05) from 17.8% in the first epoch, to 86.2% in the late period.
MorbidityBPD, as our major outcome, affected 40.0% of the ELBW infants enrolled. This condition displayed a relevant decrease (p<0.05) from 50.9% until 2009, to 32.0% following 2010. A high number of infants was diagnosed with RDS (75.6%), sepsis (60.3%; of which 92.4% were late-onset) and PDA (58.1%). Pertaining PDA medical treatment (76.1%), indomethacin was solely used in 2005–2009 and replaced by ibuprofen in 2010–2015.
Other morbidities did not change significantly, except for cPVL which fell to 10.7% (p<0.05) (Table 3).
Morbidity of the study population.
| 2005–2009 (n=56) | 2010–2015 (n=75) | p | |
|---|---|---|---|
| RDS, % | 71.4 | 78.7 | 0.340a |
| Mildd | 22.6 | 32.6 | 0.559a |
| Moderated | 34.8 | 45.2 | |
| Severed | 32.3 | 32.6 | |
| Surfactant, % | 71.4 | 77.3 | 0.441a |
| Number of doses, median (min–max) | 2 (1–4) | 2 (1–5) | 0.224c |
| BPD, %d | 50.9 | 32.0 | <0.05a |
| Mild | 60.7 | 37.5 | 0.095a |
| Moderate/severe | 39.3 | 62.5 | 0.095a |
| Pneumonia, % | 7.1 | 16.0 | 0.178a |
| Acquired | 100 | 83.3 | 0.999b |
| Congenital | 0.0 | 16.7 | |
| Sepsis, % | 60.7 | 60.0 | 0.934a |
| Early onset | 14.7 | 15.6 | 0.917a |
| Late onset | 94.1 | 91.1 | 0.695b |
| Meningitis, % | 0.0 | 1.3 | 0.999b |
| PDA, %d | 50.0 | 63.8 | 0.138a |
| Medical treatmentd | 73.9 | 77.3 | 0.759a |
| Closure (days), median (min-max) | 14 (6–93) | 11 (3–99) | 0.194c |
| NEC, % | 12.5 | 8.0 | 0.394a |
| Surgery | 0.0 | 16.7 | 0.462b |
| ROP (≥grade 2), %d | 21.1 | 37.5 | 0.099a |
| Surgeryd | 75.0 | 68.4 | 0.999b |
| Periventricular venous infarction (IVH-IV), %d | 17.3 | 22.7 | 0.462a |
| Hydrocephalus (caused by IVH-III), %d | 15.4 | 17.3 | 0.771a |
| With shunt | 25.0 | 30.8 | 0.999b |
| cPVL, %d | 27.5 | 10.7 | <0.05a |
| Parenteral nutrition, % | 91.1 | 100.0 | <0.05b |
| Duration (days), median (min–max) | 24 (1–101) | 21 (2–90) | 0.769c |
| NICU length of stay (days), median (min–max) | 40.5 (2–147) | 69 (2–191) | <0.05c |
| Death, % | 35.7 | 26.7 | 0.266a |
| Days, median (min–max) | 11.5 (2–147) | 9 (2–99) | 0.779c |
| Autopsy, % | 55.0 | 45.0 | 0.527a |
Missing values present affecting percentage calculations.
RDS, respiratory distress syndrome; BPD, bronchopulmonary dysplasia; PDA, patent ductus arteriosus; NEC, necrotizing enterocolitis; ROP, retinopathy of prematurity; PVI, periventricular venous infarction; IVH, intraventricular hemorrhage, cPVL, cystic periventricular leukomalacia; NICU, neonatal intensive care unit.
Although there was a higher use of parenteral nutrition after 2010 (p<0.05), its duration did not vary significantly. Length of stay was of a median 57 (2–191) days, ranging from 40.5 (2–147) in the first period, and 69 (2–191) in the second (p<0.05). Mortality was 30.5% and did not change significantly between the two epochs.
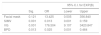
The multivariate logistic regression reported a significant reduction in BPD between the two epochs (OR=0.025; 95% CI 0.001–0.464; p=0.013), a decrease in SIMV (OR=0.013; 95% CI 0.001–0.159; p=0.001) and a generalized use of conventional ventilation with VG (OR=176.504; 95% CI 9.107–3429.847; p=0.001) (Table 4).
Multivariate analysis.
| 95% C.I. for EXP(B) | ||||
|---|---|---|---|---|
| Sig. | OR | Lower | Upper | |
| Facial mask | 0.121 | 13.425 | 0.505 | 356.840 |
| SIMV | 0.001 | 0.013 | 0.001 | 0.159 |
| VG | 0.001 | 176.504 | 9.107 | 3420.847 |
| BPD | 0.013 | 0.025 | 0.001 | 0.464 |
SIMV, synchronized intermittent mechanical ventilation; VG, volume guarantee; BPD, bronchopulmonary dysplasia.
Sig., significance; OR, odds ratio; C.I., confidence intervals.
BPD remains one of the most common complications related to prematurity. Its multifactorial pathogenesis involves several antenatal and/or postnatal risk factors.28 The premature lung, which is structurally and functionally immature, is the most susceptible to injury when exposed to certain insults. This explains why ELBW infants are at the highest risk of developing BPD.28 Given the recent advances in neonatal care, the survival of ELBW infants has significantly improved over the last decade, contributing to a rapidly increasing rate of BPD among this group.29 Nonetheless, BPD rates vary considerably among institutions, depending on neonatal practices and classification discrepancies.30,31
The major role of ventilation in the pathogenesis of BPD is related to baro- and volu-trauma. Thus, the use of non-invasive mechanical ventilation (NIMV) has been considered the optimal method of providing lung support, because it is less injurious.11 As suggested in recent guidelines,11 NIMV was widely used in our center for ELBW infants. A trend toward increased use of NIMV, both as an exclusive method of lung support and as a step-down from IMV after extubation, was noted. Moreover, the use of bilevel CPAP has increased significantly. This preference may reflect randomized controlled trials (RCTs) showing better oxygenation, respiratory rates and CO2 levels with bilevel CPAP.32 Lista et al. showed that preterm infants with RDS receiving primary support with bilevel CPAP had fewer days of respiratory support and supplemental oxygen compared to those receiving nCPAP.33 Nonetheless, there is not much evidence that conveys significant advantage of bilevel CPAP over nCPAP.11
Despite efforts to manage neonates on NIMV alone, some ELBW infants still need support with IMV. The most commonly used modes of synchronized invasive ventilation are SIMV, SIPPV and more recently PSV. Our study shows a clear shift in ventilation mode preference from SIMV, in the first epoch, to SIPPV in the second. This may be explained by recent studies suggesting a tendency toward less weaning time with SIPPV.32,34 With the assistance of every spontaneous inspiration, SIPPV also reduces breathing effort and metabolic cost of breathing compared to SIMV. However, more data is needed to assess superiority.11,34 Recent advances in ventilator technology allow the possibility of volume-targeted ventilation (VTV) strategies, such as VG. These have been developed with the purpose of accurately measuring and delivering a tidal volume leading to reduced lung damage, when compared to the traditional pressure-limited ventilation modes mentioned previously.32,35 Recent studies suggest that a generalized use of VG significantly reduced the outcomes of death, BPD, duration of ventilation, cPVL and PVI, which reflects our center's data.32,35
There were also important shifts in approach to resuscitation (oxygen exposure, room temperature, method of applying positive pressure ventilation, among others) that could influence RDS and explain the reduction in BPD observed.
Given our center's adherence to the most up-to-date guidelines, the significant reduction in the rate of BPD and cPVL registered was expected. We have adopted a far more cautious approach to ventilatory support, privileging NIMV over IMV, whenever possible, and adopting modes of invasive ventilation that cause less damage to the premature lung. Furthermore, improvements in prenatal care, delivery room stabilization, respiratory support and surfactant administration have also contributed to the observed outcomes.
This study has important strengths. Firstly, it is the first study in Portugal that comprises the most recent and comprehensive report on ventilatory practices in ELBW infants in a tertiary NICU, analyzing the progression of morbidity and mortality over an eleven-year period. Secondly, it relies on a strong database, completed by resorting to both electronic and physical medical records.
Nevertheless, two major limitations are also present. Not only is it a study based on a single center, with the limitation of not being representative of the Portuguese reality, but it is also retrospective in nature, comprising all the inherent disadvantages.
Prospective, multicenter studies with further analysis on these ventilation modes, as well as newer, less invasive strategies, are recommended.
ConclusionsChanges in our NICU's ventilatory practices, including the increased use of bilevel CPAP and a shift from SIMV to SIPPV, along with the generalized addition of VG to conventional ventilation, over the last 11 years, led to a decrease in BPD and cPVL. These results are in accordance with the most recent published guidelines.
Conflicts of interestThe authors report no conflicts of interest.