A 65-year-old woman presented with mild dysphagia, weight loss and intermittent palpitation. Chest radiograph revealed a large opacity in the right lower lung field. Subsequent CT scan showed a large posterior mediastinal lipoma extending from the level of the aortic arch to the thoracoabdominal junction. After thoracoscopic resection, the patient's dysphagia and palpitation were resolved. After a follow-up of 2 years, the patient has had no evidence of recurrence.
Uma mulher com 65 anos apresentou-se com disfagia ligeira, perda de peso e palpitações intermitentes. A radiografia do tórax revelou uma grande opacidade no campo inferior do pulmão direito. A tomografia computorizada mostrou um lipoma mediastínico de localização posterior estendendo-se desde o nível do arco aórtico à junção tóraco-abdominal. Após ressecção toracoscópica, a disfagia e as palpitações da doente foram solucionadas. Após um acompanhamento de 2 anos, a doente não teve qualquer evidência de recorrência.
Lipoma is a common neoplasm, but it is rare in the mediastinum. An extremely large and symptomatic lipoma in the posterior mediastinum is even more rare.1 We here report an unusual case of huge posterior mediastinal lipoma causing dysphagia and palpitation.
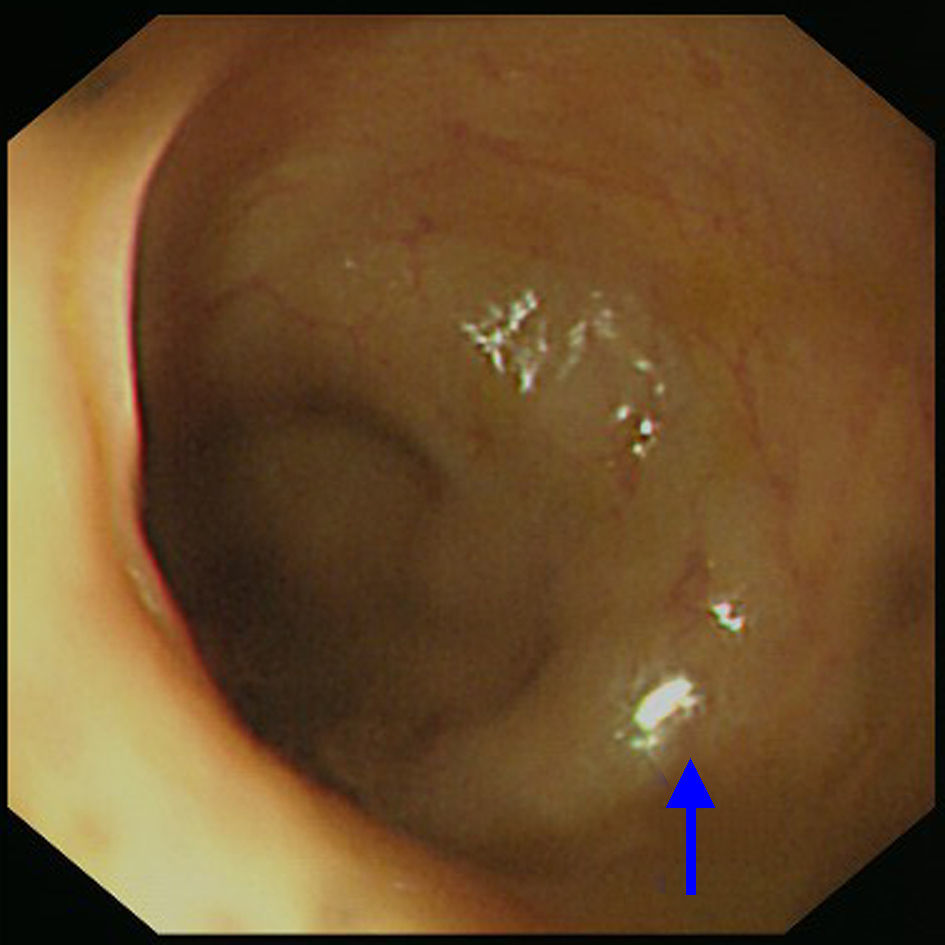
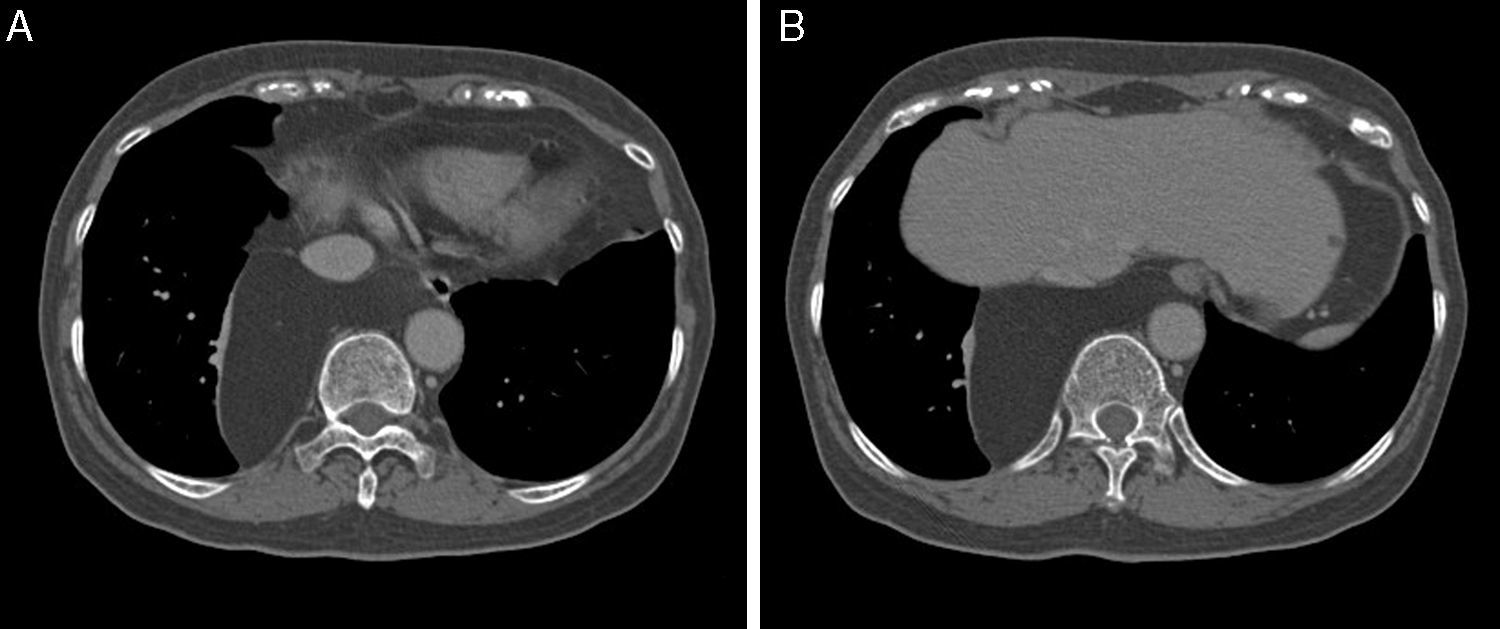
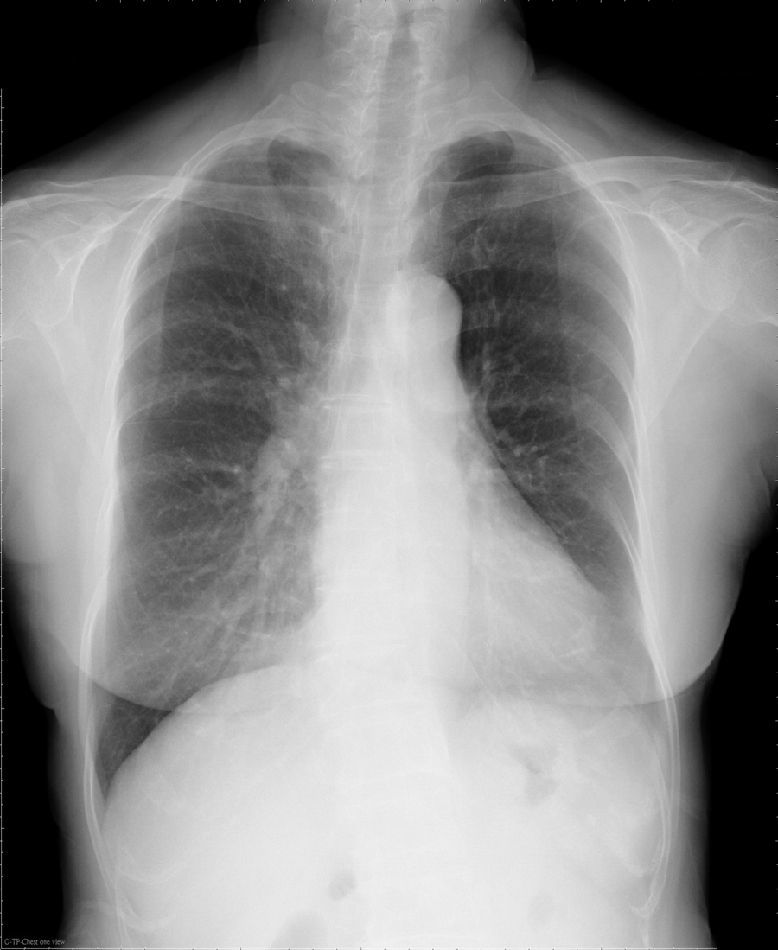
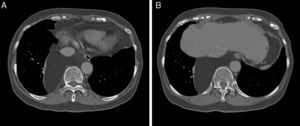
CaseA 65-year-old woman with an unremarkable medical history presented with intermittent dysphagia, which she reported had been causing a problem for approximately 1 year. The patient described a condition in which the passage of food took longer in the chest region, resulting in discomfort. Over time, the symptoms had worsened, and she had lost approximately 2kg in the previous 6 months. She finally sought medical attention in the outpatient department of our hospital. The initial physical examination findings were normal, except for an unexplained sinus tachycardia (an intermittent heartbeat of approximately 110 beats per minute). A subsequent esophagogram revealed a normal contour of the esophagus and the transit time was normal. Because the symptoms persisted and there was no sign of spontaneous regression, she underwent examination of the upper gastrointestinal tract by endoscopy. This did not provide any evidence of mucosal lesion, but the gastroenterologist did report an abnormal submucosal elevation in the lower third of the esophagus, approximately 2–3cm proximal to the esophagogastric junction (Fig. 1). Chest X-ray revealed a huge ovoid opacity in the right lower lung region adjacent to the mediastinum (Fig. 2). Computed tomographic scan indicated an enormous, low-density neoplasm in the posterior mediastinum, with a slight displacement of the esophagus (Fig. 3A), liver and inferior vena cava (Fig. 3B). Heart ultrasound revealed minimal right atrial and ventricular compression.
Chest radiograph showed one very large ovoid and well-demarcated opacity in right lower lung field. The silhouette sign is negative because the tumor margin can be differentiated from both the right heart border and diaphragm dome, indicating that the location of tumor is in the posterior mediastinum.
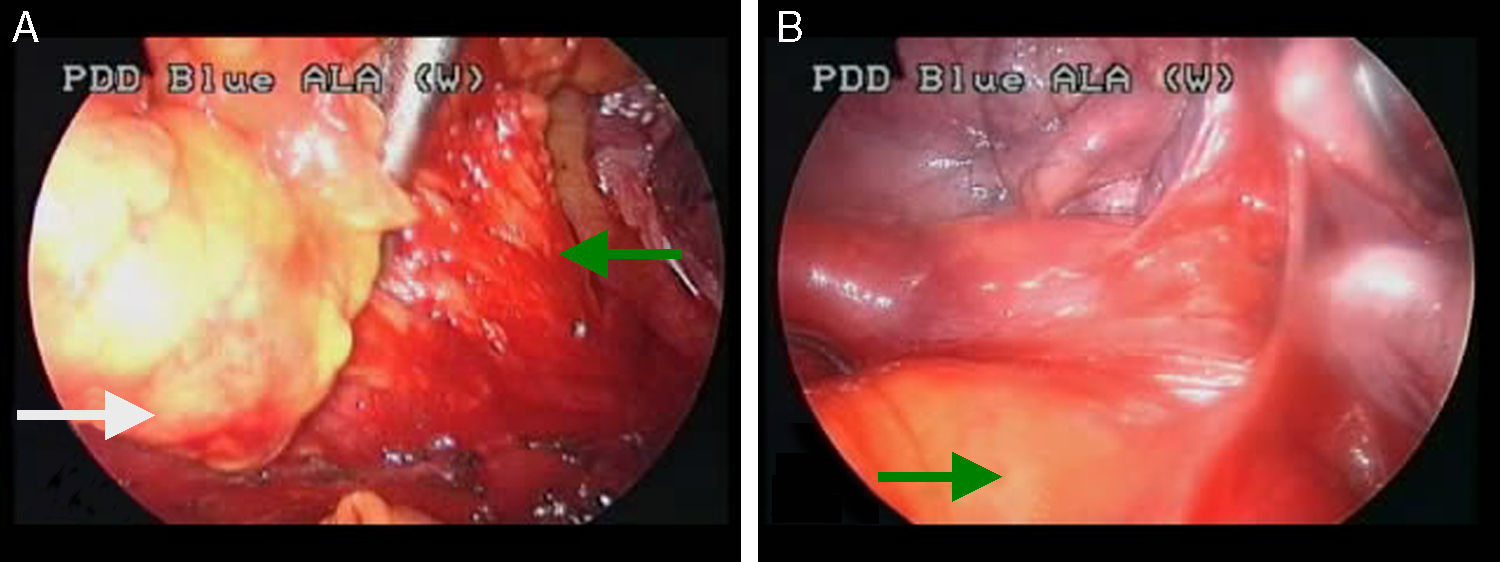
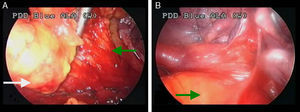
She was then surgically treated based on the diagnosis of a symptomatic, fat-containing neoplasm. She underwent thoracoscopic excision of the tumor. The approach was through a two-port thoracoscopic method, including one incision of 1.5cm and another of 2.5cm. The 1.5cm incision provided adequate visualization with a rigid endoscope 10.5mm in diameter. The larger incision gave working space for all of the instruments and the removal of the specimen. During thoracoscopic dissection, we found the tumor firmly attached to the pericardium, along with pericardial fat and the phrenic nerve (Fig. 4A), and there was some adhesion to the visceral pleura of the lung (Fig. 4B). The tumor size was 20cm×8cm×10cm. The tumor did not extend into the abdomen and was confined to the intrathoracic location. After complete resection of the lesion, an endo-bag was placed in the pleural space and then the specimen was put into the plastic bag before extraction from the pleural cavity. This method was used to prevent seeding of the tumor cells when the specimen was removed. Although enormous in size, the neoplasm was essentially soft and therefore could be safely extracted in a bag through a 2.5cm port incision. After complete resection, more than 3000ml of distilled water was used to irrigate the pleural space in order to eradicate any tumor cells which might have broken free during the surgical procedure. Any such free tumor cells would swell and then rupture in the distilled water. Three days after surgery, the chest tube was removed and she was discharged the following day.
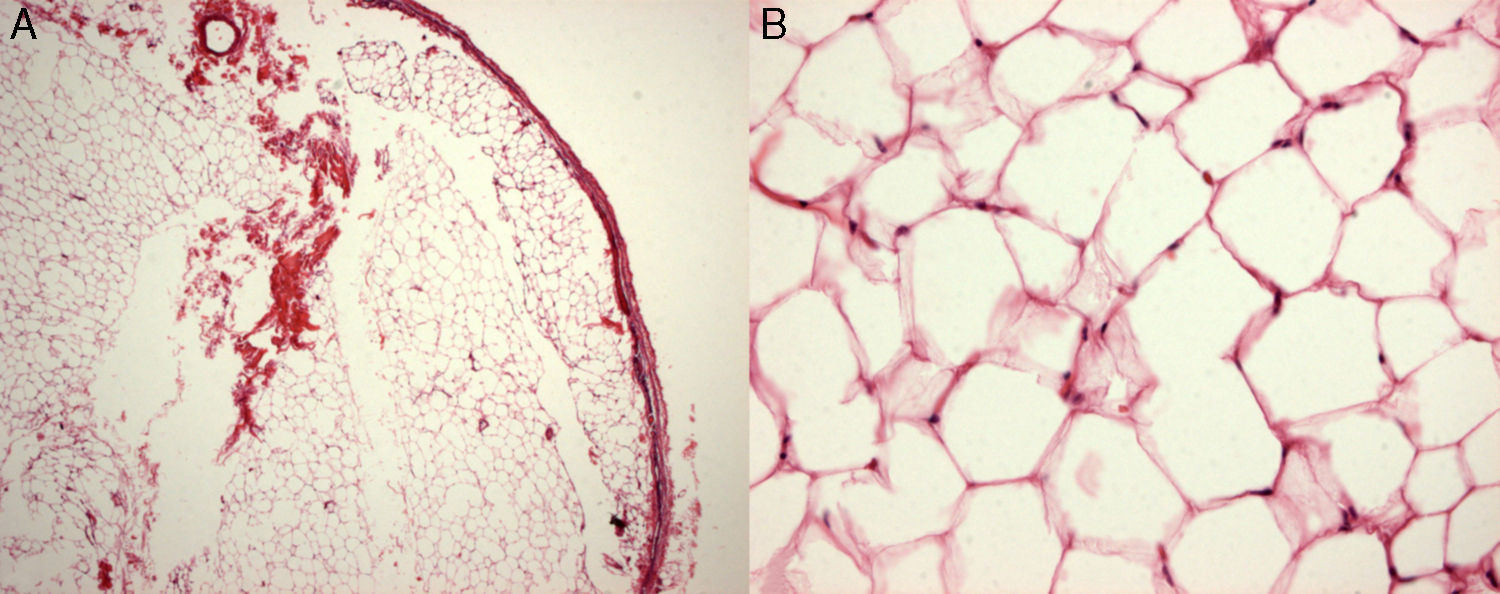
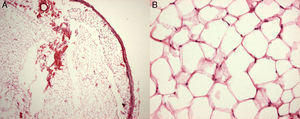
Histological examination showed the tumor to be composed of mature adipocytes, with the capsule intact. There were intervening fibrous bands, indicating this tumor to be a variant of a fibrolipoma. There was no evidence of malignancy (Fig. 5A and B). Her symptoms of dysphagia and prior unexplained sinus tachycardia improved after the operation. During a follow-up of more than 2 years, the patient has had no recurrence (Fig. 6).
A lipoma may develop in any part of the body. Mediastinal lipoma is rare and usually found in the anterior mediastinum.1 An enormous lipoma in posterior mediastinum was reported in a 50-year-old man which was found incidentally on a chest radiograph, and he was successfully treated by excision via open thoracotomy.2 Such a tumor typically grows very slowly, and the presenting symptoms are often related to a direct compression effect. The symptoms may include dysphagia, retrosternal compression and arrhythmia.1–3 In this case, however, a heart ultrasound did not find any significant abnormality. The patient's tachycardia was resolved after complete resection of the lesion. The most likely explanation for this result would be the direct effect of the tumor mass on the adjacent organs, including the esophagus and heart as well as the inferior vena cava. Liposarcoma is one of the diagnostic challenges in such cases, because it has similar imaging characteristics. When there are trabeculates, intracapsular soft tissue growth, thick septa, the presence of nodular and/or globular non-adipose mass-like areas and a decreased percentage of fat composition, the likelihood of malignancy is high. If the soft tissue involvement is difficult to determine on CT scan alone, magnetic resonance imaging (MRI) is frequently helpful. MRI provides an 83% rate of accuracy in diagnosing well-circumscribed liposarcomas.4 Although percutaneous needle biopsy is feasible in most cases, there are two reasons not to perform a percutaneous needle biopsy. The first reason is a symptomatic lipogenic tumor for which surgical resection is indicated. The second is when the lesion is very large, since a normal biopsy result might not be sufficient to exclude a sarcomatous lesion. Potential treatment options include liposuction, steroid injection and surgical resection. When malignancy cannot be ruled out, complete resection is required. Complete resection, in such circumstances, may assist in the differential diagnosis as well as cure the disease.
Thoracoscopic resection, in such cases, is generally considered to be a safe approach. When video-assisted thoracoscopic surgery is indicated for the resection of an enormous tumor, there are two important aspects to keep in mind. The first one is the nature of the neoplasm. If direct invasion of any vital organs is strongly suspected, such a procedure may carry additional risks and a change to open thoracotomy may be required. The second is the firmness as well as the size of the neoplasm. When the tumor is very soft, a small incision is sufficient for extraction even if the overall size of the neoplasm is very large. In the case reported here, the tumor was enormous, but also very soft. One 2.5-cm incision was therefore sufficient for extraction. A large incision for the extraction was thus not needed. However, if the tumor is solid as well as large, an extensive thoracotomy incision for extraction is unavoidable. Although lipoma is a benign neoplasm, it may easily recur in the surgically treated location if there is a residual lesion. Long-term follow-up is therefore mandatory in all cases.5,6