We aimed (1) to measure asthma control using a structure-questionnaire and patient self-perception of asthma-control in the Portuguese National Asthma Survey (INAsma) and (2) to study the relationship between asthma control and asthma-related quality of life.
MethodsWe analyze data of asthma patients from a cross-sectional, nationwide telephone interview study – INAsma. Controlled asthma was defined as CARAT global score >24 or CARAT lower airways score ≥16. Mini-AQLQ was used to measure quality of life.
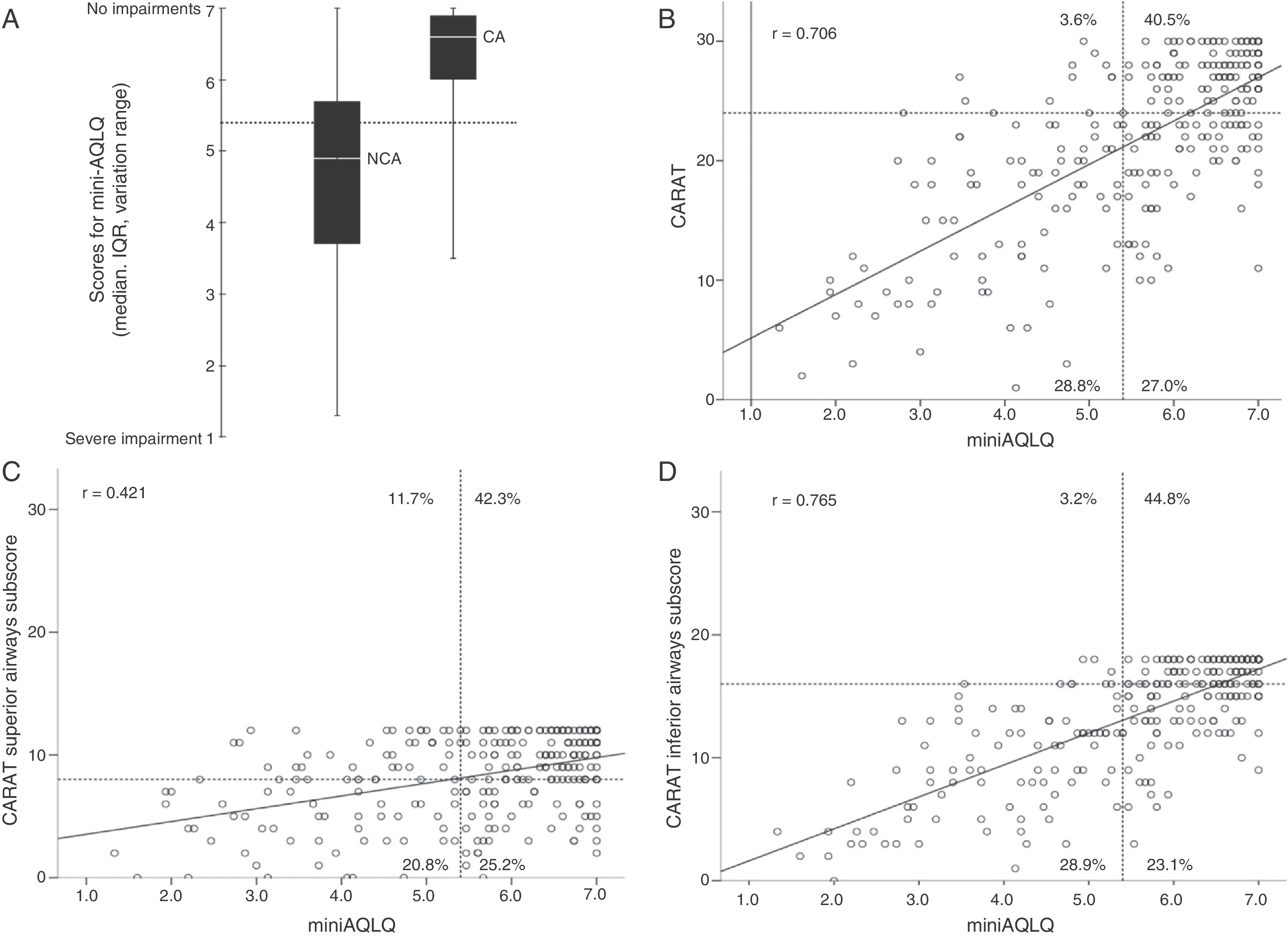
ResultsTwo hundred and seven (56.9% [95%CI: 51.8–62.0]) of the 364 patients had controlled asthma. Most patients with non-controlled asthma (88%) perceived their disease as controlled. Patients with controlled asthma presented higher mini-AQLQ scores (median, P25–P75; 6.6, 6.0–6.9) than those with non-controlled asthma (4.9, 3.7–5.7) (p < 0.001) and a significant positive correlation between CARAT and mini-AQLQ scores was observed (r = 0.706; p < 0.001).
ConclusionMore than half of the Portuguese patients presented controlled asthma and showed significantly better asthma-related quality of life. Almost 9 out of 10 patients with non-controlled disease have poor perception of their asthma control, which may hinder them from seeking better asthma control.
Proper asthma therapy and education reduces the socioeconomic burden of asthma and improves patients’ quality of life.1 However, the proportion of patients achieving asthma control remains low worldwide without substantial improvement in recent years.2, 3, 4, 5, 6
The Portuguese National Program for Asthma Control conducted by the Directorate-General of Health between 2005 and 2010, aimed to increase the proportion of asthma patients with controlled disease, and to decrease the personal and community burden of the disease.
At the end of this program, in 2010, we conducted the first Portuguese National Asthma Survey – Inquérito Nacional sobre Asma (INAsma), which consisted of two phases. In the first phase, aiming to evaluate asthma prevalence, we estimated that 7% of the Portuguese population had current asthma.7 In the second phase we focused on asthma patients addressing disease control.
We aim to measure asthma control using a structure-questionnaire and patient self-perception of asthma-control in the Portuguese National Asthma Survey (INAsma) and to study the relation of asthma control with asthma-related quality of life (ARQoL).
MethodsThe INAsma was a cross-sectional, nationwide, telephone interview study. Sample size calculations details have been previously reported.7 All the participants identified with possible asthma in the first phase of the survey were eligible for participation in the second phase. Detailed information is provided in the Supplementary Material. The study was approved by the Hospital Ethics Committee of Hospital de São João (Porto, Portugal).
Current asthma was defined as self-report of asthma and one of the following: at least one medical appointment due to asthma in the last 12 months; current use of asthma medication; asthma symptoms in the last 12 months (wheeze, cough, breathlessness or sputum production without a cold or respiratory infection).
Asthma control was defined based on Control of Allergic Rhinitis and Asthma Test (CARAT) scores.8, 9 Asthma was considered controlled for CARAT global score above 24 or CARAT lower airways score of 16 or above. Self-perception of asthma control was evaluated by the answer to the question “Do you believe your asthma was well controlled in the last 4 weeks?”. Additional questions were included assessing socio-educational variables.
ARQoL was measured by mini-Asthma Quality of Life Questionnaire (mini-AQLQ)10 with a cut-off value of 5.4 set according to a previous study in northern Portugal.11
Statistical analyses were performed using IBM SPSS Statistics v21 (2012 SPSS Inc., IBM Company, Chicago, US). Categorical variables were described with absolute frequencies, proportions and 95% Confidence Interval (95% CI) and continuous variables were described with measures of central tendency and dispersion as appropriate. Correlation between CARAT and mini-AQLQ scores was tested with Pearson's Correlation Coefficient, with a p-value of <0.05 considered as statistically significant.
ResultsOf the 707 participants identified with possible asthma in the Phase 1, 559 agreed to participate in Phase 2, from which 405 had current asthma as described in the online supplement (Fig. S1). Sufficient data to define asthma control were available for 364 patients. Participants’ characteristics are summarized in Table 1.
Table 1. Socio-demographic characteristics of the participants with classification for asthma control by asthma control status and patient perception of control and asthma related quality of life.
| Total (n = 364) | Controlled asthma | Patient perception of control | ARQoL cut-off value | ||||
| Yes (n = 207) | No (n = 157) | Controlled (n = 338) | Non-controlled (n = 21) | Above (n = 188) | Below (n = 89) | ||
| Sex, n (%) | |||||||
| Male | 155 (42.6) | 111 (71.6) | 44 (28.4) | 146 (96.1) | 6 (3.9) | 79 (81.4) | 18 (18.6) |
| Female | 209 (57.4) | 96 (45.9) | 113 (54.1) | 192 (92.8) | 15 (7.2) | 109 (60.6) | 71 (39.4) |
| Age groups, n (%) | |||||||
| <18 years old | 87 (23.9) | 59 (67.8) | 28 (32.2) | 82 (96.0) | 4 (4.7) | 0 (0.0) | 0 (0.0) |
| 18–64 years old | 177 (48.6) | 112 (63.3) | 65 (36.7) | 168 (96.0) | 7 (4.0) | 132 (74.6) | 45 (25.4) |
| >64 years old | 100 (27.5) | 36 (6.0) | 64 (64.0) | 88 (89.8) | 10 (10.2) | 56 (56.0) | 44 (44.0) |
| Education levela , n (%) | |||||||
| <9 years | 240 (65.9) | 120 (50.0) | 120 (50.0) | 220 (92.4) | 18 (7.6) | 92 (57.5) | 68 (42.5) |
| 9–12 years | 83 (22.8) | 57 (68.7) | 26 (31.3) | 80 (98.8) | 1 (1.2) | 60 (78.9) | 16 (21.1) |
| >12 years | 41 (11.3) | 30 (73.2) | 11 (26.8) | 38 (95.0) | 2 (5.0) | 36 (87.8) | 5 (12.2) |
| SESb , n (%) | |||||||
| Low | 59 (16.3) | 18 (30.5) | 41 (69.5) | 51 (87.9) | 7 (5.9) | 29 (49.2) | 30 (50.8) |
| Medium low | 222 (61.2) | 127 (57.2) | 95 (42.8) | 211 (95.9) | 9 (4.1) | 116 (69.5) | 51 (30.5) |
| Medium high | 49 (13.5) | 35 (71.4) | 14 (28.6) | 44 (91.7) | 4 (8.3) | 27 (84.8) | 5 (15.6) |
| High | 33 (9.1) | 27 (81.8) | 6 (18.2) | 31 (96.9) | 1 (3.1) | 15 (83.3) | 3 (16.7) |
| Smoking status, n (%) | |||||||
| Non-smoker | 274 (75.3) | 153 (55.8) | 121 (44.2) | 255 (93.8) | 17 (6.3) | 121 (64.0) | 68 (36.0) |
| Ex-smoker | 53 (14.6) | 33 (62.3) | 20 (37.7) | 46 (92.0) | 4 (8.0) | 39 (73.6) | 14 (26.4) |
| Current smoker | 37 (10.2) | 21 (56.8) | 16 (43.2) | 37 (100.0) | 0 (0.0) | 28 (80.0) | 7 (20.0) |
| Controlled asthma, n (%) | |||||||
| Yes | 207 (56.9) | – | – | 201 (98.5) | 3 (1.5) | 137 (92.6) | 11 (7.4) |
| No | 157 (43.1) | – | – | 137 (88.4) | 18 (85.7) | 51 (39.5) | 78 (60.5) |
| Patient perception of control, n (%) | |||||||
| Controlled | 338 (94.2) | 201 (59.5) | 137 (40.5) | – | – | 181 (70.7) | 75 (29.3) |
| Not controlled | 21 (5.8) | 3 (14.3) | 18 (85.7) | – | – | 3 (17.6) | 14 (82.4) |
Asthma Related Quality of Life (ARQoL) cut-off value of 5.4.
a A total of 60 (2.7%) participants were preschoolers (not shown) – Data retrieved from 1st phase of INAsma.
b Socioeconomic Status was categorized in high (A social class), medium high (B social class), medium low (C social classes) and low (D social class) based on occupation and school education of the person who contributes more for the household income – Data retrieved from 1st phase of INAsma.
According to the patients’ answers to CARAT, the most frequent symptoms were related to upper airways with 24.9% (n = 90) and 21.4% (n = 78) of the patients answering “Always”, to sneezing and itchy nose, respectively (Fig. S2). The less common symptom reported was nocturnal awakening with 69.5% (n = 253) of the patients answering “Never”.
Asthma was controlled in 56.9% [95%CI, 51.8–62.0] (n = 207) of the patients (Table 1). Regarding patient self-perception of control, 94% (n = 338) reported having their asthma controlled (Table 1). Among the non-controlled patients 88.4% (n = 137) perceived their asthma as controlled (Table 1, Fig. S3).
Controlled patients had higher mini-AQLQ scores than the non-controlled (median, P25–P75; 6.6, 6.0–6.9 and 4.9, 3.7–5.7, respectively; p < 0.001) (Figure 1A). A significant positive correlation between CARAT and mini-AQLQ scores was observed (r = 0.706; p < 0.001, Figure 1B).
Figure 1. Relationship between CARAT and mini-AQLQ scores (n = 274); (A) ARQoL by asthma control groups; Scatterplots show the correlation between (B) CARAT global score and ARQoL; (C) CARAT superior airways subscore and ARQoL; (D) CARAT inferior airways subscore and ARQoL. In A the horizontal line represents the Mini-AQLQ cut-off of 5.4 based on previous study; 11 NCA: non-controlled asthma; CA: Controlled asthma. In (B, C and D) the vertical lines represent the Mini-AQLQ cut-off of 5.4 11 and the horizontal lines represent the CARAT cut-offs; 9 (B) global score cut-off of 24; (C) superior airways subscore cut-off of 8 and (D) the CARAT inferior subscore cut-off of 16. The scatterplots are divided into four quadrants, the inferior left corresponds to participants with non-controlled disease and more impairments and the upper right to participants with controlled disease and less impairments.
DiscussionWe report the first nationwide results on asthma control in Portugal with more than half (57%) of the patients presenting controlled asthma. A significant positive correlation was found between CARAT and mini-AQLQ, indicating that patients with controlled asthma had significant better ARQoL comparing to patients with non-controlled asthma. However, most patients (88%) with non-controlled asthma perceived their asthma as controlled.
The proportion of asthma control was in accordance with recent studies in other countries.4 In 2010, the European National Health and Wellness Survey5 estimated a global proportion of non-controlled asthma of 53.5% across five European countries. Similarly, the International Asthma Patient Insight Research (INSPIRE) study4 found a worldwide proportion of non-controlled asthma of 51%. In Portugal, a study of asthma patients from one Allergy unit concluded that 57% had partially or complete asthma control when assessed with ACT.12
A strong positive correlation was observed between asthma control assessed by CARAT and ARQoL assessed by Mini-AQLQ. This correlation was similar to previous reports using other asthma control questionnaires11, 13, 14 but had not been reported with CARAT questionnaire.
Most of the participants with non-controlled asthma perceived their disease as controlled. This is very similar to the data from the Asthma Insights and Reality in Europe survey.3 Also in the INSPIRE study,4 patient perception of asthma control was strikingly different from that based on symptoms assessment. These data suggest that patients, especially those with poor control, continue to have very low expectations regarding asthma outcomes. Clinical studies are warranted on the relation between asthma control and patient-self perception of control.
The main strength of the present study is that INAsma is the first Portuguese study to include patients from the general population from all municipalities and all age groups.7 Some limitations are inherent to a landline telephone-based interview study, especially with the recent shift from landline telephones to cellphones. Other limitation is the potential for confusion as the definition of control may have been influenced by the rhinitis subscore. However, we compared the results of patients with and without associated rhinitis and there were no differences in the proportion of patients with controlled asthma, in perceptions of asthma control and in the correlation between asthma control and ARQoL (data not shown). Moreover, the CARAT superior airways subscore seems not to have affected the correlation between CARAT total score and miniARQLQ (Figure 1C).
In conclusion, more than half of the Portuguese asthma patients have their disease controlled and these have significantly better asthma-related quality of life. Poor perception of control seems to be an obstacle to achieving better disease control as almost 9 out of 10 patients with non-controlled disease had poor perception of their asthma control. The objective assessment of asthma control using validated tools may help patients to increase their expectations regarding asthma outcomes.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Acknowledgements
The Portuguese National Asthma Survey – Inquérito Nacional sobre Asma (INAsma) was conducted by the Center for Health Technology and Services Research (CINTESIS) in collaboration with Sociedade Portuguesa de Pneumologia, by appointment of the Portuguese Health Directorate.
The work presented in this short communication was partially funded by FEDER funds through COMPETE (Programa Operacional Factores de Competitividade) and by National funds through a FCT (Fundação para a Ciência e a Tecnologia) project with reference “PTDC/SAU-SAP/119192/2010”.
Appendix A. Supplementary dataSupplementary material associated with this article can be found in the online version available at http://doi.org/10.1016/j.rppneu.2014.08.001.
Appendix A. Supplementary dataSupplementary Fig. S1. Participants Flowchart. From 559 participants 405 had current asthma and 207 had their asthma controlled.
Supplementary Fig. S2. Answers to CARAT questionnaire. Questions 1–9: dark blue “Never”; yellow “Up to 2 days per week”; orange “More than 2 days per week”; red “Almost every day or every day”. Question 10: light blue “Not taking medication”; dark blue “Never”; orange “Less than 7 days”; red “7 or more days”.
Supplementary Fig. S3. Perceived asthma control by asthma control status. From the 359 participants who answered to the question “Did you feel that your asthma was well controlled?”, 155 had non-controlled asthma and 204 had their asthma controlled, based on CARAT scores.
Received 2 May 2014
Accepted 19 August 2014
Corresponding author. jfonseca@med.up.pt